ICU内获得性感染细菌谱的时间分布分析
2015-01-02
(中国医科大学附属盛京医院重症医学科,沈阳 110004)
ICU内获得性感染细菌谱的时间分布分析
汪海源,洪涛,吴兴茂,臧彬
(中国医科大学附属盛京医院重症医学科,沈阳 110004)
目的系统性回顾中国医科大学附属盛京医院入住重症医学科(ICU)患者48 h后细菌谱的时间分布规律,为ICU内感染早期抗生素的应用提供临床参考。方法收集2012年1月至2013年3月期间于中国医科大学附属盛京医院ICU病房治疗的患者共1 330例,其中阳性细菌培养结果患者254例,共收集病原菌1 110株,排除入住ICU病房48 h内检出病原菌288株,同一患者培养出相同病原菌者共222株。最后纳入统计的病原菌为600株。结果ICU内获得性感染率为19.1%,其中术后患者占74.3%,以腹部、脑外、骨科术后感染发生率最高。肺部感染占ICU内获得性感染的首位(40.3%),其次为血源性感染(25.3%),术后引流管内(14.2%)及尿管(7.3%)感染。入住ICU第1周内病原菌检出率最高,随着时间进展病原菌检出率逐渐降低。ICU病房内感染菌株以鲍曼不动杆菌、铜绿假单胞菌、肺炎克雷伯菌及屎肠球菌为主,任何时间均以革兰阴性杆菌占主导地位(73.8%)。另外,第2周真菌感染率上升。结论ICU内获得性感染的防治应以革兰阴性杆菌为主,随着ICU住院时间的延长,条件致病菌的比率逐渐上升,主要为非发酵菌。真菌感染在患者入住ICU第2周发生的可能性最大。
重症医学科;感染;细菌
重症医学科(intensive care unit,ICU)病房收治的患者病情危重,常合并多种并发症,免疫力低下,同时因疾病诊治的需要通常需行较多的有创操作,导致ICU内获得性感染的发生率明显高于院内感染(25%vs 5%~10%)[1]。现已公认的ICU内获得性感染的危险因素包括ICU入住时间、机械通气时间、中心静脉导管、气管导管或尿管的置入、创伤、急诊手术等。其中ICU内获得性肺炎、脓毒血症、血源性感染会明显增加患者的ICU死亡率[1,2]。因此,掌握不同时间段内占主导地位的优势病原菌谱,尽早地预防性使用抗生素是降低ICU感染率及死亡率的有效方法[2]。本研究系统性回顾了入住我院ICU患者48 h后细菌谱的分布规律,旨在为ICU内早期抗生素的应用提供借鉴。
1 材料与方法
1.1 一般资料
收集2012年1月至2013年3月期间于中国医科大学附属盛京医院ICU病房接受治疗的病例,共1 330例。其中,已排除年龄<18岁及入住ICU病房24 h内死亡的患者。同一患者重复入住ICU病房按照新病例计算。
排除48 h内细菌培养阳性患者,共收集细菌培养结果阳性患者254例。记录ICU内感染患者的年龄、性别、入住ICU病房时ApacheⅡ评分、入住原因等基本信息。
共收集病原菌1 110株,排除入住ICU病房48 h内检出病原菌288株及同一患者培养出相同病原菌者222株,最后纳入统计的病原菌为600株。
1.2 标本采集及病原菌培养
使用无菌痰液收集器或纤维支气管镜收集气管切开或置入气管导管患者下呼吸道分泌物;使用无菌注射器收集留置导尿管、手术引流管的体液;采集外周静脉血行血细菌培养;使用无菌痰液收集器收集拔除的中心静脉导管尖端后送检。所收集的标本由我院检验科负责检验,不同的标本按照要求各自行培养、分离及鉴定。
