A ONE-STAGE MODEL OF EXPERIMENTAL ACUTE NECROTIZING PANCREATITIS IN RATS*
2013-12-01SARAPULTSEVAlexeyRANTSEVMaximSARAPULTSEVPetrMEDVEDEVASvetlanaDANILOVAIrina
SARAPULTSEV Alexey,RANTSEV Maxim,SARAPULTSEV Petr,MEDVEDEVA Svetlana,DANILOVA Irina
(Institute Immunology and Physiology,the Ural Branch of Russian Academy of Sciences,Yekaterinburg 620219,Russia.E-mail:a.sarapultsev@gmail.com)
[ABSTRACT] AIM:To establish a one-stage model of experimental acute necrotizing pancreatitis(ANP)in rats characterized by the simplicity of performance and a high degree of repeatability.METHODS:ANPmodeling in rats was performed based on modification of the ligation model as follows:synthetic material ligature using an atraumatic needle was performed to capture pancreatic gland ducts and marginal duodenum vessels.Ligature tips were exteriorized to the abdominal wall,and the ligature was skinned over to avoid catching intestine loops.Pancreatic macroscopic appearance and histological changes were observed.Blood biochemical and hemostatic indicators were also determined.RESULTS:Laboratory analysis of rats with experimental ANP showed a pattern of disturbances similar to that observed during pancreatic necrosis in humans as soon as the first day.General blood analysis revealed enhanced leukocytosis and alterations in leukogram characteristics,indicating acute inflammation.Serum levels of amylase,aspartate aminotransferase and creatinine significantly increased(P<0.05).Hemostatic indicators showed alterations indicating formation of disseminated intravascular coagulation,and signs of endotoxicosis were observed.These typical pancreatic necrosis patterns of disturbances were validated by the results of histological investigation.CONCLUSION:Histological changes and laboratory indicators confirm the development of a suitable model of ANP.
[KEY WORDS] Pancreatitis,acute necrotizing;Rats;Endotoxemia
Acute pancreatitis(AP)currently ranks first among acute abdominal diseases,and severe forms of the disease occur in 19%of the cases[1-4].The total lethality rate varies from 4%to 15%[2,5].Despite the availability of multiple conservative and surgical treatments,lethality from destructive forms of AP ranges from 25% to 60%[6-9].Improving classic treatment methods and developing new approaches to treat common pancreatic necrosis requires experimentation using an increased number of laboratory animals[10].
The first reference to an experimental model of AP was in 1856 by Bernard,who induced pancreatitis by introducing olive oil into the excretory duct of a pancreatic gland[11-12].Obstructive pancreatic necrosis simulation experiments were subsequently performed(Pavlov I,1877).Later models included intraperitoneal introduction of ethionine(Farber E,Proper H,1950)or infected contents of the duodenum and bile directly into pancreatic tissue(Nikolaev IG,1962)[11,13-14].Although a variety of new AP simulators are currently available,most methods are technically complex and lack reproducibility[10,13,15].
The majority of AP models are based on the canalicular hypertension mechanism of disease introduction[16-17].Although canalicular hypertension models are pathogenetically justified,obtaining intraductal hypertension and disorder in pancreatic juice outflow often contradicts the anatomical-functional conditions of AP genesis.High variability in intraductal aggression components by different researchers,absence of a differentiated approach regarding the required concentration of damaging compounds,and the level of intraductal pressure at the moment of stimulus introduction all lead to significant differences in experimental AP intensity and severity of morphological-functional pancreatic and systematic metabolic disorders.As a result,data interpretation is difficult,diminishes reliability,and prevents unification of AP simulation methods in experimental practice.
Traumatic AP simulators modeled by introduction of different chemical substances directly into pancreatic tissue with or without ligation of the chief excretory duct of the pancreas have gained interest.Bile,proteolytic enzymes,turpentine,different acids,salts,oils,Triton X-100 and others are used most frequently[16].However,traumatic APsimulators cause limited acute tissue necrosis focused on the location where the damaging agent was introduced.When using these simulators,important pathological processes preceding the destructive changes are not taken into account and the degree of the organ’s involvement is not commensurate with the actual clinical process due to its distinct local nature.
Infectious methods of AP simulation are based on the introduction of pathogenic bacterial suspensions,staphylococcal toxin and lecithovitellase mixture in the pancreas duct or tissue or by infection of the gallbladder and duodenum cavity with conditionally pathogenic microorganisms[16,18].These simulators result in acute purulent pancreatitis,which represents a secondary process under natural conditions and is a consequence of an aseptic inflammatory destructive process in the organ that is not taken into consideration when using infectious simulators.
