儿童幕上脑室占位性病变的影像学诊断价值
2015-10-17李美蓉李玉华
杨 飘,李美蓉,李玉华
(上海交通大学医学院附属新华医院放射科,上海 200092)
◁论著▷
儿童幕上脑室占位性病变的影像学诊断价值
杨飘,李美蓉,李玉华
(上海交通大学医学院附属新华医院放射科,上海200092)
目的:探讨儿童幕上脑室内占位性病变的影像诊断价值。方法:回顾性分析经手术病理证实的45例儿童幕上脑室占位性病变的临床及影像资料。男25例,女20例,年龄4月~13岁,中位年龄2岁。结果:脉络丛乳头状瘤16例,边缘呈颗粒状或分叶状,CT表现为稍高密度,MRI表现为T1WI呈等、低信号,T2WI等、高信号,DWI等低信号,增强后明显强化。非典型脉络丛乳头状瘤6例,1例散在斑点状钙化,2例伴脑脊液播散,2例伴周围脑组织水肿。脉络丛癌1例,呈囊实性,DWI呈高信号。毛细胞型星形细胞瘤4例,毛细胞黏液样星形细胞瘤2例,均位于三脑室,DWI稍低信号,增强明显强化。室管膜瘤2例,非典型畸胎样/横纹肌样瘤2例,室管膜下巨细胞星形细胞瘤1例,脑膜瘤1例。神经上皮囊肿10例,囊壁菲薄,囊液信号与脑脊液信号相似,增强扫描无强化。结论:儿童幕上脑室占位性病变的病理类型复杂,CT和MRI基本能反映肿瘤的特点,结合临床资料,可对大部分病例作出定性诊断。
脉络丛肿瘤;儿童;体层摄影术,X线计算机;磁共振成像
儿童幕上脑室占位性病变发病率低,病理类型复杂,目前关于儿童脑室内占位性病变的研究多集中在四脑室,而对幕上脑室内占位性病变研究较少。本文笔者回顾性分析本院45例经病理证实的儿童幕上脑室占位性病变的CT和MRI表现,旨在探讨其影像诊断价值。
1 材料与方法
1.1一般资料
搜集我院经病理证实的儿童幕上脑室占位性病变45例,其中男25例,女20例,年龄4月~13岁,中位年龄2岁。患儿临床主要表现为头痛、头晕、恶心呕吐等颅高压症状,部分患儿表现为肢体活动不利、双眼凝视、发育迟缓等。
1.2检查方法
21例行CT扫描,40例行MRI扫描。CT采用Siemens公司Somatom Definition双源CT,对比剂为Onmipaque,剂量2mL/kg。MRI采用GE公司Signa Exite 1.5T MR和Signa HDxt 3T成像系统,头颅正交线圈,平扫常规序列T1WI、T2WI,增强扫描用SET1WI,对比剂使用Gd-DTPA,剂量0.1 mmol/kg,行横断面、冠状面和矢状面扫描。不能配合检查的患儿,给予5%水合氯醛溶液(0.5mg/kg)诱导其入睡。
2 结果
脉络丛肿瘤(23例):年龄4月~7岁,12例位于侧脑室,5例位于三脑室,6例同时累及侧脑室和三脑室。脉络丛乳头状瘤16例,CT平扫均表现为稍高密度,MRI表现为T1WI呈等、低信号,T2WI呈等、高信号,DWI等低信号,增强后明显强化,边缘呈颗粒状或分叶状,2例伴有脑脊液播散。非典型脉络丛乳头状瘤6例,与脉络丛乳头状瘤相似,1例见散在斑点状钙化,2例伴脑脊液播散 (图1),2例伴周围脑组织水肿。脉络丛癌1例,位于三脑室,呈囊实性,DWI呈高信号,伴局部瘤周水肿。本组脉络丛乳头状肿瘤78%(18/23)伴有幕上脑室均大。
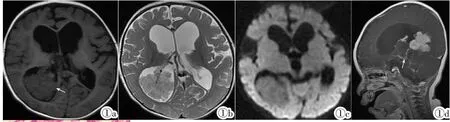
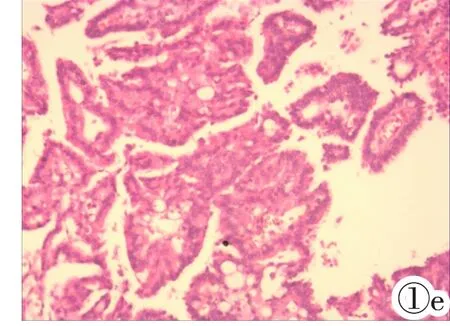