1.3 统计学分析
所有数据采用SPSS 13.0统计学软件进行分析。
2 结果
2.1 ICU内感染患者的一般情况
1 330例患者中,发生ICU内感染患者254例,ICU内获得性感染率为19.1%,其中57.7%的患者出现2株以上的病原菌感染。ICU内获得性感染患者中,100%为尿管置入,53.9%为中心静脉置入,93.3%为机械通气。术后患者占74.3%,以腹部、脑外科、骨科手术后感染发生率最高。见表1。
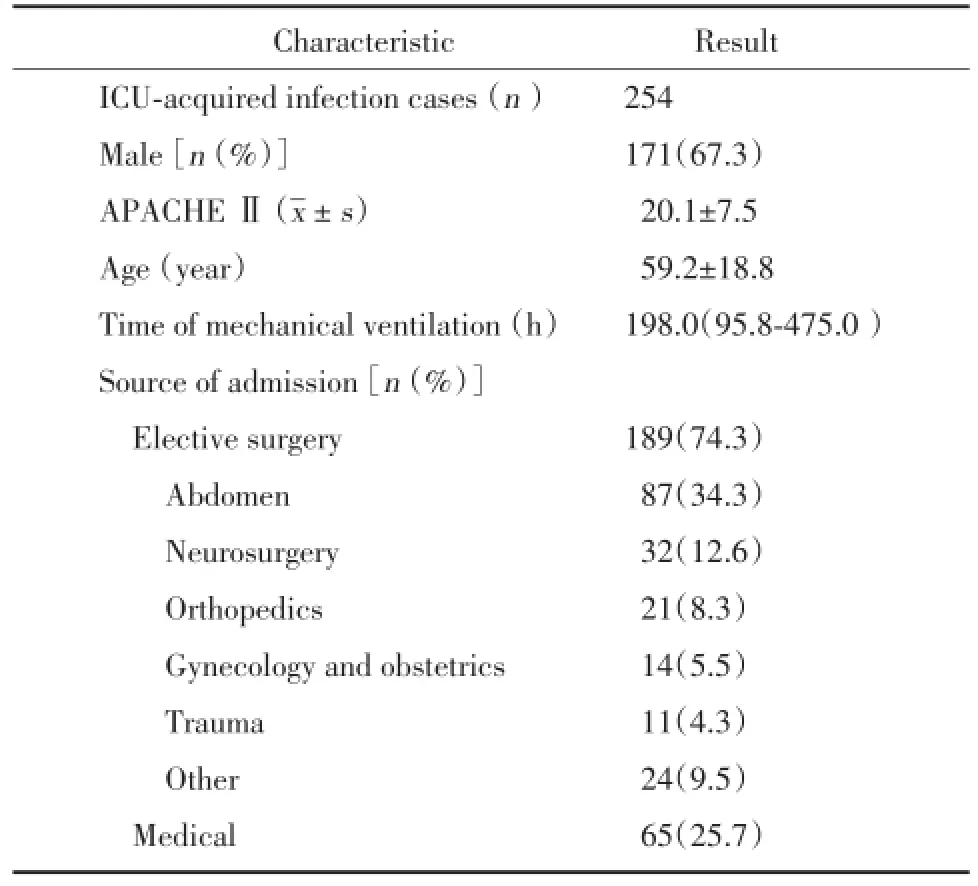
表1 ICU内感染患者的一般情况Tab.1 The general conditions of patients with ICU-acquired infections
2.2 ICU内获得性感染部位
肺部是ICU内获得性感染的首要部位,占40.3%,其次为血源性感染(25.3%),术后引流管内(14.2%)及尿管(7.3%)感染,见表2。第1周内病原菌检出率最高,其后随着时间进展病原菌检出率逐渐降低,至第4周时基本无病原菌检出。
2.3 ICU内获得性感染病原菌
在第1周内(2~7 d),ICU内获得性感染主要病原菌为鲍曼不动杆菌(31.4%)、铜绿假单胞菌(11.0%)、肺炎克雷伯菌(10.6%)、屎肠球菌(10.2%)及金黄色葡萄球菌(8.6%)。第2周内,主要病原菌为鲍曼不动杆菌(40.4%)、铜绿假单胞菌(12.5%)、屎肠球菌(10.6%)、肺炎克雷伯菌(6.7%)及近平滑假丝酵母(5.8%)。第3周内,主要病原菌为鲍曼不动杆菌(38.9%)、铜绿假单胞菌(22.2%)、肺炎克雷伯菌(5.6%)、屎肠球菌(5.6%)、真菌(5.6%)。4周后主要病原菌为鲍曼不动杆菌(26.3%)、铜绿假单胞菌(18.0%)、肺炎克雷伯菌(10.5%)、大肠埃希菌(8.8%)和屎肠球菌(7.0%)。可见在ICU病房内感染菌株始终以鲍曼不动杆菌、铜绿假单胞菌、肺炎克雷伯菌及屎肠球菌为主,以革兰阴性杆菌占主导地位。第1周内出现感染病原菌最多,后逐渐减少。第2周时出现真菌感染的上升趋势。
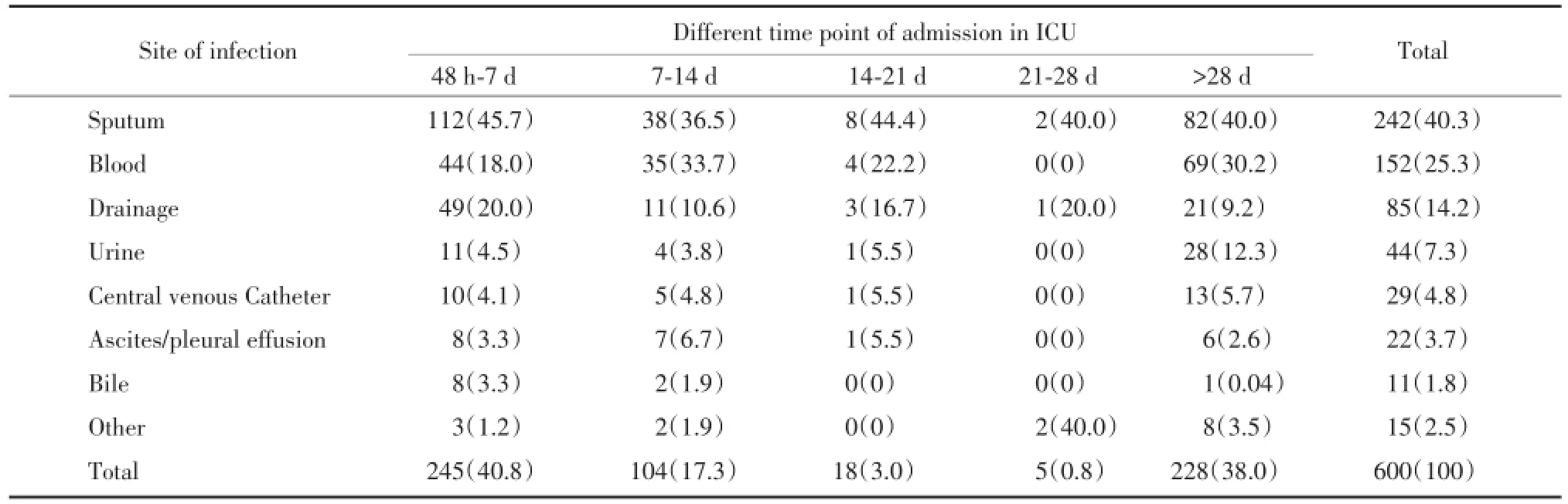
表2 不同来源病原菌的时间分布及构成比[n(%)]Tab.2 Time distribution and constituent ratio of different sources of pathogenic bacteria[n(%)]
28 d内检出病原菌株共372例,占总标本的62%。28 d后收集病原菌株共228例,占总标本的38%,最长收集时间为425 d。

表3 ICU内获得性感染细菌谱的时间分布[n(%)]Tab.3 The time distribution of bacteria of ICU-acquired infections[n(%)]
3 讨论