Methods of APsimulation based on the introduction of supramaximal doses of exogenous pepsinogen secretagogues(i.e.,synthetic cholecystokinins and structural analogs caerulein)and secretin have gained attention[19-21].However,these methods reflect only the degree of intensity of pancreas-stimulating effects,which are manifest with or due to a number of well-known structural/functional disorders.In addition,application of stimulators in practice is not economical due to the high cost of exogenous pepsinogen secretagogues.
Vascular AP models are based on embolization,ligation and occlusion of intrapancreatic and extrapancreatic vessels[16,22].The comparative complexity of their implementation is the main drawback of these models.One simple and reasonably effective model should be mentioned[23],although this technique has drawbacks in that it isn’t conducive to finding the Wirsung’s duct of pancreas hidden in the duodenum mesentery adipose aggregations.The use of a microirrigator to thread the filament leads to trauma to the duodenum mesentery and sharply increases the risk of bleeding due to vessel injury.Microirrigator exteriorization on the dorsal abdominal wall increases the risk of the injuries of retroperitoneal vessels,kidney and ureter,and can pinch the portal vein.Prolonged pancreas duct system clamping(up to 2~3 h)during replication of the experimental model does not always result in pancreatic necrosis.
Based on technical and economic considerations,most experiments are performed using small test animals,such as mice and rats.During experimentation on large-scale groups of small test animals,researchers are often compelled to use one-phase schemes of AP modeling based on vessel ligation.Rats are an optimal model because of their well-described physiology and anatomy,their digestive system structure and feeding patterns similar to human’s,their resistance to surgical insult,and showing disease results in a short period of time due to their high metabolic rate.
The objective of this research is to develop a new model of acute necrotizing pancreatitis(ANP)in rats to test novel conservative and surgical treatments for the disease.
MATERIALS AND METHODS
1 Animal preparation and anesthesia
Experiments were performed on healthy,sexually mature,nonlinear albino female rats.Animals were quarantined in the vivarium at the Institute of Immunology and Physiology of the Ural Branch of Russian Academy of Sciences(RAS;Yekaterinburg,Russia).The animals showed no symptoms of any disease.All animals were maintained under the same conditions and fed according to a customary schedule.All animals undergoing surgery received a similar level of care and attention.Surgery was performed using aseptic technique and sterile instruments.
All experimental procedures with animals were approved by the Institute of Animal Care and Use Committee at the Institute of Immunology and Physiology of the Ural Branch of RAS,and performed in accordance with the principles formulated in the European Convention for the Protection of Vertebrate Animals used for Experimental and Other Scientific Purposes(Strasbourg,France,1986-03-18),the American Physiological Society Guiding Principles in the Care and Use of Vertebrate Animals in Research and Training,and the Laboratory Practice Regulations of Russian Federation(Ministry of Public Health Order No.267 from 2003-06-19)[24-26].
For separate experiments,the procedure was as follows:after fasting overnight,the rats were anesthetized with ether,and experimental acute pancreatic necrosis was performed;at the endpoints,all rats were anesthetized with ether and decapitated;diazepam(2.5 mg/kg)was used to reduce the dose of general anesthetic and for smoother induction and recovery[25-26].Thirty rats with body weight of 180~240 g were randomly divided into two groups(n=15 in each group):experiment group and control group.The average body weight of the rats in experiment group was 223 g,while that in control group was 220 g.Animals underwent midline laparotomy with subsequent wound closure.Body weight dispersion of the initial mass did not exceed 10%.The animals were removed from the experiment 24,120 and 168 h after previously narcotized by intraperitoneal introduction of 40 mg/kg pentobarbital sodium.
2 Experimental protocol
2.1 Concise description of the technique Under anesthetic,midline laparotomy in the length of 2~3 cm was performed along the Sergeant’s white(Hunter’s)line to reduce blood loss.The duodenum,mesogaster and part of the stomach were delivered,and transillumination of duodenum mesentery elements was performed to visualize details,including the affected elements(pancreatic gland ducts and duodenum marginal vessel).Synthetic material(section diameter=0)ligature using an atraumatic needle was performed to capture the gland duct and marginal duodenum vessel.Ligature tips were exteriorized to the abdominal wall,and the ligature was skinned over to avoid catching intestine loops.The laparotomy wound was sutured.The ligation exposure time was 50~60 min,at which time ligature was completely removed from the abdominal space.
Ten minutes after experimental ANPmodeling,the animals resumed preoperative behavioral reactions.After evaluating behavioral patterns over 24 h,there were no detectable peculiarities in behavioral responses and animals were active and responded readily to light and acoustic stimulation.There were no symptoms of respiratory failure,malnutrition or altered liquid consumption.The animals only received water during the first 24 h,but their eating switched to habitual patterns after 48 h.