图1非典型脉络丛乳头状瘤。图1a:横断面T1WI示肿瘤位于右侧脑室三角区,边缘呈颗粒状,呈稍低信号;图1b:横断面T2WI示病灶稍高信号;图1c:DWI示肿瘤低信号;图1d:增强矢状面T1WI示肿瘤明显强化,可见非梗阻性脑积水,伴脑膜异常强化(箭头);图1e:肿瘤细胞呈乳头样排列,局部呈片状排列,细胞核具有异型性,偶见核分裂像(3~4/10HPF)。
Figure 1.Atypical choroid plexus papilloma.Figure 1a:Axial T1WI showed a lobulated,hypo-intense mass in the right lateral ventricle.Figure 1b,1c:The mass was hyper-intense on T2WI and hypo-intense on DWI.Figure 1d:Contrast-enhanced sagittal T1WI showed intense enhancement of the mass and leptomeningeal dissemination.Non-obstructive hydrocephalus was present.Figure 1e: Histopathological features included increased cellular density,papillary growth of tumor cells and brisk mitotic activity(3~4 per 10 high-power fields).
毛细胞型星形细胞瘤(4例)及毛细胞黏液样星形细胞瘤(2例):1~13岁,均位于三脑室内,均呈实性,且无明显瘤周水肿。CT平扫5例呈低密度,1例呈高低混杂密度,1例伴有边缘点线样钙化。DWI稍低信号,T1低信号,T2高信号,增强扫描5例呈明显强化(图2),1例轻度强化。
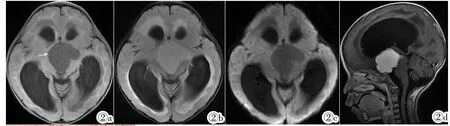
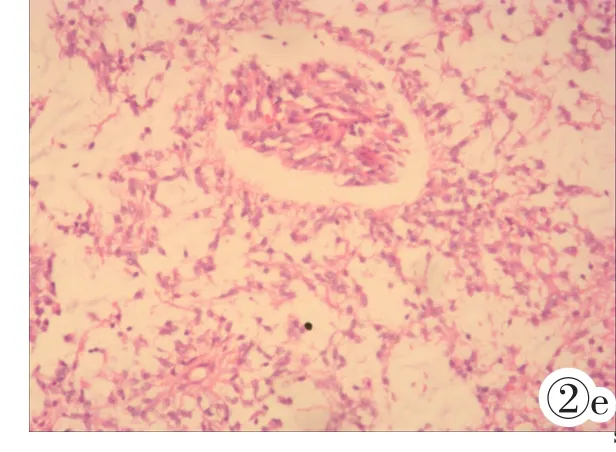
图2毛细胞黏液样星形细胞瘤。图2a:横断面T1WI示肿瘤位于第三脑室,边界清晰,呈低信号;图2b:横断面T2WI示肿瘤稍高信号;图2c:DWI见肿瘤低信号;图2d:增强矢状位T1WI示病灶明显均匀强化,伴梗阻性脑积水;图2e:在大量的黏液背景可见双极性的梭形细胞,肿瘤细胞围绕血管分布。
Figure 2.Pilomyxoid Astrocytoma.Figure 2a:Axial T1WI showed a well-defined,homogeneous,hypo-intense mass in the third ventricle.Figure 2b,2c:The mass was hyper-intense on T2WI and hypo-intense on DWI.Figure 2d:Contrast-enhanced sagittal T1WI showed intense enhancement.Obstructive hydrocephalus was present.Figure 2e:The tumor was composed of bipolar spindle cells with an angiocentric growth pattern,setting in a strikingly mucinous background.
