去骨瓣减压联合血管重建术对重型颅脑损伤患者脑灌注的影响
2015-06-28黄良珍刘朝晖彭浩赵建农
黄良珍,刘朝晖,彭浩,赵建农
去骨瓣减压联合血管重建术对重型颅脑损伤患者脑灌注的影响
黄良珍,刘朝晖,彭浩,赵建农
目的比较标准大骨瓣减压联合脑-硬脑膜-肌肉血管重建术与传统标准大骨瓣减压术治疗重型颅脑损伤的临床效果。方法选择2012年3月-2015年3月收治的以额颞叶脑挫裂伤为主的重型颅脑损伤患者48例,随机分为试验组和对照组,每组24例。试验组采用标准大骨瓣减压联合脑-硬脑膜-肌肉血管重建术,对照组采用传统标准大骨瓣减压术,术后通过CT灌注成像(CTP)观察脑组织血流动力学改变,指标包括脑血流量(CBF)、脑血容量(CBV)、平均通过时间(MTT)、达峰时间(TTP),以及术侧与对侧的比值(即rCBF、rCBV、rMTT、rTTP),并对术后半年的格拉斯哥预后评分(GOS)情况进行分析。结果试验组术后1周及1个月时的CBF、CBV高于对照组,MTT、TTP低于对照组,差异均有统计学意义(P<0.05);试验组术后1周和1个月时的rCBF、rCBV、rMTT、rTTP差异无统计学意义(P>0.05),而对照组术后1周时的rCBF、rCBV值高于术后1个月时,rMTT、rTTP低于术后1个月时,差异有统计学意义(P<0.05)。术后半年GOS评分结果显示,试验组中恢复较好(包括良好和中残)的比例高于对照组,而恢复较差(包括重残、植物状态、死亡)的比例低于对照组,差异均有统计学意义(P<0.05)。结论标准大骨瓣减压联合脑-硬脑膜-肌肉血管重建术在降低重症颅脑损伤患者颅内压的同时能有效改善受损脑组织的血供,疗效显著,预后较好,值得临床应用及推广。
颅脑损伤;减压颅骨切除术;脑血管重建术;灌注成像
重型颅脑损伤的致死率、致残率高,文献报道其致死率约为35%[1]。特别是对冲伤引起的以额颞叶脑挫裂伤为主的重型颅脑损伤往往合并颅内血肿、脑水肿、脑梗死、脑疝,患者病情重、进展快,预后较差[2-4]。目前对以额颞叶脑挫裂伤为主的重型颅脑损伤尤其是并发脑疝后的治疗,主要采用急诊标准大骨瓣减压和颅内血肿清除术[5],但由于脑组织小血管损伤以及正常的血液循环和血脑屏障被破坏,重新建立新的血供需要的时间长甚至无法建立血供,术后利用血管扩张药进行活血化瘀治疗效果较差,且单纯的去骨瓣减压手术对局部脑挫裂伤引起的血液循环障碍、脑水肿改善作用不明显。脑血管重建术长期用于脑缺血性疾病的治疗,利用脑膜中动脉和颞浅动脉作为血管供体,改善成年烟雾病缺血症状疗效确切[6-7]。本研究采用去骨瓣减压联合间接血管重建术治疗以额颞叶脑挫裂伤为主的重型颅脑损伤,术后通过CT灌注成像(CT perfusion,CTP)观察脑组织血流动力学的改变,并对术后半年的格拉斯哥预后评分(GOS)情况进行分析,旨在为重型颅脑损伤患者的临床治疗提供指导。
1 资料与方法
1.1 临床资料 选择2012年3月-2015年3月收治的以额颞叶脑挫裂伤为主的重型颅脑损伤患者48例,其中男23例,女25例,年龄52~75岁,平均59.3岁,GOS评分3~8分。致伤原因:交通伤25例,坠落伤13例,混合伤8例,其他伤2例。所有患者均有开颅减压手术指征。按入院时间奇偶数分为对照组和试验组,每组24例,分别行标准大骨瓣减压和标准大骨瓣减压联合脑-硬脑膜-肌肉血管重建术。纳入标准为:①明确的外伤史,以额颞叶脑挫裂伤为主的重型颅脑损伤;②临床表现有昏迷、偏瘫、失语或四肢瘫,有生命体征改变;③有一侧或双侧瞳孔散大;④CT检查均为幕上病变,一侧额颞叶脑挫伤和硬膜下血肿:⑤血肿>60ml,脑池变窄或封闭,中线结构移位>5mm;⑥患者年龄18~68岁。排除标准为:①原发性脑干损伤、严重合并伤、失血性休克、呼吸循环等多系统衰竭、凝血功能异常者;②既往有高血压病、经常性头痛等可疑脑血管病者;③既往有脑肿瘤者。
1.2 手术方法 对照组采用标准大骨瓣减压传统术式:额颞顶大弧形切口,始于发际内中线旁2~3cm处,与上矢状窦平行向后达顶结节,再呈弧形向下转向前至颞部,在耳前垂直向下,在耳屏前1cm直达颧弓。头皮切口直达颅骨,形成肌皮瓣,将其翻向前下方(即额颞处),暴露出颅骨的额颞顶区。在裸露的颅骨上行5~6个钻孔,并将各骨孔锯断,用咬骨钳咬除颅骨至中颅窝底,大小约12cm×14cm,形成一个包括额骨、颞骨鳞部及顶骨的大型游离骨瓣。清除硬膜外、硬膜下、脑内血肿及脑挫裂伤坏死组织,悬吊硬脑膜,留置引流管,缝合帽状腱膜层及头皮后关颅。试验组采用标准大骨瓣减压联合脑-硬脑膜-肌肉血管重建术:手术过程基本同上,但在切开头皮时避免损伤颞浅动脉主干,以骨膜剥离子剥离颞肌,保留完整的颞深动脉网络,游离骨瓣时保留脑膜中动脉,再清除硬膜下血肿及失活的脑组织,沿脑膜中动脉的主干及主要分支两侧剪开硬脑膜,宽度0.5~1.0cm。其余部位硬脑膜放射状剪开,止血后将其反折贴敷于脑皮层表面,取保留有颞浅动脉的颞肌和硬脑膜一起行减张缝合,去除骨瓣,硬膜外放置引流管,缝合帽状腱膜层及头皮。
1.3 评价指标 术后第7天和第30天采用飞利浦公司Light Speed 256排螺旋CT扫描机获得CTP图像。由VPCT Neuro分析软件自动生成脑血流量(cerebral blood flow,CBF)、脑血容量(cerebral blood volume,CBV)、平均通过时间(mean transit time,MTT)和达峰时间(time to peak,TTP)的灌注参数图。扫描时选择额颞叶脑挫裂伤最严重的部位作为感兴趣区(ROI),由系统自动选取对侧镜像ROI,获得各个ROI的灌注参数,即CBF、CBV、MTT、TTP值。将各组患者ROI参数的平均值作为绝对CBF、CBV、MTT、TTP值,用术侧与对侧的比值计算出相对灌注参数,即rCBF、rCBV、rMTT、rTTP值。比较两组术侧各参数绝对值,评价试验组和对照组术后1周和术后1个月时血流灌注的差异;对两组患者前后两次各参数的相对值进行比较,评价术后脑灌注的变化情况。
术后半年对两组患者进行GOS评分并行组间比较,评价两组患者预后情况。
1.4 统计学处理 采用SPSS 20.0软件进行统计分析。计量资料以表示,组间比较采用t检验,计数资料以百分数表示,组间比较采用χ2检验。P<0.05为差异有统计学意义。