2.2 Methods for validating modeling The pancreas was morphologically evaluated after fixation.Lightoptical examination was performed in addition to visual assessment.Paraffin blocks were made according to common histological methods.Series of 5~6μm thick sections were stained with hematoxylin and eosin(HE)after van Gieson and Weigert staining[27-28].
Hemostatic parameters including thrombelastography data(R,К and MA),antithrombin III,fibrinogen,prothrombin consumption index and D-dimers were measured to evaluate the intensity of hemocoagulation dysfunction according to standard instructions[29].
Thrombelastography was executed on a 4-channel thrombelastograph ROTEM® (Tem International,Munich,Germany)according to the manufacturer’s instructions.
Antithrombin III,fibrinogen and D-dimers were analyzed on a fully automated Sysmex® CA-7000 System(Siemens,Erlangen,Germany)with Dade Behring reagents(Dade Behring,Marburg,Germany).The coagulation technique was used to determine the fibrinogen concentration[30].A chromogenic method was applied to assess antithrombin III activity.
Prothrombin consumption index was determined using STart® 4 Hemostasis Analyzer(Diagnostica Stago,France)and Techplastin kit(Biokont,Russia)according to the manufacturer’s instructions.
The coupling capacity of albumin in serum was defined by the fluorescence method using a Hitachi MPF-4(Japan)spectrofluorometer with Zond-Albumin kit(Zond,Moscow,Russia)according to the manufacturer’s instructions.
Concentrations of low-and average-molecular weight substances in plasma and erythrocytes were analyzed using Malakhova’s method at 254 and 280 nm wavelengths[31].
Blood(3 mL)for biochemical examination was drawn by cardiac puncture with subsequent centrifugation and serum separation,and analyzed using IMMAGE® 800 Immunochemistry System(Beckman Coulter,Switzerland).
3 Statistical analysis
Student’s t test was applied to compare the differences between groups using the SPSS computer program.Data were expressed as mean±SEM.P<0.05 was considered statistically significant.
RESULTS
Macroscopically,one day after impact on the pancreas and duodenum marginal vessel,animals in experiment group displayed necrotic foci accompanied by hemorrhagic impregnation and symptomatic perifocal edema.On the 5th day,multiple steatonecrosis,serous-hemorrhagic bloody effusion,peritonitis symptoms and mode-rately increased enteroparesis were detected on the parietal and visceral peritoneum of the abdominal cavity.On the 7th day,animals in experiment group showed deve-loping purulent common peritonitis or intra-abdominal abscesses.All phases of the clinical course of necrosis were observed.
During the 1st day of the experiment,the necrotic focus was represented by destruction of acinar structures in the exocrine region of the pancreas.Cells with karyorrhexis,karyolysis,plasmatorrhexis and plasmolysis were observed.The trabecular vessels were full of blood.Sludge complexes were formed in the clearance and parts of the vessels with marginal leukocyte diapedesis.A pronounced extravasate reaction in the form of polymorphonuclear leukocyte infiltration into trabecular structures was also observed.In a number of cases,the necrosis of acini and endocrine structures was detected in lobuli of the pancreas(Figure 1A).
The necrotic zone with destroyed structures of some lobes of the organ parenchyma was observed on the 5th day(Figure 1B).Vascular wall destruction was identified in connective tissue trabecules,while diffuse leukocyte infiltration with abscess formation was observed in the adjacent mesentery and peritoneum.
On the 7th day,the affected zone was replaced by granulation tissue consisting of fibroblasts,fibrous structures and multiple capillaries of the sinusoidal type.Granulation tissues were infiltrated with lymphocytes and a small quantity of polymorphonuclear leukocytes,and mast cell migration was observed.An apparent macrophage response was also observed(Figure 1C).