室管膜瘤(2例):年龄4~7岁,位于侧脑室。1例间变性室管膜瘤,CT表现为囊实性肿块,实性部分呈稍高密度,MRI表现为T1低信号,T2高信号,DWI稍高信号,增强后实性部分强化明显,病灶周围脑组织部分水肿。1例室管膜瘤,DWI表现为高低混杂信号,T1呈等、低信号,T2以高信号为主,增强呈明显结节状、环形强化,周围脑实质水肿,伴幕上脑室扩大。
室管膜下巨细胞星形细胞瘤(1例):5岁,合并结节性硬化,肿瘤位于室间孔区。MRI表现为DWI等、低信号,T1等信号,T2不均匀高信号,增强呈现明显强化(图3)。
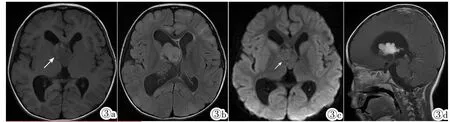
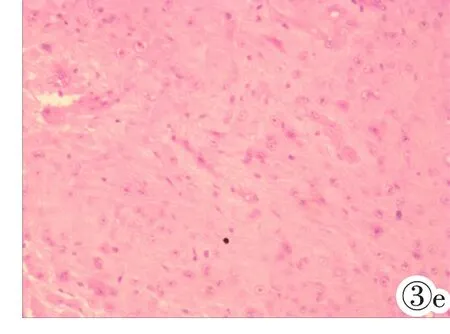
图3室管膜下巨细胞星形细胞瘤,伴结节性硬化。图3a:横断面T1WI示肿瘤位于右侧室间孔区,基本位于侧脑室内,以低信号为主,左侧颞部皮层下小病灶;图3b:横断面T2WI示肿瘤呈高信号;图3c:DWI见肿瘤呈等、低信号;图3d:增强T1WI矢状面示肿瘤明显强化;图3e:细胞胞质丰富,多核或巨核,伴节细胞样瘤细胞,核仁明显。
Figure 3.Subependymal giant cell astrocytoma with tuberous sclerosis complex.Figure 3a:Axial T1WI showed a hypo-intense mass near the foramen of Monro.Subcortical focal areas of T1hypo-intensity were noted.Figure 3b,3c:The mass was hyper-intense on T2WI and hypo-to-isointense on DWI.Figure 3d:Contrast-enhanced sagittal T1WI showed avid enhancement of the mass.Figure 3e:Histologically,there were gemistocytes and ganglioid-like cells with clear nucleolus.
非典型畸胎样/横纹肌样瘤(2例):10月~9岁,1例位于三脑室;1例位于侧脑室,累及枕叶。CT平扫呈高低混杂密度,DWI呈明显高信号,T1呈低信号,T2呈高信号,内见囊变坏死区域;1例增强呈轻度不均匀强化(图4),1例三脑室信号均匀,病灶呈明显强化,并伴有右侧额叶及中脑强化结节。2例均伴有瘤周水肿。
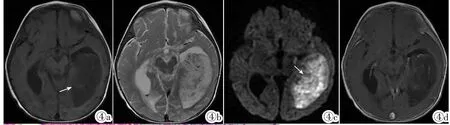
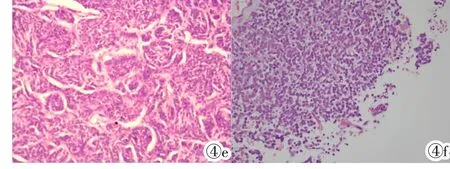
图4非典型畸胎样/横纹肌样瘤。图4a:横断面T1WI示肿块体积较大,位于左侧脑室内,呈低信号;图4b:横断面T2WI示肿块呈混杂高信号;图4c:DWI见肿块呈明显高信号;图4d:增强T1WI横断面示肿块呈轻度不均匀强化;图4e,4f:镜下见横纹肌样细胞,大量小细胞,局部见菊形团形成。
Figure4.Atypical teratoid/rhabdoidtumor. Figure 4a:Axial T1WI showed a large hypo-intense mass in the left ventricle.Figure 4b,4c:The mass was heterogeneous on T2WI and hyper-intense on DWI.Figure 4d:Contrast-enhanced T1WI showed slight enhancement.Figure 4e,4f:Histologically,the tumor contained rhabdoid cells and a large number of small cells with focal rosettes.