作为院内感染的一种,ICU获得性感染与普通专科病房的院内感染有所不同。ICU患者因病情危重,住院时间长,侵袭性操作多,使用生命支持装备以及存在多重耐药菌,导致ICU的院内感染较普通病房更普遍[3]。ICU患者来源较为复杂,包括急诊患者、外科术后患者、内科经治疗后病情加重患者、入ICU前未曾及已应用抗生素治疗患者。即使在ICU已经行抗生素治疗,一部分患者因免疫力下降以及各种解剖屏障、生物屏障破坏,还会随着住院时间的延长而出现新发感染,而微生物室对于病原菌的获取、保存、转运、分离和鉴定有严格的规定[4],在时间上存在滞后,对于中重度感染的危重患者往往会出现初始抗生素治疗不充分。较早即有文献提出,初始抗生素治疗的不充分性对于患者的预后有极其不利的影响[5~10],因此有必要对ICU获得性感染的细菌谱进行入ICU后时间上的归纳分析,以便为临床上抗生素的使用及调整提供参考。
虽然患者来源不同,但大部分ICU患者为外科患者,尤其是术后患者(74.3%),其肺内感染比重最高,究其原因与患者年龄、麻醉后气道的开放、较长的机械通气时间和术后患者长时间卧床有关[11]。送检样本中,病原菌检出率前4位分别为痰液、血液、术后引流液及尿液,痰液在不同时间段检出病原菌始终最多,与文献报道相近[12,13];血液检出病原菌比重次之,原因可能与中心静脉导管的留置[14]和腹部手术、妇产科手术及创伤手术较多,且大部分为Ⅱ类切口甚至Ⅲ类切口,病原菌容易入血有关;在入ICU 48 h至7 d,检出病原菌样本中术后引流液占20%,仅次于痰液,究其原因仍然与创伤及感染部位手术有关[15];对于入住ICU超过28 d的患者,总体比重处于第4位的尿液却超过引流液而居于第3位,原因可能为这部分患者绝大多数为神经系统疾病或者疾病长期迁延不愈而导致长时间留置尿管,进而出现尿液检出病原菌增多[16]。
对于检出病原菌的时间分布,随着住院时间的延长,总体上呈递减趋势,前4周即检出所有病原菌的60%以上,与抗生素的应用有密切的关系。检出病原菌中按所占比重来看仍然以革兰阴性杆菌为主,占7成以上,分离前5位病原菌分别为鲍曼不动杆菌、铜绿假单胞菌、肺炎克雷伯菌、屎肠球菌及大肠埃希菌,与既往的文献比较,细菌谱变化较大[17],分析原因与病原菌耐药性的变化有关[18]。入住ICU 48 h以后不论何时,检出鲍曼不动杆菌和铜绿假单胞菌的可能性可达40%以上。肺炎克雷伯菌、屎肠球菌和大肠埃希菌主要在入住ICU前2周检出,占总体检出的50%以上。尤其需要注意的是,在入住ICU第2周,真菌的检出率比其他时间段都要多,以近平滑假丝酵母为主,考虑原因与中心静脉导管的留置有关[19]。
[1]Trilla A.Epidemiology of nosocomial infections in adult intensive care units[J].Intensive Care Med,1994,20(suppl 3):S1-S4.
[2]Lambert ML,Suetens C,Savey A,et al.Clinical outcomes of healthcare-associated infections and antimicrobial resistance in patients admitted to European intensive-care units:a cohort study[J].Lancet Infect Dis,2011,11(1):30-38.