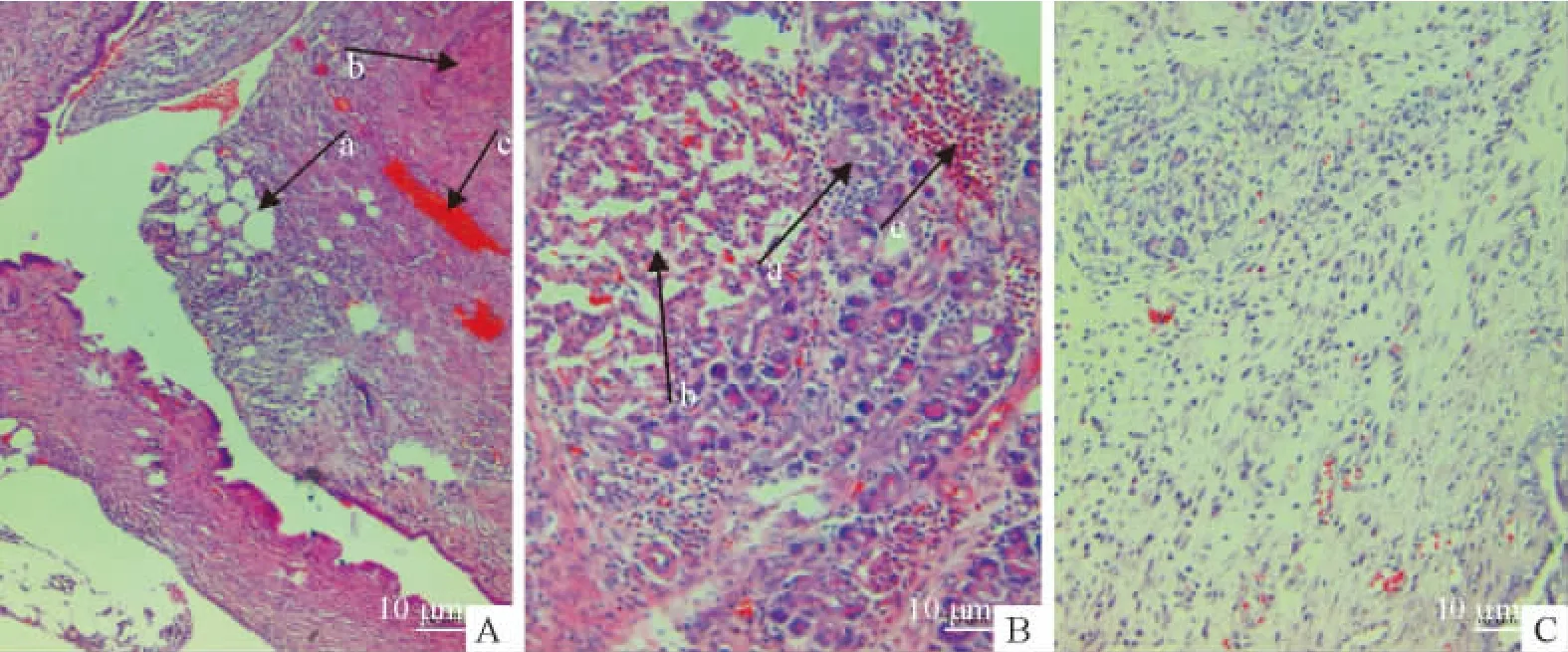
Figure 1.Pancreatic necrosis observed under microscope(HE staining;A,C:×200;B:×400).A:on the 1st day,destruction of acinar structures in exocrine regions of the pancreas(a),full trabecular vessels(b)and focal hemorrhage(c)were observed;B:on the 5th day,destroyed acinar structures in exocrine regions of the pancreas(a),dystrophic changes in pancreatic islets(b)and perifocal infiltration with polymorphonuclear leucocytes(c)were observed;C:on the 7th day,the affected zone was replaced by granulation tissue elements infiltrated with lymphocytes and polymorphonuclear leucocytes.
Structural alterations in the pancreas on the 1st day of the experiment were accompanied by the changes of blood biochemical and hemostatic parameters,as shown in Tables 1 and 2.
Serum levels of amylase,aspartate aminotransferase(AST)and creatinine were significantly increased in experiment group compared with control group(Table 1).
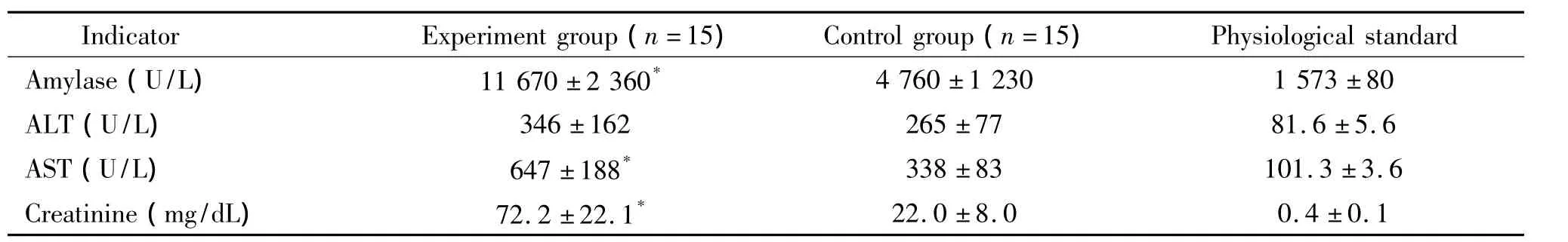
Table 1.Changes of serum biochemical indicators(Mean±SEM)
On the 1st day,hemostatic indicators including antithrombin III activity,fibrinogen concentration,platelet count and prothrombin consumption index in experiment group were all at high levels compared with control group(Table 2).