脑膜瘤(1例):2岁,位于左侧脑室后角,CT平扫结节状高密度,T1呈稍低信号,T2Flair呈低信号伴周边高信号,DWI呈部分高信号,增强扫描呈明显不均匀强化,脑室无明显扩大。
神经上皮囊肿(10例):男9例,女1例,年龄9月~12岁,9例位于侧脑室,囊壁菲薄,呈圆形或类圆形,77.8%(7/9)囊液信号/密度与脑脊液相似,22.2%(2/9)囊液T1WI信号略高于脑脊液,T2WI高信号,DWI上均为低信号,增强扫描无强化;1例位于三脑室,呈多囊性,大部分囊液密度/信号与脑脊液信号相似,部分囊液密度稍高于脑脊液。根据病理表现,本组包括蛛网膜囊肿7例及室管膜囊肿3例。
3 讨论
3.1幕上脑室结构特点
脑室属于脑脊液产生和循环的通路,包括室管膜、脉络丛等结构。胚胎时期,脑室由神经管脑端的室管膜上皮外翻形成,原始软蛛网膜及血管内陷参与脉络丛组织形成[1]。脑室内覆室管膜,室管膜下层主要为胶质细胞,脉络丛血供丰富,产生脑脊液。脑室内占位性病变包括起源于脑室室管膜、脉络丛上皮的病变以及原发于周围结构但肿瘤表现为脑室内的占位病变。
3.2儿童幕上脑室占位性病变的诊断及鉴别诊断
脉络丛肿瘤是儿童幕上脑室肿瘤中最常见的类型,本组占65.7%(23/35)。脉络丛肿瘤起源于脉络丛上皮,最常见于侧脑室[1],本组78%(18/23)位于侧脑室。肿瘤可分泌脑脊液,体积较大时可阻塞脑脊液通路,因而常伴有脑积水,本组78%有明显幕上脑积水。根据组织学特点,脉络丛肿瘤可分为脉络丛乳头状瘤 (WHOⅠ级)、非典型脉络丛乳头状瘤(WHOⅡ级)和脉络丛癌(WHOⅢ级)。其中,前两者可见于任何年龄组,而脉络丛癌绝大多数见于婴幼儿[2]。脉络丛乳头状瘤典型影像学表现为:边缘颗粒状或分叶状实性肿块,CT平扫呈等、高密度,MRI扫描DWI呈等低信号,T1呈等、低信号,T2呈等、高信号,增强显著强化,本组符合。非典型脉络丛乳头状瘤在本组中1/3伴周围脑组织水肿,考虑可能由于肿瘤对周围脑组织侵袭性有关,与李丽等[3]报道相似;1/3伴脑脊液播散,较脉络丛乳头状瘤的1/8发生率高,提示非典型脉络丛乳头状瘤可能更易发生脑脊液播散。脉络丛癌倾向为形态不规则肿块[4],且肿瘤内部容易发生坏死,因而在CT及MRI上更易表现为不均匀密度/信号[1]。本组1例脉络丛癌符合以上表现,并DWI呈现高信号。以往认为脉络丛肿瘤难以鉴别,我们结合本组病例认为:非典型脉络丛乳头状瘤更易发生瘤周水肿及脑脊液播散,而脉络丛癌形态不规则且囊变、坏死多见。
毛细胞型星形细胞瘤是儿童颅内常见的一种特殊类型星形细胞肿瘤,WHOⅠ级,常见于儿童和青少年。毛细胞黏液样星形细胞瘤为新近分类的肿瘤,WHOⅡ级,较毛细胞型星形细胞瘤更具有侵袭性的生物学特征[2]。两种肿瘤目前在影像学上仍然难以鉴别。三脑室毛细胞型星形细胞瘤,实质成分为主,伴或不伴有小囊变,增强后显著均匀强化,DWI等低信号以及瘤周水肿轻或无是其典型表现[5],本组符合。且毛细胞黏液样星形细胞瘤发病年龄(平均年龄22月)可能较毛细胞型星形细胞瘤(平均年龄54月)更小。
室管膜瘤起源于脑室壁的室管膜细胞,好发于儿童,四脑室常见,幕上少见。幕上室管膜瘤超过半数位于脑实质内,其余发生于脑室内,且常沿脑室壁或透明隔生长[6]。幕上室管膜瘤缺乏特征性表现。本组中2例均发生于侧脑室,呈囊实性,伴有瘤周水肿,但例数较少,缺乏代表性。