2 结 果
试验组术后1周和1个月时的CBF、CBV明显高于对照组,MTT、TTP明显低于对照组,差异有统计学意义(P<0.05)。试验组术后1周和1个月时的CBF、CBV、MTT、TTP比较差异均无统计学意义(P>0.05),对照组术后1个月时的CBF、CBV低于术后1周水平,MTT、TTP高于术后1周水平(P<0.05)。试验组术后1周和1个月时的rCBF、rCBV、rMTT、rTTP比较差异无统计学意义(P>0.05),对照组术后1个月时的rCBF、rCBV低于1周水平,rMTT、rTTP高于术后1周水平,差异有统计学意义(P<0.05,表1)。
表1 两组术后血流动力学变化比较(±s,n=24)Tab. 1 Comparison of hemodynamic changes after operation in two groups (±s,n=24)
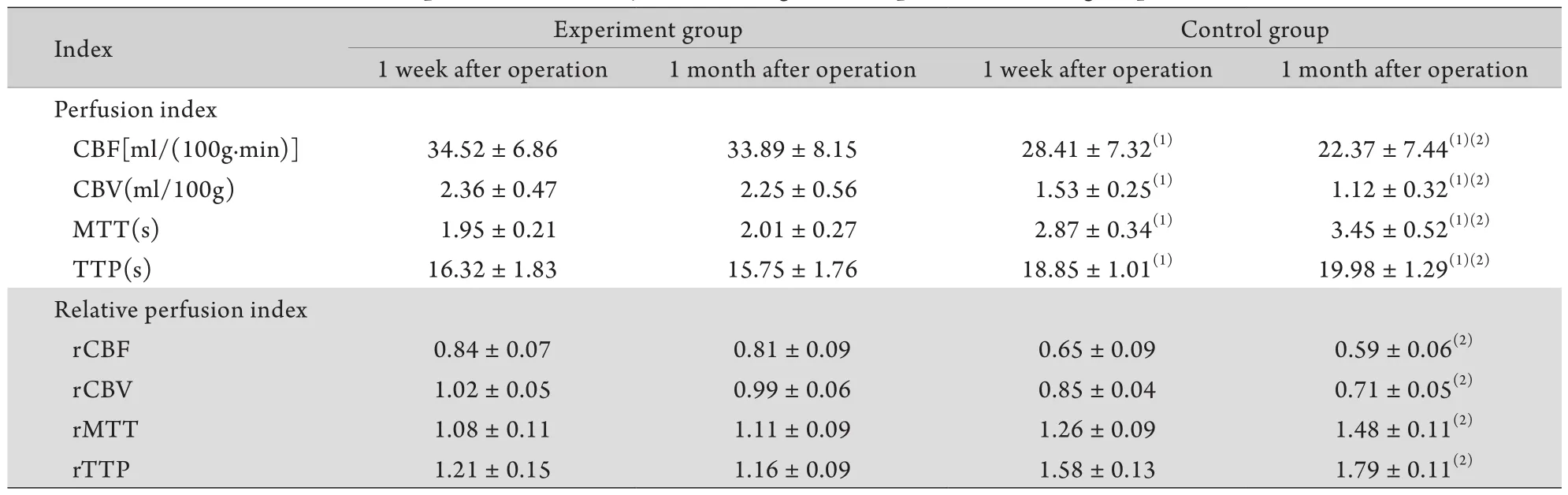
表1 两组术后血流动力学变化比较(±s,n=24)Tab. 1 Comparison of hemodynamic changes after operation in two groups (±s,n=24)
(1)P<0.05 compared with experiment group; (2)P<0.05 compared with 1 week after operation
Index Experiment group Control group 1 week after operation 1 month after operation 1 week after operation 1 month after operation Perfusion index CBF[ml/(100g.min)] 34.52±6.86 33.89±8.15 28.41±7.32(1) 22.37±7.44(1)(2)CBV(ml/100g) 2.36±0.47 2.25±0.56 1.53±0.25(1) 1.12±0.32(1)(2)MTT(s) 1.95±0.21 2.01±0.27 2.87±0.34(1) 3.45±0.52(1)(2)TTP(s) 16.32±1.83 15.75±1.76 18.85±1.01(1) 19.98±1.29(1)(2)Relative perfusion index rCBF 0.84±0.07 0.81±0.09 0.65±0.09 0.59±0.06(2)rCBV 1.02±0.05 0.99±0.06 0.85±0.04 0.71±0.05(2)rMTT 1.08±0.11 1.11±0.09 1.26±0.09 1.48±0.11(2)rTTP 1.21±0.15 1.16±0.09 1.58±0.13 1.79±0.11(2)
术后半年GOS评分结果显示,试验组中良好17例、中残3例、重残、植物状态及死亡各1例,对照组中良好9例、中残4例、重残5例、植物状态4例、死亡2例。试验组恢复较好(包括良好和中残,共20 例)的比例高于对照组(共13例),差异有统计学意义(χ2=2.11,P<0.05),恢复较差(包括重残、植物状态、死亡,共3例)的比例低于对照组(共11例),差异有统计学意义(χ2=2.40,P<0.05)。
