感染肠道病毒71型14例死亡病例病理特征与临床分期反思
2013-12-26欧维琳李佩青李坤雄李运千熊雨美农光民杨思达
韦 丹 蒋 敏 欧维琳 李佩青 李坤雄 李运千 陈 娥 熊雨美 农光民 杨思达
·论著·
感染肠道病毒71型14例死亡病例病理特征与临床分期反思
韦 丹1,5蒋 敏1,5欧维琳2,5李佩青3,5李坤雄1李运千2陈 娥4熊雨美3农光民1杨思达3
目的 观察肠道病毒71型(EV71)感染死亡病例临床演变过程,探讨EV71神经损伤途径,反思EV71感染重症病例临床救治专家共识(简称专家共识)的临床分期。方法 回顾性收集2008至2010年广西9所医院(12例)和2011至2012年广州市妇女儿童医疗中心(2例)EV71感染死亡病例,描述分析14例EV71感染死亡病例尸解病理特征与临床症状、病程特点。结果 14例EV71感染死亡病例,男7例,女7例,年龄7~36月龄,平均(19.0±9.8)月龄。14例EV71感染死亡病例均见脑干筛状坏死及软化灶形成,10例累及延髓,肺、心和其他脏器病理未见炎性细胞浸润。专家共识中10个(35.7%)症状和体征未被发现或记录,4期的惊厥与2期症状同时出现,4期的意识障碍在2期的抖动后出现,起病后48 h以内可观察到的症状和体征有,发热、皮疹、呕吐、惊跳、惊厥、疲倦、咽峡炎和抖动。分别有42.9%(6/14)的EV71感染重症病例2~4期症状与体征于12 h内和48 h内体现,直至死亡。12例EV71感染死亡病例中从发热至死亡平均为72.4 h,从基础生命体征(3期症状体征)出现异常(平均65.5 h)至死亡为6.9 h,从出现自主等神经系统症状(2期症状体征平均39.8 h)至死亡为32.6 h。结论 ①EV71感染病例直接死亡原因为脑干器质性破坏后功能衰竭;②推测EV71存在神经损伤通路;③神经专科评估特异性指标应作为EV71感染病例必要的过程;④惊厥可列入 EV71感染早期后神经损伤的观察指标中,对意识障碍进行具体分级并相应表述于专家共识的不同分期中;⑤建议结合神经专科评估特异性指标,进行更充分的临床分期高质量的研究,为临床医生提供相对充分的观察和干预时间窗口。
肠道病毒71型; 神经损伤; 病程; 尸解; 临床分期
肠道病毒71(EV71)由Kennett等[1]首次报道。目前已知EV71可引起多种神经系统相关疾病[2],继发严重的CNS并发症或致死性肺水肿[3~11]。近年来,EV71的流行在亚太地区呈上升趋势,1998年,中国台湾地区暴发手足口病,12万以上居民被感染,死亡78例,其中检出病原为EV71达92% (34/37)[12];2008年中国广东地区手足口病暴发,其中广州地区EV71的检出率为63.6%[13];2008至2012年中国广西地区也有手足口病的暴发。
EV71所致手足口病的研究受到国内外的关注[14~16],逐渐明确脑干是EV71主要的攻击靶点[17]。国内经历近5年手足口病危重症救治,EV71感染重症病例临床救治专家共识(简称专家共识)先后产生了多个版本,对早期识别EV71感染重症病例起到了非常重要的影响,但EV71感染重症病例的临床症状和体征变化快,难以把握,本文收集EV71感染死亡病例的病理和临床资料,以2011年版专家共识中临床分期的症状和体征作为观察指标,反思专家共识中临床分期对早期发现重症手足口病的有利与不利因素。
1 方法
1.1 病例纳入标准 ①咽拭子、粪便或肛拭子标本,RT-PCR法检测EV71阳性。②EV71感染死亡病例。③死亡病例于48 h内病理专科医生进行尸解。
1.2 资料收集方法 ①尸体解剖以分系统大体病理和镜下病理归纳描述;②以专家共识中临床分期的症状和体征作为观察指标(1期:发热、皮疹、咽峡炎、纳差、上感样症状,2期:精神差、嗜睡、易惊、头痛、呕吐、烦燥、抖动、疲倦、惊跳、颈强直,3期:呼吸和心率加快、出冷汗、皮肤花纹、四肢冷,4期:心动过速/过缓、呼吸急速、唇发绀、肺出血、休克、频繁抽搐、意识障碍、死亡),以就诊时发热主诉作为EV71感染起病的起点,高年资的儿科医生重新调阅纳入分析的死亡病历,在统一设计的表格中以小时为单位统计上述观察指标出现时间,直至抢救不能挽回至死亡的时点。
1.3 病原学检测 采集的咽拭子、粪便或肛拭子棉签,迅速放入装有3~5 mL保存液的配套采样管中,旋紧管盖并密封待检测。样品检测采用RT-PCR法(美国ABI 7500实时荧光定量PCR仪),检测试剂盒为Rneasy Mini Kit(德国QIAGEN公司),按照试剂盒说明书操作。结果判定标准:检测样本Ct值>30为阴性;Ct值≤30,为阳性结果。
2 结果
2.1 一般情况 12例EV71感染死亡患儿来自于2008年5月至2010年7月广西壮族自治区9所县市级医院,死亡病例分别由广西医科大学和桂林医学院病理教研室尸检;2例EV71感染死亡患儿来自于2011年9月至2012年4月广州市妇女儿童医疗中心,死亡病例由广州医学院病理教研室尸检。14例EV71感染死亡患儿,男7例,女7例,死亡时的平均年龄为7~36(19.0±9.8)月龄,其中0~1岁5例(35.7%),~3岁9例(64.3%)。
2.2 尸解所见
2.2.1 大体解剖所见 脑干水肿,大脑及脑干切面未见出血、坏死,未见脑疝(图1A);肺脏可见两肺质地较实,肺切面均见较多泡沫状或淡红色液体溢出。
2.2.2 镜下脑病理改变 均见脑干筛状坏死及软化灶形成(图1B),10例延髓可见神经细胞坏死及筛状软化灶,伴有较多小胶质细胞浸润,可见噬神经细胞现象和胶质小结形成(图1C~E),间质小血管扩张充血,均见血管周围有较多淋巴细胞、单核细胞浸润呈“袖套状”(图1F)改变,较多细小的嗜酸性颗粒(图1G);小脑部分蒲倾野氏细胞可见变性、坏死,未见炎细胞浸润(图1H)。
2.2.3 镜下心、肺和其他脏器病理改变 肺脏:均可见肺泡壁增厚,间质纤维组织增生,血管轻度扩张、充血,肺泡腔内见粉红色或淡染均质水肿液(图1I),3例伴有少量淋巴细胞、单核细胞及巨噬细胞浸润, 2例有少量透明膜形成(图1J)。心脏:13例无心肌坏死及12例无炎细胞浸润,间质轻度充血、水肿,未见出血(图1K);1例心肌见少量淋巴细胞、单核细胞浸润;1例出现神经系统症状117 h死亡的病例尸解可见心肌纤维局部有小灶性的变性坏死。其他脏器(如肝、脾、肾、肾上腺、胰、胸腺和胃肠道等)均未见明显病理改变。
2.3 临床表现 专家共识中共涉及28个症状和体征,本组14例EV71感染死亡病例中,专家共识中10个(35.7%)症状和体征未被发现或记录,包括1期:纳差、上感样症状,2期:精神差、嗜睡、头痛、烦燥、颈强直,3期:出冷汗、皮肤花纹,4期:唇发绀。表1显示,以就诊时发热主诉作为EV71感染起病时点,被发现或记录的专家共识中症状和体征出现时间顺序为:发热14例(1期,0 h)、皮疹9例(1期,18 h)、呕吐11例(2期,29 h ) 、惊跳6例 (2期,36 h)、惊厥8例(4期,42 h)、疲倦12例(2期,46 h)、咽峡炎3例(1期,48 h)、抖动8例(2期,48 h)、意识障碍12例(4期,58 h)、呼吸加快11例(3期,64 h )、 心率加快10例(3期,65 h)、四肢冷13例(3期,67 h)、休克11例(4期,74 h)、肺出血14例(4期,74 h)、呼吸减慢10例(4期,76 h)、心率减慢10例(4期,80 h)、肺水肿7例(4期,81 h)。9/14例(64.3%)4期的惊厥症状与2期症状同时出现,11/14例(78.6%)4期的意识障碍在2期抖动症状后出现,起病后48 h以内可观察到的症状和体征有,发热、皮疹、呕吐、惊跳、惊厥、疲倦、咽峡炎和抖动。分别有6/14例(42.9%)的EV71感染重症病例2~4期症状与体征于12 h内和48 h内先后、同时或交替出现,直至死亡,其中例10以1期发热与4期抽搐起病,随后其他3、4期症状同时出现,2 h后死亡。
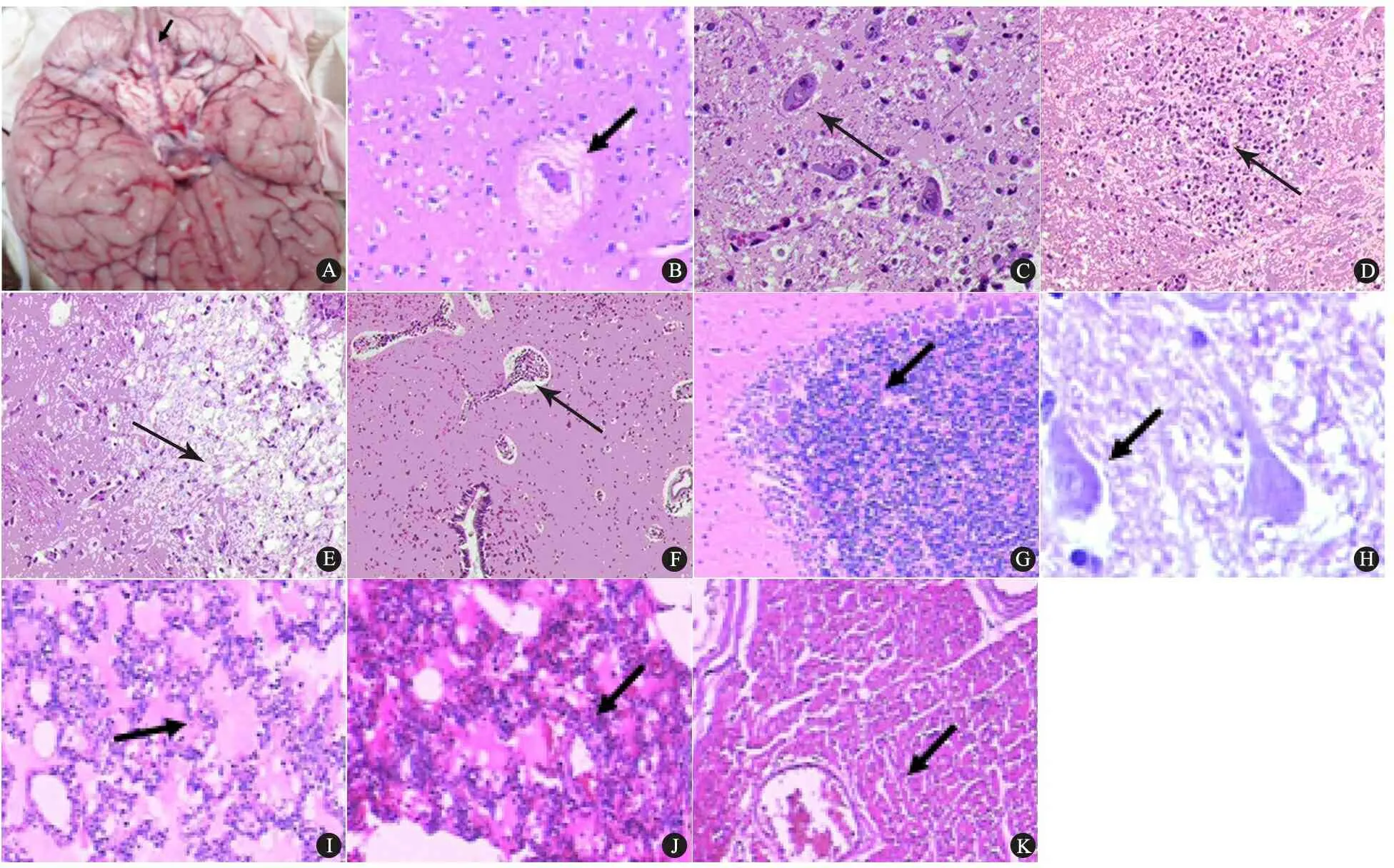
图1 EV71感染死亡病例大体解剖和病理(苏木精-伊红染色)所见
Fig 1 Gross and micrographs of unsurvival enterovirus 71 infection cases (stained with hematoxylin and eosin)
Notes A: Autopsy revealed edema in brain stem; B: dilation of blood vessels and neuronal and perivascular area widened (×100); C: neuronophagia phenomenon (×400); D: colloid in the brain stem (×400); E: neuronal necrosis and softening in the brain stem (×100); F: perivascular cuffing in the brain stem (×200); G: small eosinophils (×200); H: neuronal degeneration and necrosis; I: pink fluid in the alveolar space (×200); J: hyaline membrane in the alveolar space (×200); K: mild congestion and edema without inflammation and necrosis (×200)
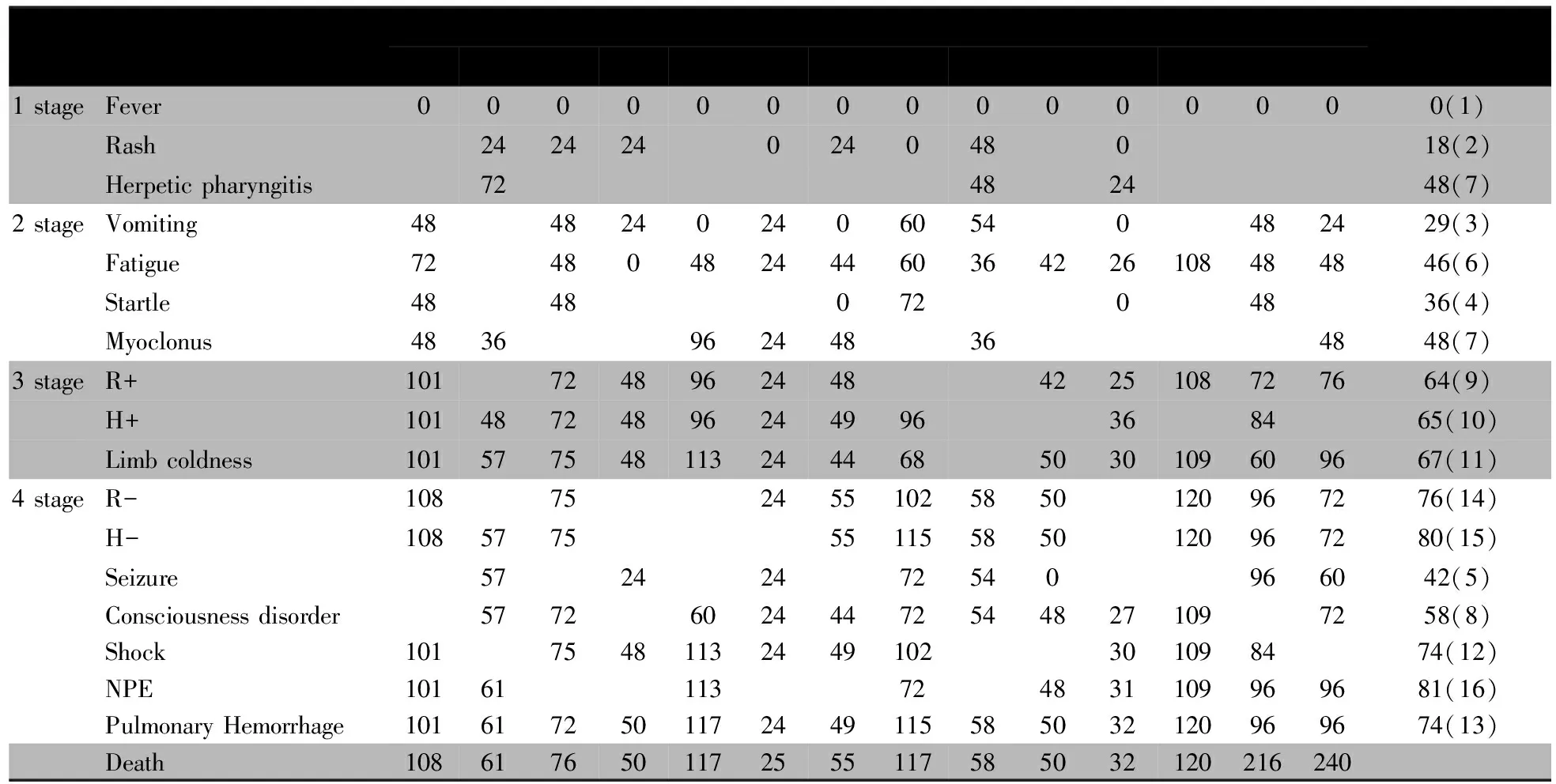
表1 14例EV71感染死亡病例症状和体征出现时间(h)及排序
本文2例在高级生命支持下至放弃治疗持续9和10 d。7例(50%)EV71感染重症病例起病72 h内死亡,5例(35.8%)起病120 h内死亡,这12例EV71感染死亡病例中从发热至死亡平均时间为72. 4 h,从基础生命体征(3期症状体症)出现异常(平均65.5 h)至死亡为6.9 h,从出现自主等神经系统症状(2期症状体征平均39.8 h)至死亡为32.6 h。
3 讨论
本文14例EV71感染死亡病例均见脑干筛状坏死及软化灶形成,10例累及延髓,肺、心和其他脏器病理未见炎性细胞浸润。咽拭子、粪便或肛拭子标本RT-PCR法检测EV71阳性,但未行累及脏器病原学检测,因此说明本组死亡病例与EV71感染关联性很强,以此为基础的对专家共识中各期症状和体征出现时间顺序的统计,可较为真实地体现EV71感染至死亡的临床演变进程。
研究表明,EV71致中枢神经系统受累症状可理解为中脑、基底节、丘脑、脑干及自主神经功能紊乱症状[18~20],这些神经系统症状和体征在本组病例中均有不同程度的表达,尸解所见脑干筛状坏死,证实脑干为EV71攻击的靶位以及脑干功能衰竭为其主要死因[21~27],同时也证实EV71感染神经受累病例出现的神经系统外异常表现为神经源性反应。本组病例从发热至死亡时程平均94.6 h,其中例13和14高级生命支持了120~140 h后放弃,实际从发热至死亡平均时间75.7 h。尸解未见脑干外脏器原发性感染或基础疾病表现,考虑EV71存在神经通路损伤机制[28~36],可通过第3~12 对颅神经的运动神经逆行扩散影响脑干不同部位对应的神经核团,随后向上扩展至皮质延髓束及至大脑运动皮质[37~39]。
就EV71神经损伤病例而言,需进行神经专科评估,包括基础生命体征外的意识状态、瞳孔和神经反射。本组病例除放弃后死亡的例13和14外,12例EV71感染死亡病例从基础生命体征出现异常至死亡为6.9 h,基础生命体征异常时,机体已处在失代偿状态,可迅速进入死亡,为临床医生所留抢救干预的时间短速,降低病患良好存活的机会。这12例从出现自主等神经系统症状至死亡为32.6 h,与出现基础生命异常比较而言,出现自主等神经系统症状更能为临床医生提供相对充分的观察和干预时间窗口。结合本文死亡病例以脑干损害为主要表现,EV71感染重症病例更体现为神经系统的急性表现和重症表型。因此,对于早期发现重症病例一方面应进一步提炼较为特异的神经系统症状和体征,同时更应强调对早期EV71感染病例以神经专科的视角进行评估。
专家共识将EV71感染分为5期,1~4期的10个症状和体征在本组病例中未被发现或记录,可能与症状和体征未发生有关、也有可能与未被观察到有关、也有可能与临床医生不认知或判断不准确有关,专家共识2期未被记录到的头痛,可能受患儿年龄及意识水平等因素的限制未能准确表达,临床医生不能进行客观评估。2期未被记录到的嗜睡可能与专家共识中意识障碍定义和分级不清晰有关。
本组病例中有57.1%(8/14) 记录了惊厥, 专家共识中的4期惊厥(平均出现时间42 h)与2期症状几乎同时出现(平均出现时间39.8 h),4期的惊厥与2期的抖动、惊跳,虽然各自的神经定位及其临床表现不尽相同,但在本组病例中同时出现,加之惊厥发作影响因素不单一,将其纳入专家共识2期的观察指标中较为合理。
本组病例中有78.6%(11/14) 记录了意识障碍, 在专家共识中症状和体征出现时间顺序中仅次于与2期的抖动,2期抖动出现于48 h,4期意识障碍出现于58 h。临床对意识障碍有不同程度的表达,如轻度意识障碍可为意识模糊、疲倦和思睡;中度意识障碍可见嗜睡和谵妄;重度意识障碍表现为昏睡及各种程度的昏迷。 专家共识临床分期中,在2期有中度意识障碍的嗜睡表述,在4期有不分程度意识障碍表述,本组病例不排除将不同程度(轻度、中度、重度)的意识障碍均理解为意识障碍被记录。建议在专家共识分期中对意识障碍进行具体分级并相应表述于不同分期中。
本研究观察到的 EV71感染至死亡的临床演变进程,专家共识中1~4期症状体征可先后或同时出现,也可交替发生,个别病情进展凶猛患儿,在短期内呈现异常呼吸,脑干延髓呼吸中枢直接受到攻击,按专家共识的临床分期,患儿仅处于2期,提示专家共识中2和4期分期界限不够清晰, 或需更系统地观察和挖掘新的神经系统的症状与体征, 如颅神经症状和精神状态等;或提炼反映脑干受损神经系统特异指标在2期中表述,如中国台湾学者提出的脑干脑炎3级分法[38],Ⅰ级:脑干炎,全身性肌阵挛抽搐、震颤和共济失调,或两者兼而有之;Ⅱ级,颅神经受累,包括眼干扰,眼球震颤,斜视或凝视麻痹和延髓麻痹(构音障碍、吞咽困难、发音困难、面瘫肌阵挛);Ⅲ级,进展快,出现呼吸困难、发绀、周围血管灌注不良、休克、昏迷和眼睛反射消失等。对上述症状和体征的了解与熟悉,有利于临床医生认识及提早预警危重状态发生, 提高抢救成功率。当然合理和实用的EV71感染临床分期还有待于设计严密的、偏倚得到很好控制的高质量研究来体现。
本文的不足与局限:①本文虽然在 EV71感染症状与体征的统计上做了充分的准备, 从回顾性收集的病历资料中以高年资的儿科医生进行认真提炼, 但限于病情进展快(从 EV71感染至死亡时间平均75.7 h) ,或来自于10家县市级医院临床医生不认知或判断不准确,导致可能存在未被观察到的症状和体征, 或观察到的症状与体征不能做出准确的判断, 故本文仅为描述性的研究; ②本组尸解病例未行累及脏器病原学检测, 确切说明死亡病例与 EV71感染尚显不足。
[1]Kennett ML,Birch CJ,Lewis FA,et al. Enterovirus type 71 infection in Melbourne. Bull World Health Organ,1974,51:609-614
[2]Huang CC,Liu CC,Chang YC,et al. Neurologic complications in children with Enterovirus 71 infection. N Engl J Med,1999,341(13):936-942
[3]Alexander JP,Baden L,Pallansch MA,et al. Enterovirus 71 infections and neurologic disease- United States, 1977-1991. J In fect Dis,1994,169(4):905-908
[4]Ho M,Chen ER,Hsu KH,et al. An epidemic of enterovirus 71 infection in Taiwan. N Engl J Med,1999,341(13): 929-935
[5]Chen KT,Chang HL,Wang ST,et al.Epidemiologic features of hand -foot - mouth disease and herpangina caused by enterovirus 71 in Taiwan. 1998 - 2005. Pediatrics, 2007,120(2) : 244-252
[6]van der Sanden S, Koopmans M, Uslu G, et al. Epidemiology of enterovirus 71 in the Netherlands, 1963 to 2008. J Clin Microbiol, 2009 ,47(9): 2826-2833
[7]Ryu WS, Kang B, Hong J, et al. Clinical and etiological characteristics of enterovirus 71-related diseases during a recent 2-year period in Korea. J Clin Microbiol, 2010,48(7): 2490-2494
[8]McMinn P,Stratov I,Nagarajan L,et al. Neurological manifestations of enterovirus 71 infection in children during an outbreak of hand, foot, and mouth disease in Western Australia. Clin Infect Dis, 2001,32(2): 236-242
[9]Lum LC,Wong KT,Lam SK,et al. Neurogenic pulmonary oedema and enterovirus 71 encephalomyelitis. Lancet, 1998,352(9137):1391
[10]Shindarov LM,Chumakov MP,Voroshilova MK,et al. Epidemiological, clinical, and pathomorphological characteristics of epidemic poliomyelitis-like disease caused by enterovirus 71. J Hyg Epidemiol Microbiol Immunol,1979,23(3):284-295
[11]Ishimaru Y,Nakano S,Yamaoka K,et al. Outbreaks of hand, foot, and mouth disease by enterovirus 71. High incidence of complication disorders of central nervous system. Arch Dis Child, 1980,55(8):583-588
[12]Ho M, Chen ER, Hsu KH, et al.An epidemic of enterovirus 71 infection in Taiwan. Taiwan Enterovirus Epidemic Working Group.N Engl J Med,1999,341(13):929-935
[13]Zhu B(朱冰),Zhong JY,Xia HM,et al. Etiology of hand, foot and mouth disease in Guangzhou in 2008. Chin J Pediatr (中华儿科杂志),2010,48(2):127-130
[14]Huang ML,Chiang PS,Lou ST,et al. Development of a high-throughput assay for measuring serum neutralizing antibody against Enterovirus 71. J Virol Methods,2010,165(1):42-45
[15]Ooi EE,Phoon MC,Ishak B,et al. Seroepidemiology of human Enterovirus 71,Singapore. Emerg Infect Dis,2002,8(9):995-997
[16]Lou ST,Chiang PS,Chao AS, et al. Enterovirus 71 maternal antibodies in infants,Taiwan. Emerg Infect Dis,2009,15(4):581-584
[17]Pozzetto B,Gaudin OG,Aouni M,et al. Comparative evaluation of immunoglobulin M neutralizing antibody response in acute-phase sera and virus isolation for the routine diagnosis of enteroviuus infection. J Clin Microbiol,1989,27(4):705-708
[18]Gao YY(高媛媛), Yang SD, Tao JP, et al. Clinical features and critical illness risk factors of children with hand, foot and mouth disease of neurological involvement. Chin J Evid Based Pediatr(中国循证儿科杂志),2010,5(2):135-139
[19]Lin HS(林海生), Yang SD, Ning SR, et al. Clinical analysis of 19 children with brainstem encephalitis associated with hand, foot and mouth disease. Chin J Evid Based Pediatr(中国循证儿科杂志),2009,4(8):520-524
[20]Ooi MH, Solomon T, Podin Y, et al.Evaluation of different clinical sample types in diagnosis of human enterovirus 71-associated hand-foot-and-mouth disease.J Clin Microbiol, 2007,45(6):1858-1866
[21]Yang Y, Wang H, Gong E, et al. Neuropathology in 2 cases of fatal enterovirus type 71 infection from a recent epidemic in the People's Republic of China: a histopathologic, immunohistochemical, and reverse transcription polymerase chain reaction study.Hum Pathol, 2009, 40(9):1288-1295
[22]Wong KT,Munisamy B,Ong KC,et al. The distribution of suggests possible viral spread by neural pathways. J Neuropathol Exp Neurol,2008,67(2):162-169
[23]Chang LY, Lin TY, Hsu KH, et al. Clinical features and risk factors of pulmonary edema after enterovirus 71 related hand, foot, and mouth disease. Clin Infect Dis,1999,29(1):184-190
[24]Wang SM, Lei HY, Huang KJ, et al. Pathogenesis of enterovirus 71 brainstem encephalitis in pediatric patients: roles of cytokines and cellular immune activation in patients with pulmonary edema. J Infcet Dis, 2003,188(4):564-570
[25]Lin TY, Hsia SH, Huang YC, et al. Proinflammatory cytokine reactions in enterovirus 71 infections of the central nervous system. Clin Infect Dis, 2003,34(3):269-274
[26]Nagata N, Iwasaki T, Ami Y, et al. Differential localization of neurons susceptible to enterovirus 71 and poliovirus type I in the central nervous system of cynomolgus monkeys after intravenous inoculation. J Gen Viral, 2004,85(10):2981-2989
[27] Abu Bakar S, Shafee N, Chee HY. Adenovirus in EV71-associated hand, foot, and month disease. Lancet, 2000,355(9198):146
[28]Chen YC, Yu CK, Wang YF, et al. A murine oral enterovirus 71 infection model with central nervous system involvement. J Gen Virol,2004,85(1):69-77
[29]Ren R, Racaniello VR. Poliovirus spreads from muscle to central nervous system by neural pathway. J Infect Dis, 1992,166(4):747-752
[30]Ong KC, Badmanathan M, Devi S, et al.Pathologic characterization of a murine model of human enterovirus 71 encephalomyelitis. J Neuropathol Exp Neurol,2008,67(6):532-542
[31]Shieh WJ, Jung SM, Hsueh C, et al. Pathological studies of fatal cases in outbreak of hand, foot, and mouth disease, Taiwan. Emerg Infect Dis, 2001,7(1):146-148
[32]Wong KT. Emerging and re-emerging epidemic encephalitis: A tale of two viruses. Neuropathol Appl Neurobiol, 2000, 26(4):313-318
[33]Wong KT, Lum LC, Lam SK. Enterovirus 71 infection and neurologic complications. N Engl J Med, 2000,342(5):356-357
[34]Yang Y, Wang H, Gong E, et al Neuropathology in 2 cases of fatal enterovirus type 71 infection from a recent epidemic in the People′s Republic of China: a histopathologic, immunohistochemical, and reverse transcription polymerase chain reaction study. Hum Pathol, 2009,40(9):1288-1295
[35]Lee TC, Guo HR, Su HJ, et al. Diseases caused by enterovirus 71 infection. Pediatr Infect Dis J,2009,28(10):904-910
[36]Chang LY, Lin TY, Hsu KH, et al. Clinical features and risk factors of pulmonary oedema after enterovirus-71-related hand,foot and mouth disease. Lancet, 1999, 354(9191):1682-1686
[37]Sedy J , Zicha J , Nedvídková J , et al. The role of sympathetic nervous system in the development of neurogenicpulmonaryedema in spinal cord-injured rats. J Appl Physiol,2012,112 (1): 1-8
[38]Huang CC, Liu CC, Chang YC, et al. Neurologic complications in children with enterovirus 71 infection.N Engl J Med, 1999, 341(13):936-942
[39]Chen YC, Yu CK, Wang YF, et al. A murine oral enterovirus 71 infection model with central nervous system involvement. J Gen Virol, 2004,85(Pt 1):69-77
The introspection on clinical staging and pathological features of autopsy and clinical manifestations after Enterovirus 71 infection
WEIDan1,5,JIANGMin1,5,OUWei-lin2,5,LIPei-qing3,5,LIKun-xiong1,LIYun-qian2,CHENE4,XIONGYu-mei34,NONGGuang-min1,YANGSi-da3
(1FirstAffiliatedHospitalofGuangxiMedicalUniversity,Nanning530021; 2AffiliatedHospitalofGuilinMedicalCollege,Guilin541001; 3GuangzhouWomenandChildren′sMedicalCenter,Guangzhou510623 ; 4YuLinSecondPeople′sHospital,GuangxiZhuangAutonomousRegion,YuLin537000,China;5hasequalcontribution)
NONG Guang-min,E-mail:ngm8525@163.com;YANG Si-da,E-mail:sida_yang@yahoo.com.cn
ObjectiveTo observe clinical progression in severe cases with enterovirus 71 (EV71) infection, attempt to explore the neurologic invasive pathways, and introspect on the " Clinical expert consensus of EV71 infection severe cases (referred to expert consensus) " after EV71 infection.MethodsUnsurvival cases of EV71 infection were selected from nine hospitals in Guangxi (12 cases) from 2008 to 2010,and in Guangzhou Women and Children′s Medical Center (2 cases) from2011 to 2012, to analyze these 14 cases in clinical manifestations and features of autopsy.Results14 unsurvival cases of EV71 infection, male: female =7∶7 , aged from 7 to 36 months, the average age was (19.0 ± 9.8) months. The autopsy common features of 14/14 cases were the brainstem cribriform necrosis and malacia formation, 10 cases involved in the medulla oblongata, and there were no inflammatory cells in other organs. Nine symptoms/signs (34.6%) in the expert consensus hadn′t been recorded. Both seizure and disturbance of consciousness in stage 4 had occurred with the symptoms / signs in stage 2 simultaneously. The symptoms/signs could be observed at the beginning were fever, rash, vomiting, startle, seizure, fatigue; 42.9% cases appeared various neurological symptoms orderly, simultaneously or alternately until death. The 12/14 cases average survival duration after onset of symptoms/ signs was 72.4 h, and after appearing any abnormal basic vital signs in stage 3(mean duration 65.5 h) was 6.9 h, and after appearing neurologic symptoms/ signs in stage 2 (mean duration 39.8 h) was 32.6 h.Conclusion①The cause of death for confirmed EV71 infection was brainstem function failure; ②It is speculated that EV71 neurologic invasive pathways existed; ③It is recommended that neurologic specialist assessment for special clinical indicators is needed after EV71 infection; ④Seizure and confusion should be included in the earlier observation indicators; ⑤It is proposed that indicators of neurologic specialist assessment would be used in the fuller clinical staging study of EV71 infected neurologic involvement, to provide sufficient time of observation and intervention for clinicans.
Enterovirus 71; Nerve damage; Course; Autopsy; Clinical staging
1 广西医科大学第一附属医院 南宁,530021; 2 桂林医学院附属医院 桂林,541001;3 广州市妇女儿童医疗中心广州,510623;4 广西壮族自治区玉林市第二人民医院 玉林,537000; 5 共同第一作者
农光民,E-mail:ngm8525@163.com;杨思达,E-mail:sida_yang@yahoo.com.cn
10.3969/j.issn.1673-5501.2013.02.001
2012-11-17
2013-03-11)
张崇凡)