室管膜下巨细胞星形细胞瘤属于良性肿瘤,好发于20岁以下,可发生于胎儿,多发生于侧脑室孟氏孔附近,偶可发生于侧脑室体部及下角,5%累及三脑室[7]。本组1例,肿瘤基本位于侧脑内。该病是结节性硬化患者最易发生的颅内肿瘤,但已有文献报道可发生于非结节性硬化患者[8]。孟氏孔附近的室管膜下结节容易转化为室管膜下巨细胞星形细胞瘤[9]。当肿瘤位于室间孔区,有钙化,且伴有结节性硬化时,需要考虑该疾病。
脑膜瘤发生于脑室内少见,占颅内脑膜瘤0.5% ~3.7%[10],多见于成人,在儿童颅内肿瘤中所占比例小于3%,但儿童脑膜瘤17%发生于脑室内[1]。脑室内脑膜瘤主要起源于脉络丛组织或基质的蛛网膜成纤维细胞团,为胚胎发育过程中软脑膜随着脑血管延伸至脑深部参与形成脉络丛[11]。本组1例病灶在MR扫描T2以低信号为主,增强后明显不均匀强化,脑室无明显扩张,术前诊断困难。
颅内非典型畸胎样/横纹肌样瘤为高度恶性肿瘤,2岁以下常见,最常见于后颅窝,其次为幕上,少数可位于松果体区、脊髓及多灶性分布[12]。肿瘤常出现出血、坏死、边缘囊变。本组2例DWI上均呈明显高信号,其中1例同时伴有额叶异常强化结节,考虑可能为多灶性。
神经上皮囊肿曾被称为蛛网膜囊肿、室管膜囊肿、脉络膜囊肿、脉络膜上皮囊肿等,因其来源于脉络丛和室管膜,而脉络丛和室管膜组织是由原始神经上皮分化而来,因此目前统称为神经上皮囊肿。神经上皮囊肿在侧脑室中多见,较少发生于三脑室,也可发生于脑实质内[13]。本组90%发生于侧脑室,10%发生于三脑室。囊肿呈圆形、类圆形,囊壁薄,囊液成分多与脑脊液相似,增强扫描囊壁及囊液均无强化。该组1例呈多囊性,部分囊液CT密度稍高,另2例内部囊液T1信号稍高于脑脊液,T2高信号,考虑可能与囊液蛋白含量较高或囊液搏动有关。
综上所述,儿童幕上脑室占位性病变的病理类型复杂。其中最常见为脉络丛乳头状瘤,具有较特征性的影像学表现,当其发生在第三脑室时需要与毛细胞型星形细胞瘤、毛细胞黏液样星形细胞瘤鉴别。其次为神经上皮囊肿。室管膜瘤较幕下少见,影像学缺乏特征。室管膜下巨细胞星形细胞瘤常伴有结节性硬化。其他儿童幕上脑室肿瘤更为少见,包括脑膜瘤、非典型畸胎样/横纹肌样瘤等,仅从影像学上定性困难,但是DWI高信号以及有无脑水肿对良恶性肿瘤的诊断具有重要作用。
[1]Smith AB,Smirniotopoulos JG,Horkanyne-Szakaly I.From the radiologic pathology archives:intraventricular neoplasms:radiologic-pathologic correlation[J].Radiographics,2013,33(1):21-43.
[2]Louis DN,Ohgaki H,Wiestler OD,et al.The 2007 WHO classification of tumours of the central nervous system[J].Acta Neuropathologica,2007,114(2):97-109.