[3]Erdem H,Inan A,Carevic B,et al.Surveillance,control and management of infections in intensive care units in Southern Europe,Turkey and Iran-a prospective multicenter point prevalence study[J].J Infect,2014,68(2):131-140.
[4]Baron EJ,Miller JM,Weinstein MP,et al.A guide to utilization of the microbiology laboratory for diagnosis of infectious diseases:2013 recommendations by the Infectious Diseases Society of America(IDSA)and the American Society for Microbiology(ASM)[J]. Clin Infect Dis,2013,57(4):485-488.
[5]Barochia AV,Cui X,Vitberg D,et al.Bundled care for septic shock:an analysis of clinical trials[J].Crit Care Med,2010,38(2):668-678.
[6]Kumar A,Zarychanski R,Light B,et al.Early combination antibiotic therapy yields improved survival compared with monotherapy in septic shock:a propensity-matched analysis[J].Crit Care Med,2010,38(9):1773-1785.
[7]Micek ST,Welch EC,Khan J,et al.Empiric combination antibiotic therapy is associated with improved outcome against sepsis due to Gram-negative bacteria:a retrospective analysis[J].Antimicrob Agents Chemother,2010,54(5):1742-1748.
[8]Martínez JA,Cobos-Trigueros N,Soriano A,et al.Influence of empiric therapy with a beta-lactam alone or combined with an aminoglycoside on prognosis of bacteremia due to gram-negative microorganisms[J].Antimicrob Agents Chemother,2010,54(9):3590-3596.