3 讨 论
重症颅脑损伤病情复杂,常易并发创伤性脑水肿和脑梗死,其发生和发展严重影响患者的预后[8-9]。创伤性脑水肿和脑梗死通常与下列几种情况有关:脑组织、脑血管受损,引起血管内膜损伤或出血,形成血管栓塞或闭塞;脑血管痉挛、蛛网膜下腔出血后脑血管痉挛可导致脑梗死,而头部外伤后也可产生类似的脑血管痉挛[10-12];因脑组织损伤、水肿,肿胀的脑组织移位,引起血管移位、受压、迂回、扭曲,血液滞留、阻塞而发生脑梗死等[13]。创伤性脑水肿和创伤后引起的脑梗死极易引起颅内压增高,甚至可导致脑移位和脑疝,是致死和致残的主要原因之一。20世纪80年代末有学者主张采用标准外伤大骨瓣开颅术治疗重型颅脑损伤,随后在国内得到广泛的临床应用[14]。已有大量研究表明,传统标准大骨瓣减压术能显著降低颅内压,但其脑组织血供重建效果较差[15-17],故本研究采用标准大骨瓣减压联合脑-硬脑膜-肌肉血管重建术治疗重症颅脑损伤,旨在降低患者颅内压的同时改善脑组织血供。
本研究发现,试验组术后1周及术后1个月时的CBF、CBV明显高于对照组,MTT、TTP明显低于对照组。与传统术式比较,本研究采用的联合术式将硬脑膜的血管和带有血管的颞肌直接贴敷在受损的脑表面,使颞肌的血管和硬脑膜的血管与脑表面的血管融合,利用增生的毛细血管直接改善受损部位脑组织的血液循环,可在有效降低颅内压的基础上重建受损部位脑组织的血运,最大程度地促使受损部位脑组织的康复[18]。试验组术后1周与术后1个月时的rCBF、rCBV、rMTT、rTTP比较差异无统计学意义,而对照组术后1周时的rCBF、rCBV值高于术后1个月时,rMTT、rTTP低于术后1个月时。这主要是由于对照组微血管闭塞程度较高,血供恢复较差,微循环障碍随着时间的推移而加重,发生脑梗死的危险性增高,而试验组重建血供后脑组织微循环变化较小。试验组中恢复较好(包括良好和中残)的比例高于对照组,而恢复较差(包括重残、植物状态、死亡)的比例低于对照组,这进一步证实了联合术式的临床效果要优于传统标准术式,考虑是由于联合术式一方面降低了患者的颅内高压,另一方面改善了脑挫裂伤部位的缺血缺氧状态,减轻了脑水肿,降低了脑梗死的发生率,使脑功能得到最大程度的恢复,从而改善了预后,提高了患者的生存质量。
综上所述,标准大骨瓣减压联合脑-硬脑膜-肌肉血管重建术在降低重症颅脑损伤患者颅内压的同时能有效改善受损脑组织的血供,疗效显著,脑功能恢复程度高,预后较好,为重症颅脑损伤的有效治疗方法之一,值得临床应用及推广。
[1]Nemetz PN, Leibson C, Naessens JM,et al. Traumatic brain injury and time to onset of Alzheimer's disease: a populationbased study[J]. Am J Epidemiol, 1999, 149(1): 32-40.
[2]Magone MT, Kwon E, Shin SY. Chronic visual dysfunction after blast-induced mild traumatic brain injury[J]. J Rehabil Res Dev, 2014, 51(1): 71-80.
[3]Asha'Ari ZA, Ahmad R, Rahman J,et al. Contrecoup injury in patients with traumatic temporal bone fracture[J]. J Laryngol Otol, 2011, 125(8): 781-785.
[4]Li X, Li B, Yang L,et al. Clinical application of invasive intracranial pressure monitoring after severe traumatic brain injury[J]. Med J Chin PLA, 2011, 36(12): 1323-1325.[李侠, 李兵, 杨黎, 等. 重型颅脑损伤术后有创颅内压监测的临床应用[J]. 解放军医学杂志, 2011, 36(12): 1323-1325.]
[5]Bian AM. Experience of decompressive craniectomy[J]. Prac J Card Cereb Pneumal Vasc Dis, 2003, 11(5): 319-320.[卞爱苗. 对去骨瓣减压的几点体会[J]. 实用心脑肺血管病杂志, 2003, 11(5): 319-320.]
[6]Li DB, Song DL, Gu YX,et al. Preliminary clinical study of combined extra-intracranial feeding arteries reconstruction for severe middle cerebral artery stenosis or occlusion[J]. Chin J Neurosurg Dis Res, 2009, 8(2): 161-165.[李东波, 宋冬雷, 顾宇翔, 等. 脑供血动脉联合重建术治疗大脑中动脉重度狭窄或闭塞[J]. 中华神经外科疾病研究杂志, 2009, 8(2): 161-165.]
[7]Zhang J, Wang JH, Geng DY,et al. 256-slice whole-brain CT perfusion in assessment of graft reperfusion after surgical revascularization and hemodynamic alterations before and after surgery in Moyamoya disease[J]. Chin J Radiol, 2011, 45(8): 743-746.[张军, 王剑虹, 耿道颖, 等. 采用256层CT全脑灌注研究烟雾病术后桥血管再通及手术前后脑血流动力学的变化[J]. 中华放射学杂志, 2011, 45(8): 743-746.]
[8]Kilbaugh T, Karlsson M, Byro M,et al. Mitochondrial bioenergetic alterations after focal traumatic brain injury in the immature brain[J]. Exp Neurol, 2015, 271: 136-144.
[9]Mioni G, Rendell PG, Terrett G,et al. Prospective memory performance in traumatic brain injury patients: a study of implementation intentions[J]. J Int Neuropsychol Soc, 2015, 21(4): 305-313.
[10] Daradkeh G, Essa MM, Al-Adawi SS,et al. Nutritional status, assessment, requirements and adequacy of traumatic brain injury patients[J]. Pak J Biol Sci, 2014, 17(10): 1089-1097.
[11] Lequerica A, Jasey N, Portelli TJN,et al. Pilot study on the effect of ramelteon on sleep disturbance after traumatic brain injury (TBI): preliminary evidence from a clinical trial[J]. Arch Phys Med Rehabil, 2015, pii: S0003-9993(15)00423-2.
[12] Yang J, Korley FK, Dai M,et al. Serum neurogranin measurement as a biomarker of acute traumatic brain injury[J]. Clin Biochem, 2015, 48(13-14): 843-848.
[13] Yu CC, Duan GS, Yu XG,et al. Tentorial hernia intracranial vascular occlusion[J]. Chin J Neurosurg, 1995, 11(4): 241.[于朝春, 段国升, 余新光, 等. 小脑幕裂孔疝致颅内血管闭塞[J]. 中华神经外科杂志, 1995, 11(4): 241.]
[14] Jiang JR. Introduction of a US clinical commonly used standard large trauma craniotomy[J]. Chin J Neurosurg, 1998, 14(6): 58.[江基尧. 介绍一种美国临床常用的标准外伤大骨瓣开颅术[J]. 中华神经外科杂志, 1998, 14(6): 58.]
[15] Bowers CA, Riva-Cambrin J, Hertzler DA 2nd,et al. Risk factors and rates of bone flap resorption in pediatric patients after decompressive craniectomy for traumatic brain injury[J]. J Neurosurg Pediatr, 2013, 11(5): 526-532.
[16] Sadowski C, Lübbeke A, Saudan M,et al. Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or a 95 degrees screw-plate: a prospective, randomized study[J]. J Bone Joint Surg Am, 2002, 84-A(3): 372-381.
[17] Jasielski P, Glowacki M, Czernicki Z. Decompressive craniectomy in trauma: when to perform, what can be achieved[J]. Acta Neurochir Suppl, 2013, 118: 125-128.
[18] Ho KM, Honeybul S, Yip CB,et al. Prognostic significance of blood-brain barrier disruption in patients with severe nonpenetrating traumatic brain injury requiring decompressive craniectomy[J]. J Neurosurg, 2014, 121(3): 674-679.
Effect of large decompressive craniectomy combined with vascular reconstruction on cerebral perfusion in patients with severe brain injury
HUANG Liang-zhen, LIU Chao-hui, PENG Hao, ZHAO Jian-nong*
Department of Neurosurgery, People's Hospital of Hainan Province, Haikou 570311, China
*< class="emphasis_italic">Corresponding author, E-mail: zjn@vip.163.com
, E-mail: zjn@vip.163.com
This work was supported by the Natural Science Foundation of Hainan Province (20158349) and the Medical and Health Research Foundation of Hainan Province (1424320.27A2008)
ObjectiveTo compare the efficacies of large decompressive craniectomy combined with vascular reconstruction and traditional decompressive craniectomy in treatment of severe brain injury.MethodsForty-eight patients with severe brain injury, which was dominated by brain contusion to the frontoparietal lobes, admitted to our hospital from March 2012 to March 2014 were divided equally into experimental group and control group. The patients in the experimental group underwent large decompressive craniectomy combined with vascular reconstruction, and the patients in the control group
traditional decompressive craniectomy. The hemodynamic changes including cerebral blood flow (CBF), cerebral blood volume (CBV), mean transit time (MTT), time to peak (TTP) and the ratios of these values (rCBF, rCBV, rMTT and rTTP) on two sides were observed by CT perfusion imaging, and the Glasgow outcome score (GOS) was analyzed 6 months after operation.ResultsThe CBF and CBV scores in experimental group were higher than those in the control group at 1 week and 1 month after the operation (P<0.05). The MTT and TTP scores in the experimental group were lower than those in the control group at 1 week and 1 month after the operation (P<0.05). The rCBF and rCBV values were higher in 1 week than in 1 month, while the rMTT and rTTP values were lower in 1 week than in 1 month in the control group (P<0.05), while there was no statistical difference in rCBF, rCBV, rMTT and rTTP between 1 week and 1 month in the experimental group (P>0.05). The rate of satisfactory recovery (including good recovery and moderate disability) was higher in the experimental group than in the control group, while the rate of poor recovery (includingsevere disability, vegetative state and death) was lower in the experimental group than in the control group (P<0.05).ConclusionThe large decompressive craniectomy combined with vascular reconstruction can not only decrease the intracranial pressure, but also recover the blood supply of brain, thus deserving the clinical application and popularization.
craniocerebral trauma; decompressive craniectomy; cerebral revascularization; perfusion imaging
R651.15
A
0577-7402(2015)11-0934-04
10.11855/j.issn.0577-7402.2015.11.15
2015-06-07;
2015-09-25)
(责任编辑:胡全兵)
海南省自然科学基金(20158349);海南省医药卫生科研项目(1424320.27A2008)
黄良珍,副主任医师。主要从事颅内肿瘤、脑血管病、高血压脑出血、颅脑损伤的临床治疗工作
570311 海口 海南省人民医院神经外科(黄良珍、刘朝晖、彭浩、赵建农)
赵建农,E-mail:zjn@vip.163.com