[3]李丽,宋建勋,孙鹏飞.非典型性脉络丛乳头状瘤1例[J].中国临床医学影像杂志,2010,21(1):74.
[4]Barkovich AJ.Pediatric neuroimaging[M].Philadelphia Pa:Lippincott Williams&Wilkins,2005:603-610.
[5]严嘉仪,李美蓉,李玉华.儿童颅内毛细胞型星形细胞瘤MRI表现[J].放射学实践,2013,28(7):746-749.
[6]Yuh EL,Barkovich AJ,Gupta N.Imaging of ependymomas:MRI and CT[J].Child's Nervous System,2009,25(10):1203-1213.
[7]王王华,段青,梁辉顺,等.室管膜下巨细胞星形细胞瘤的临床及神经影像学特征 [J].中国临床医学影像杂志,2010,21(4):261-264.
[8]Takei H,Adesina AM,Powell SZ.Solitary subependymal giant cell astrocytomaincidentallyfoundat autopsyinanelderly womanwithout tuberous sclerosis complex[J].Neuropathology,2009,29(2):181-186.
[9]Nabbout R,Santos M,RollandY,et al.Early diagnosis of subependymal giant cell astrocytoma in children with tuberous sclerosis[J].J Neur,Neuros&Psychiatr,1999,66(3):370-375.
[10]Liu M,Wei Y,Liu Y,et al.Intraventricular meningiomas:a report of 25 cases[J].Neuros Rev,2006,29(1):36-40.
[11]胡鹏,陈东,丁浩源.脑室内脑膜瘤的MRI诊断[J].中国医学影像学杂志,2013,21(10):741-744.
[12]Dang T,Vassilyadi M,Michaud J,et al.Atypical teratoid/rhabdoid tumors[J].Child's Nervous System,2003,19(4):244-248.
[13]范帆,包强,鱼博浪,等.颅内神经上皮囊肿的CT,MRI及DWI诊断[J].中国临床医学影像杂志,2010,21(7):501-503.
Imaging diagnosis of supratentorial ventricular masses in children
YANG Piao,LIMei-rong,LI Yu-hua
(Department of Radiology,Xinhua Hospital,Shanghai Jiaotong University School of Medicine,Shanghai 200092,China)
Objective:To explore the value of imaging diagnosis of supratentorial ventricular masses in children.Methods:Forty-five cases(25 males,aged from 4 months to 13 years with a median age of 2 years)of supratentorial ventricular masses in children confirmed by pathology were analyzed retrospectively.Results:Sixteen cases were choroid plexus papillomas,which appeared as lobulated or granular-countered masses.They were hyperattenuating on CT,iso-to hypointense on T1WI,iso-to hyperintense on T2WI and iso-to hypointense on DWI.Contrast-enhanced imaging showed avid enhancement.Six cases were atypical choroid plexus papillomas with the appearance of small calcifications(n=1),CSF spreading(n=2)and peritumoral edema (n=2).One case was choroid plexus carcinoma,which was solid-cystic with hyperintensity on DWI.Four cases were pilocytic astrocytoma,and 2 cases were pilomyxoid astrocytoma.They were located in the third ventricle,with hypointensity on DWI and intense enhancement.Two cases were ependymomas.Two cases were atypical teratoid/rhabdold tumors.One case was subependymal giant cell tumor.One case was meningioma.Ten cases were neuroepithelial cysts,which showed a thin cyst wall.They showed similar intensity to CSF and no enhancement.Conclusion:The types of the supratentorial ventricular masses in children are varied.CT and MRI can reflect certain characteristics of the masses in this region.With the help of clinical and imaging findings,the diagnosis can be drawn in most cases.
Choroid plexus neoplasms;Child;Tomography,X-ray computed;Magnetic resonance imaging
R739.41;R814.42;R445.2
A
1008-1062(2015)03-0153-04
2014-08-12;
2014-10-09
杨飘(1991-),女,浙江东阳人,硕士研究生。
李玉华,上海交通大学医学院附属新华医院放射科,200092。