[9]Levy MM,Dellinger RP,Townsend SR,et al.The Surviving Sepsis Campaign:results of an international guideline-based performance improvement program targeting severe sepsis[J].Crit Care Med,2010,38(2):367-374.
[10]Gurnani PK,Patel GP,Crank CW,et al.Impact of the implementation of a sepsis protocol for the management of fluid-refractory septic shock:A single-center,before-and-after study[J].Clin Ther,2010,32(7):1285-1293.
[11]蔡小晖.气管插管全麻术后医院内肺部感染的危险因素分析[J].中华医院感染学杂志,2011,21(9):1780-1782.
[12]Barbier F,Andremont A,Wolff M,et al.Hospital-acquired pneumonia and ventilator-associated pneumonia:recent advances in epidemiology and management[J].Curr Opin Pulm Med,2013,19(3):216-228.
[13]Rosenthal VD,Bijie H,Maki DG,et al.International Nosocomial Infection Control Consortium(INICC)report,data summary of 36 countries,for 2004-2009[J].Am J Infect Control,2012,40(5):396-407.
[14]Al Mohajer M,Darouiche RO.Sepsis syndrome,bloodstream infections,and device-related infections[J].Med Clin North Am,2012,96(6):1203-1223.
[15]Petersen K,Waterman P.Prophylaxis and treatment of infections associated with penetrating traumatic injury[J].Expert Rev Anti Infect Ther,2011,9(1):81-96.
[16]Chenoweth C,Saint S.Preventing catheter-associated urinary tract infections in the intensive care unit[J].Crit Care Clin,2013,29(1):19-32.
[17]Doyle JS,Buising KL,Thursky KA.Epidemiology of infections acquired in intensive care units[J].Semin Respir Crit Care Med,2011,32(2):115-138.
[18]Fraimow HS,Tsigrelis C.Antimicrobial resistance in the intensive care unit:mechanisms,epidemiology,and management of specific resistant pathogens[J].Crit Care Clin,2011,27(1):163-205.
[19]Pappas PG,Kauffman CA,Andes D,et al.Clinical practice guidelines for the management of candidiasis:2009 update by the Infectious Diseases Society of America[J].Clin Infect Dis,2009,48(5):503-535.
(编辑王又冬)
Analysis of Bacterial Time Distribution of ICU-acquired Infections
WANGHai-yuan,HONGTao,WUXing-mao,ZANGBin
(Department of Critical Care Medicine,Shengjing Hospital,China Medical University,Shenyang 110004,China)
Objective To retrospectively analyze bacterial time distribution of IC U-acquired infections in Shengjing Hospital of China Medical University,so as to provide reference for the early antibiotic use for ICU-acquired infections.MethodsA total of 1 330 cases in ICU from Jan.2012 to Mar.2013 were collected,the bacterial culture was positive in 254 cases.A total of 1 110 strains were collected from all the patients.Excluding 288 strains which were detected within 48 hours of patients′admission in ICU and 222 strains which were repeatedly detected in the same patients,600 strains were finally enrolled in the statistical analysis.ResultsThe rate of ICU-acquired infections was 19.1%.Postoperative infections accounted for 74.3%,most of which occurred after neurosurgeries,and abdominal,orthopedic operations.Pulmonary infection ranked the first in ICU-acquired infections,accounting for 40.3%,followed by blood stream infection(25.3%),postoperative drainage infection(14.2%)and urinary tract infection(7.3%).The rate of pathogenic bacteria detection was the highest in the first week of patients′admission in ICU,and was getting lower as time went by.Strains detected in ICU mainly were Bauman Acinetobacter,Pseudomonas aeruginosa,Klebsiella pneumonia and Enterococcus faecium,most of strains resulting in infections were gram negative bacilli throughout the time.In addition,the infection rate of fungi was increased at 2 weeks of patients′admission in ICU.ConclusionThe treatment of ICU-acquired infections should be targeted atgram negative bacilli.The detection rate of opportunistic pathogens gradually increased with prolonged stay in ICU,most of which are non-fermentative bacteria.Fungi infections are most likely to occurat2 weeks of patients′admission in ICU.
intensive care unit;infection;bacteria
R446.1
A
0258-4646(2015)05-0434-04
汪海源(1978-),男,主治医师,硕士.
臧彬,E-mail:zangb@sj-hospital.org
2014-10-16
网络出版时间:
