液氨吸入性肺炎损伤的影像学表现及动态观察
2015-10-17赵洪全孔丽丽程永远孙海成
赵洪全,孔丽丽,程永远,孙海成
(1.烟台经济技术开发区医院影像科,山东 烟台 264006;2.烟台市莱阳中心医院放射科,山东 莱阳 265200)
液氨吸入性肺炎损伤的影像学表现及动态观察
赵洪全1,孔丽丽1,程永远2,孙海成2
(1.烟台经济技术开发区医院影像科,山东 烟台264006;2.烟台市莱阳中心医院放射科,山东 莱阳265200)
目的:回顾分析急性氨中毒所致吸入性肺炎损伤的影像学表现,探讨病变的演化过程。资料与方法:一次事故致30例健康青年人急性氨中毒吸入性肺炎,男9例,女21例。对伤者的所有胸部影像资料进行回顾,重点对19例中、重度中毒者的CT影像表现进行动态比较分析。结果:本组30例伤者,轻度中毒11例(36.7%),X线主要表现为肺纹理增多模糊,均在7 d内治愈出院,10月后CT复查未见异常。中度中毒10例(33.3%),急性期CT主要表现:支气管血管束增粗模糊10例,小片状影4例,树芽征1例与上述小片状影同时存在。临床治愈出院3月后CT复查,6例无异常发现,4例局部显示轻度间质纤维化征象。9例(30%)重度中毒者2月内,6例表现为细支气管肺泡炎的征象,可见大小不等的斑片影,毛玻璃密度影(GGO)和“马赛克征”;2例表现为细支气管损伤性炎症并阻塞的征象,表现为弥漫分布的“树芽征”等,并很快形成坏死性空洞;1例表现为多发肺组织破坏,空洞形成,同时并发气胸、液气胸、皮下及纵隔气肿等。3月后病变慢性化,斑片影、“树芽征”等逐渐吸收,气胸、皮下及纵隔气肿吸收减少,厚壁空洞逐渐演变为空腔样病变,但GGO和“马赛克征”吸收缓慢。结论:液氨吸入性肺炎病变多样,重度中毒损伤有复杂的病变演化过程,CT对肺内病变的观察有较重要的价值。
肺炎,吸入性;体层摄影术,螺旋计算机;放射摄影术
液氨吸入性肺炎属于职业性损伤[1-4]。该损伤有关的国家诊断标准[1-2],主要依据临床症状、体征、胸部X线征象和血气分析四方面的情况评价损伤程度,不包括CT影像。近些年国内外不断报道液氨泄漏致多人伤亡的事故[3-6],有关文献多集中在临床治疗与护理经验的总结[5-7],CT诊断方面的文献很少[8]。本文回顾总结了一次液氨泄漏事故引起的30例伤者的影像资料。重点探讨液氨吸入性肺炎损伤病变的CT表现和临床变化过程,为该病的临床诊治积累经验,也为国家有关部门修订相关诊断标准时,增加CT方面的诊断依据提供参考。
1 资料和方法
1.1一般临床资料
该事故造成损伤的员工都是健康的青年人,女工多。从液氨泄漏至得到有效控制,历时约10min。员工的受伤程度不一,“一过性反应”多人未统计,事发1 h内死亡2例 (未住院治疗)。住院救治的30例,男9例,女21例,年龄20~37岁,平均25.5岁。按有关国家诊断标准[1-2],结合CT影像表现,30例分为:轻度中毒11例,中度中毒10例,重度中毒9例。19例中、重度中毒者,住院29~461 d,平均为212.3 d,17例康复或好转出院,2例男性分别于伤后71 d和357 d死于呼吸功能衰竭。
1.2影像学检查及影像分析方法
早期摄床边CR片,2周后逐步用CT扫描。19例中、重度伤者CT检查2~10次,共116例次,平均6.1次。CT为GE-Hispeed全身螺旋CT机。扫描参数:120 kV,130~200mA,平扫层厚5~10mm,螺距1,快速连续扫描,部分病变采用薄层扫描,层厚5mm,未行增强扫描和高分辨扫描。所有影像学资料的观察与分析均由两名副高以上职称的影像诊断医生讨论确定。
2 结果
2.1轻度液氨中毒吸入性肺炎
轻度中毒的11例(36.7%),急性期未行CT检查,CR片主要表现为肺纹理增多模糊,未见明显肺损伤炎症表现。均在1周内治愈出院,10月后随访复查,临床和CT均无异常发现。
2.2中度液氨中毒吸入性肺炎
10例(33.3%)中度中毒,1~2月内主要表现:①10例均表现支气管血管束增粗、模糊(100%);②4例(40%)表现为双肺散在的小片状影,大小约1~3 cm,治疗后吸收完全(图1a,1b);③树芽征1例,与上述小片状影同时存在(图1b);④局限性肺气肿3例,表现为部分肺叶透光强,肺透光不均匀。出院后3月随访复查CT,6例无异常,4例局部显示轻度间质纤维化征象,其中1例伴小囊状支气管扩张。
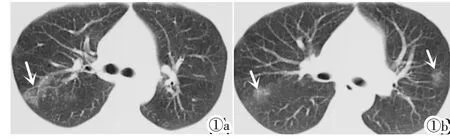
图1中度肺损伤2例。图1a:伤后40 d,双肺血管纹理增多,右肺局部见多发小点片状影,呈“树芽征”(↑);图1b:伤后30 d,双肺血管纹理增多,双肺散在小片状影(↑)。
Figure 1.Two cases of moderate lung injury.Figure 1a:40 days after injury.Pulmonary vascular texture was increase and multiple small patchy shadow was shown in the right lung characterized by“tree-in-bud”(↑).Figure 1b:30 days after injury.Pulmonary vascular texture was increased and scattered small patches were shown(↑).
2.3重度液氨中毒吸入性肺炎
9例(30%)重度中毒者表现复杂,病变发展过程中可见多种肺内病变:①大片状影2例,多发较大范围密度较高的阴影,经一定时间后可坏死,形成蜂窝状影和厚壁空洞(图2a~2d)。②广泛分布的小片状影6例,密度淡,大小1~2 cm,呈半透明状或局灶性磨玻璃影(GGO),并可见“马赛克征”。这种毛玻璃样密度影,持续时间长,可达3~6月(图3a~3e)。③典型树芽征2例(图4a~4c,图5a)。④厚壁空洞3例,腔内无液平,大小形态多变,经治疗后逐步变为空腔样病变(图2,4,5),其他多发的薄壁空腔4例,大小不等,且不断变化,可愈合消失(图4d~4f)。⑤双肺广泛肺气肿8例,见于损伤3月以后的慢性期(图3f)。⑥间质性病变包括小叶间隔增厚(网状影、线状影),支气管血管束增粗增多7例。伴随肺纤维化的出现,形成不规则纤维斑块影4例,以上病变在伤后3月明显(图2e,2f,3f)。⑦并发症征象包括支气管扩张4例见于慢性期,双侧(液)气胸1例、纵隔及皮下气肿3例等见于损伤早期(图2a~2c,5a)。
2.4重度液氨中毒吸入性肺炎病变的演化过程
9例重度中毒者,6例病变演化过程类似:早期平片未见明显片状影,但患者临床症状重,CT显示弥漫性病变。损伤的2月内,CT主要表现为双肺弥漫性肺泡水肿和肺泡炎的改变,如大、小斑片影,呈GGO性病灶,“马赛克征”等。同时有细支气管炎改变,包括肺支气管血管束的增多、模糊等 (图3a,3b)。3月后随着病情的稳定,病变向慢性发展,大、小斑片影吸收好转;GGO,“马赛克征”等长期存在,吸收缓慢(图3c,3d),最终残留不均匀性肺气肿和间质纤维化表现(图3e,3f)。2例早期X线片无明显片状影,患者临床症状重,伤后30~40 d,双肺出现阻塞性细支气管炎表现,呈典型弥漫性分布的“树芽征”(图4a~4c,5a);并短期加重出现局部蜂窝状或空洞样破坏,形成厚壁空洞,空洞存留较长时间,变化多样(图4d,5b,5c)。3月后病变慢性化,空洞逐渐变为空腔样病灶。最终残留的病变主要有广泛的肺气肿、纤维化、多发小空腔样病灶和支气管扩张等(图4e,4f,5d),其中1例死亡。③1例急性期表现为多发片状影,很快肺组织破坏、形成多发空洞,先后
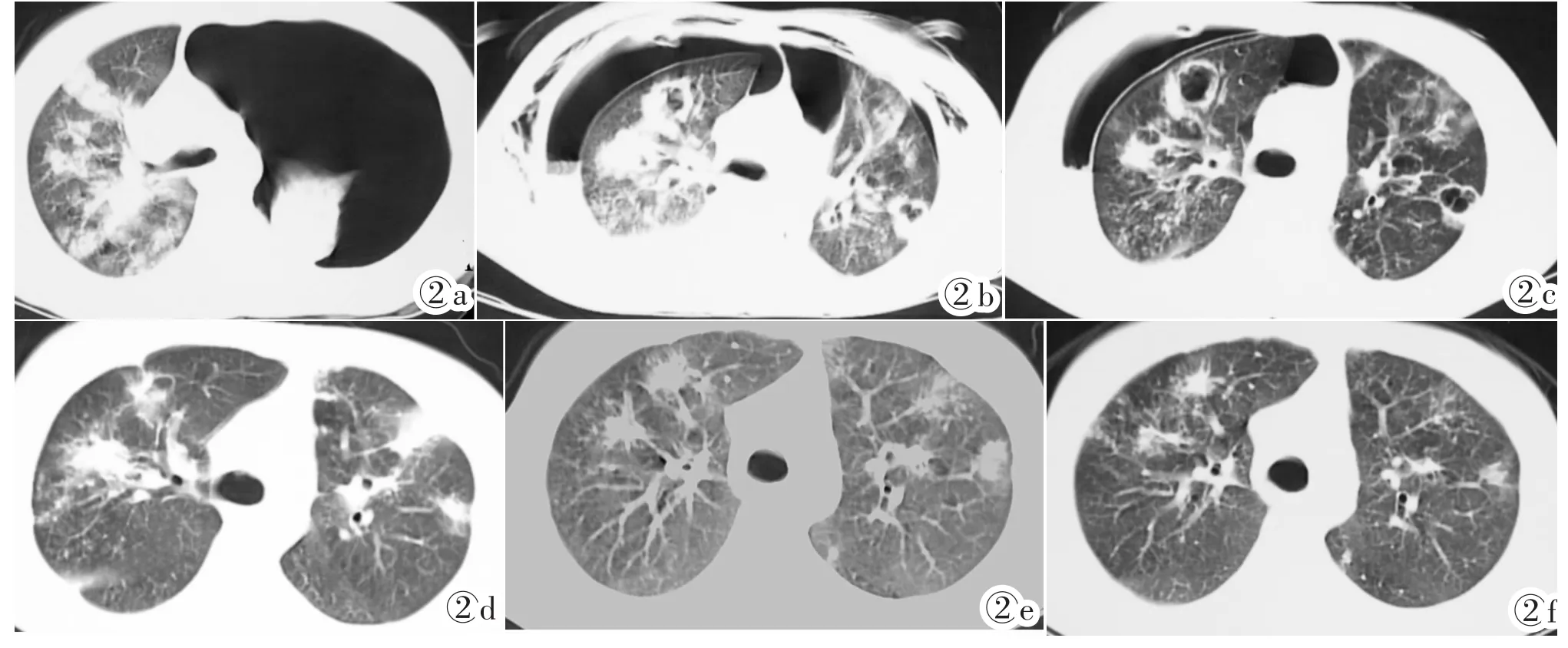
图2重度肺损伤例1。图2a:伤后28 d,左侧气胸肺压缩,右肺多发大片状影;图2b:伤后2月左侧气胸逐渐吸收,右侧液气胸,双侧胸腔闭式引流,双肺多发坏死性空洞,胸壁皮下气肿;图2c:伤后3月左侧气胸吸收,右侧液气胸好转,双肺多发空洞部分转为空腔样病灶,皮下气肿吸收,病情稳定;图2d:伤后4月双肺多发不规则团块状、纤维索条病灶,空洞闭合;图2e:伤后5月;图2f:伤后7月,双肺见慢性纤维性病灶,好转出院。
Figure 2.Case 1 of severe lung injury.Figure 2a:28 days after injury,the left lung was compressed by pneumothorax.Multiple patchy shadows occurred in the right lung.Figure 2b:Two months after injury,the left pneumothorax was absorbed gradually and liquid pneumothorax occurred in the right side with bilateral closed drainage of chest.Multiple necrotic cavities occurred in both lungs with subcutaneous emphysema in chest wall.Figure 2c:Three months after injury,left pneumothorax was absorbed and the right liquid pneumothorax was relieved. Part cavities developed into cavum with disapperace of subcutaneous emphysema.Figure 2d:Four months after injury,multiple irregular crumby or fibrotic lesions remained with enclosure of cavities.Figure 2e:Five months after injury.Figure 2f:Seven months after injury,both lungs showed chronic fibrotic lesions.
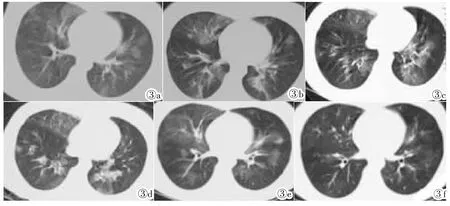
图3重度肺损伤例2。图3a:伤后30 d,双肺弥漫分布GGO密度灶,边缘模糊,呈“马赛克征”表现;图3b:伤后2月,病灶密度增高;图3c:伤后3月,病灶密度进一步增高;图3d:伤后5月,病灶吸收减少,密度增高;图3e:伤后7月,双肺病灶吸收好转,残留散在GGO密度灶,呈“马赛克征”表现;图3f:伤后10月,双肺残留细小纤维性病灶,好转出院。
Figure 3.Case 2 of severe lung injury.Figure 3a:30 days after injury,diffuse distribution of ground glass opacity(GGO)and“mosaic”sign were shown.Figure 3b:Two months after injury,the density of lesions increased.Figure 3c:Three months after injury,the density of lesions inreased further.Figure 3d:Five months after injury,lesions decreased and their density increased;Figure 3e:Seven months after injury,lesions were absorbed and some residual GGO and“mosaic”sign were shown.Figure 3f:Ten months after injury,some residual fine fibrosis was shown.双侧气胸、液气胸,皮下气肿(图2a~2c)。3月后气胸、液气胸吸收好转,双肺多发空洞部分转为空腔样病灶。后空腔闭合,逐渐演变为多发不规则团块状、纤维索条状病灶,最终残留慢性纤维性病灶(图2d~2f),好转出院。
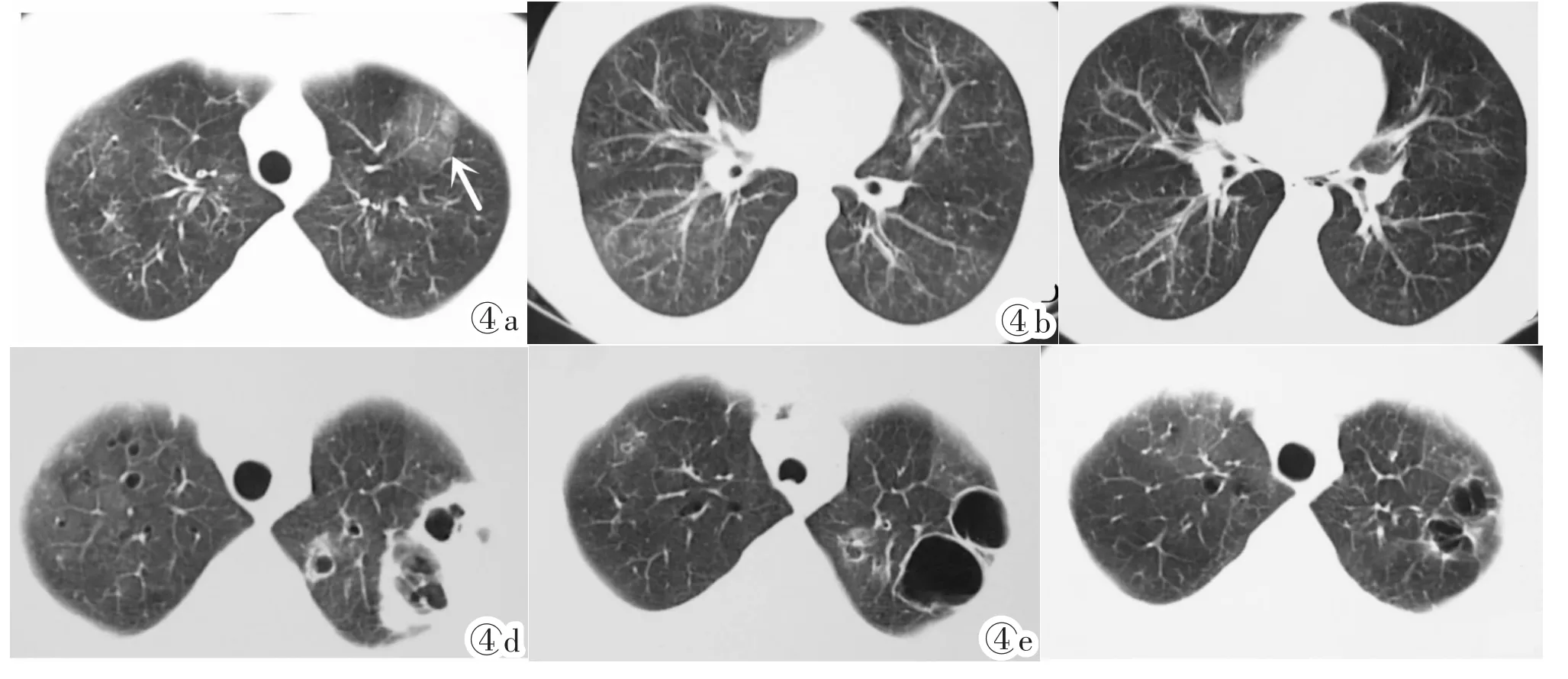
图4重度肺损伤例3。图4a,4b:伤后30 d,双肺弥漫分布的点片状影,呈典型“树芽征”,伴散在片状GGO(↑);图4c:伤后2月,双肺“树芽征”部分吸收;图4d:伤后80 d,左上肺破坏见不规则厚壁空洞,右上肺多发小囊状病灶;图4e:伤后4月,左上肺空洞演变为空腔样病灶,双肺见多发纤维灶;图4f:伤后10月,左上肺残留不规则空腔样病灶,双肺散在纤维性病灶,好转出院。
Figure 4.Case 3 of severe lung injury.Figure 4a,4b:30 days after injury,diffuse dot and patchy shadows in both lungs with typical “tree-in-bud”and scattered flake GGO(↑)were shown.Figure 4c:Two months after injury,part“tree-in-bud”was absorbed.Figure 4d:80 days after injury,irregular thick wall cavity in upper left lung and multiple cystic lesions in upper right lung were shown.Figure 4e:Four months after injury,the cavity in upper left lung changed into cavum with multiple fibrosis in both lungs.Figure 4f:Ten months after injury,a residual irregular cavum remained in left upper lung with scattered fibrosis in both lungs.
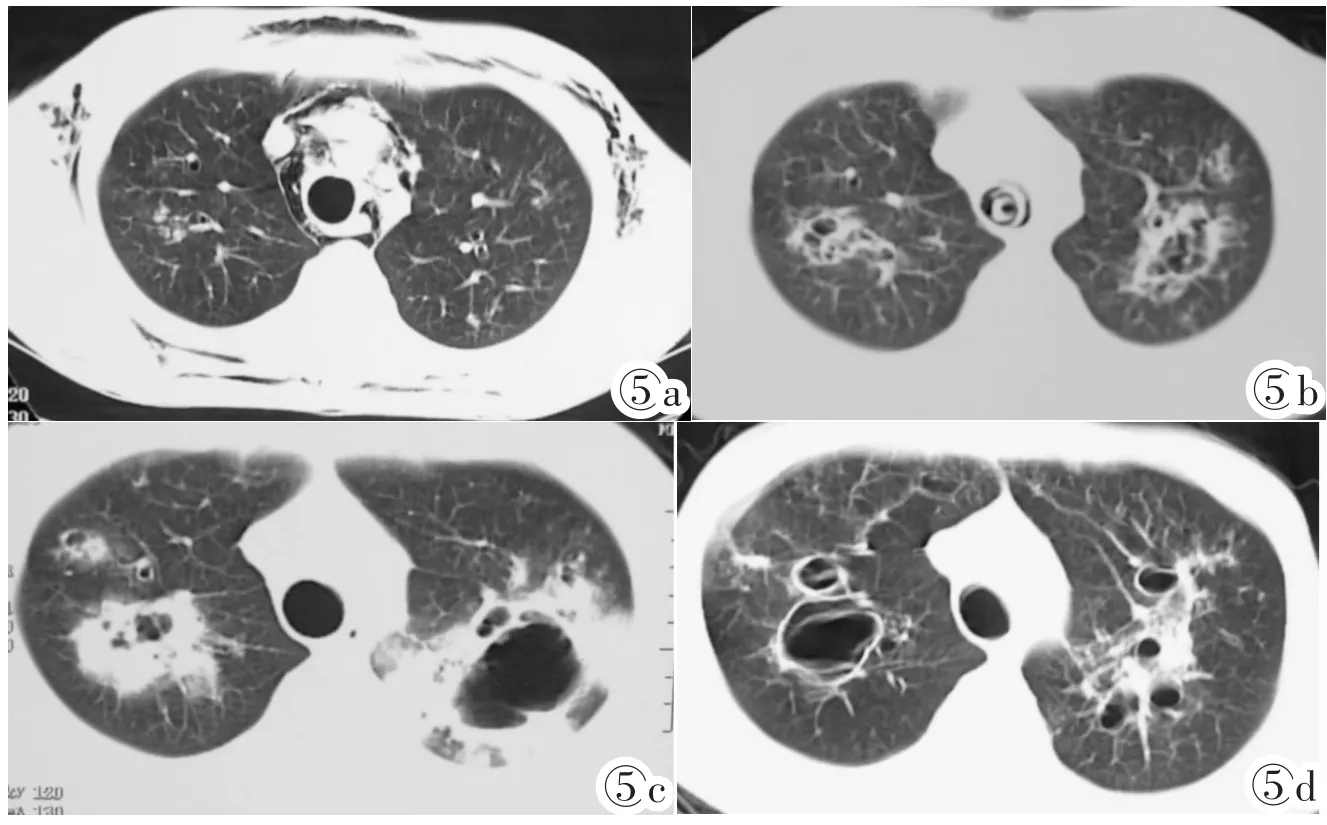
图5重度肺损伤例4。图5a:伤后45 d双肺弥漫分布的点状影,可见树芽征,伴多发小囊状病灶;图5b:伤后70 d,双上肺组织破坏,呈蜂窝状病灶;图5c:伤后3月,双肺厚壁空洞;图5d:伤后8月双上肺空洞好转,残留空腔样病灶和纤维灶;伤后357 d突发呼吸道结痂脱落导致气道梗阻死亡。
Figure 5.Cases 4 of severe lung injury.Figure 5a:45 days after injury,diffuse distribution of dots with“tree-in-bud”and multiple cystic lesions were shown in both lungs. Figure 5b:70 days after injury,both lungs were damaged with honeycomb lesions.Figure 5c:Three months after injury,thick wall cavities were shown.Figure 5d:Eight months after injury,cavity lesions were relieved and taken place by residual cavum and fibrosis.357 days after injury,the patient died of sudden falling of respiratory scabs which caused airway obstruction.
3 讨论
3.1液氨吸入性肺炎的临床特点
液氨在化工和食品冷藏加工行业应用广泛,化学事故发生率相当高[3-4]。氨气属于中央气道作用性有毒工业化学物质,经呼吸道吸入可造成呼吸道黏膜的坏死[3-4],同时可引起眼球和皮肤灼伤,多发生在面部和四肢等暴露部位[3-4,7]。高浓度氨气可引起反射性呼吸停止和心脏停搏而死亡[3-7]。由于伤者常合并较大面积和重度皮肤损伤,早期皮肤治疗和急救阶段CT检查受到限制,床边X线片较方便实用,床边X线检查操作应严格执行有关国家标准[2]。
3.2本组病例资料的特点
本组病例具有以下特点:①住院时间长,伤者前后经过多次CT扫描检查,对病变的观察全面,可很好地观察肺损伤的CT表现与病变的发展过程,但对部分重度损伤病人可能存在射线超标的问题。②伤者事前均为健康的青年人,对这些人CT影像的回顾,可以认为是对正常人液氨吸入性肺炎损伤CT表现的总结。③由于住院时间长,尤其是重度伤者,治疗期间可能并发细菌性肺炎等多种并发症。本文主要回顾总结了该损伤的CT征象及病变演化过程,有关并发症的征象也应该属于该吸入性肺炎损伤的CT表现,并可作为损伤程度评价的依据,本组病例多未进行细菌培养是其不足。
3.3重度液氨吸入性肺炎损伤CT病变的演化过程
对9例重度肺损伤多次CT影像的动态观察分析可以总结发现液氨吸入性肺炎的病变演化过程。在损伤早期的2月内,多数病例CT主要表现细支气管和肺泡炎的改变,可见大、小不等的斑片影,GGO,“马赛克征”;部分表现为细支气管炎并阻塞征象,表现为弥漫分布的“树芽征”等。极少数病例表现为多发肺组织破坏,空洞形成,同时并发气胸、液气胸、皮下及纵隔气肿等。其中GGO和“马赛克征”吸收缓慢、长期存在是其特点。另外表现为弥漫“树芽征”的2例伤者,短期出现坏死空洞,预示病变较重,空洞形成可能与细支气管阻塞,通气不畅,合并肺内炎症有关。伤后3月,随着病程的稳定,病变开始向慢性发展,大、小斑片影多吸收好转;“树芽征”等逐渐吸收;气胸、液气胸、皮下及纵隔气肿吸收减少;厚壁空洞逐渐演变为空腔样病变。GGO,“马赛克征”则长期存在。同时逐渐出现肺炎机化、纤维化及并发症改变,可见纤维斑块影、索条影、支气管扩张、肺气肿等。重度损伤最终残留的病变主要是广泛的肺气肿、纤维性病灶、空腔样病变和支气管扩张等。
3.4CT判定液氨吸入性肺炎损伤程度的可行性
多年来,有关液氨吸入性肺炎损伤的国家诊断标准[1-2],在指导临床诊治和损伤程度评价等方面发挥了重要作用,本组伤者也按照该评价方法进行诊断分级。但是,本组伤者的胸部X线征象与其他临床表现存在较明显的不相称:19例中、重度中毒者在早期X线片除了肺纹理改变外,仅7例发现较明显的片状影等病变,但临床症状和其他诊断指标提示患者伤情较重,后来的CT检查证实有明显的肺损伤病变。普通X线片对液氨吸入性肺炎病变多样性的观察也有一定限度,而CT检查在观察各种病变及分布、判定肺损伤的程度、观察慢性期间质性病变、观察并发症等方面有明显优势。因此在患者病情允许的情况下,应尽早进行CT检查,同时建议国家有关部门修订有关标准时,增加CT方面的诊断依据。根据本组的观察,CT对该损伤的诊断可做如下分级:①轻度中毒,主要表现支气管血管束增多或伴边缘模糊,短期治疗吸收恢复,一般不必行CT扫描;②中度损伤,可表现为支气管血管束增多,边缘模糊或呈网状阴影;肺野透亮度降低或不均匀;或有边缘模糊散在的斑片状阴影;符合肺炎或间质性肺炎的表现,治疗后吸收完全,不留明显痕迹。③重度中毒,主要表现为两肺多发的密度较淡边缘模糊的斑片状、云絮状阴影;广泛分布的“树芽征”样改变,广泛的GGO及“马赛克征”改变,符合严重的肺炎或肺泡性肺水肿;有空洞或空腔形成,或较重的气胸或纵隔气肿,皮下气肿;3月后多有不可恢复的病变如广泛间质纤维化、肺气肿、纤维斑块、支气管扩张、空腔样病变等。
[1]中华人民共和国卫生部.职业性急性氨中毒诊断标准 (GBZ14-2002)[M].北京:法律出版社,2002:4.
[2]中华人民共和国卫生部.职业性急性化学物中毒性呼吸系统疾病诊断标准(GBZ73-2009)[M].北京:人民卫生出版社,2009:11.
[3]和丽秋.液氨泄漏事故现场处置探析 [J].职业卫生及应急救援,2014,32(3):175-177.
[4]赵建,杜先林.有毒工业化学物质中的肺损伤毒剂[J].职业卫生及应急救援,2014,32(1):45-47.
[5]吴桂生.氨气吸入性肺损伤30例临床观察 [J].内蒙古中医药,2010,29(5):80-81.
[6]赵凤德,韩明峰,孙伟,等.急性氨气吸入性肺损伤32例临床诊治分析[J].蚌埠医学院学报,2012,37(4):412-414.
[7]Makarovsky I,Markel G,Dushnitsky T,et al.Ammonia—when something swell wrong[J].IMAJ,2008,10(7):537-543.
[8]张国梁.液氨吸入性肺损伤21例CT与临床特点分析[J].中国厂矿医学,2008,21(1):24-25.
Imaging findings and follow-up observation of aspiration pneumonia injury caused by liquid ammonia poisoning
ZHAO Hong-quan1,KONG Li-li1,CHENG Yong-yuan2,SUN Hai-cheng2
(1.Department of Imaging,Yantai Economic and Technological Development Zone Hospital,Yantai Shandong 264006,China;2.Department of Radiology,Laiyang Central Hospital,Laiyang Shandong 265200,China)
Objective:To retrospectively analyze imaging manifestations of aspiration pneumonia caused by acute ammonia poisoning and investigate its changing process.Materials and Methods:In an accident,30 healthy young people suffered from acute ammonia poisoning(9 males and 21 females).All the chest imaging data were reviewed,and special emphasis was put on follow-up CT imaging manifestation of 19 moderate to severe cases.Results:Of the 30 cases,11 mild poisoning (36.7%)were cured in seven days.Pulmonary texture became increased and fuzzy from their X-ray examinations and there were no abnormality on follow-up CT images after 10 months.For 10 cases of moderate poisoning(33.3%)in acute phase,CT images showed fuzzy broncho-vascular markings in 10 cases,spotty shadows in 4 cases,and tree-in-bud sign with small lamellar shadows in 1 case.After 3 months,the results of CT manifestations were no abnormal findings in 6 cases,local mild fibrosis in 4 cases.For 9 cases(30%)of severe lung injury within 2 months,6 cases showed signs of alveobronchiolitis with patchy shadows varying in size,ground glass opacity(GGO)and“mosaic”sign.Two cases showed signs of bronchiolar inflammation and obstruction,which was characterized by diffuse distribution of“tree-in-bud”and quick formation of necrotic cavity.One case showed multiple lung tissue injuries and formation of necrotic cavities,complicated with pneumothorax,liquid pneumothorax,subcutaneous and mediastinal emphysema etc.After 3 months,lung injuries became chronic.Small shadows and “tree-in-bud”were absorbed gradually.Pneumothorax,subcutaneous and mediastinal emphysema were reduced.The cavum took the place of thick wall cavities.But the absorption of GGO and“mosaic sign”took a long time.Conclusion:Varied manifestation could occur during aspiration pneumonia owing to liquid ammonia poisoning with complex changes in severe cases.CT imaging manifestations played an important role in observing lung injuries.
Pneumonia,aspiration;Tomography,spiral computed;Radiography
R563.1;R814.42;R814.41
A
1008-1062(2015)03-0170-05
2014-05-05;
2014-10-12
赵洪全(1964-),男,山东莱阳人,主任医师。