According to the thrombelastography data,the rats in experiment group demonstrated reduced blood coagulation activity at 1 and 2 phases of blood coagulation and formation of the grume fibrin/thrombocyte structure indicated by R,КandМА(R characterizes the first two phases of blood coagulation;КandМАcharacterize the quality of the grume fibrin/thrombocyte structure),as compared with the control rats(Table 2).
D-dimer concentration,an indicator that reflects an imbalance between thrombus formation and fibrinolysis system,in experiment group was significantly higher than that in control group.A reduction in albumin coupling capacity was observed in experiment group on the 1st day compared with control group(Table 2).The concentration of low-and average-molecular weight substances in red cells in experiment group was reliably lower than that in control group.Reduced catabolic pool levels were observed in experimental ANP rats that had been introduced to the L-17 compound compared with the control rats(0.040/0.053 for plasma and 0.335/0.392 for red cells).
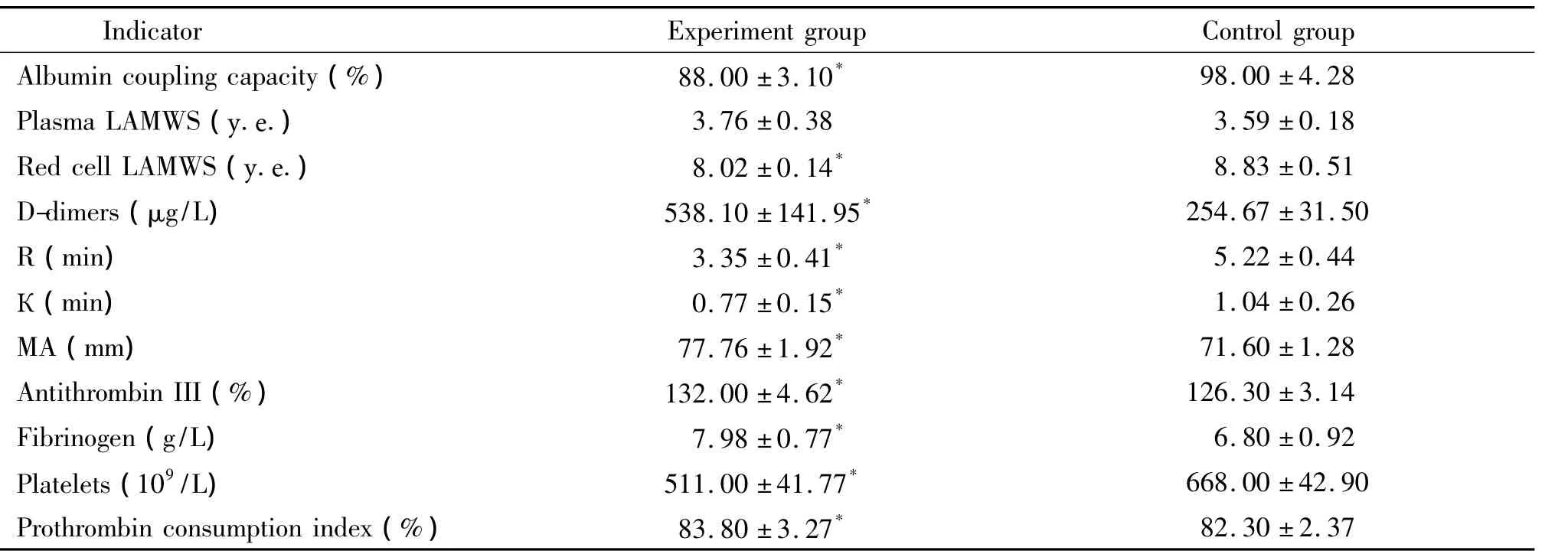
Table 2.Primary endotoxicosis and hemostasis indicators on the 1st day of the experiment(Mean±SEM.n=15)
DISCUSSION
None of the rodent APmodels are perfect and each has its own strengths and weaknesses.Useful animal AP models are pragmatic in that most of them are:(1)elicited in rodents(rats and mice),which are cheap,easy to handle and readily available to genetic manipulation;(2)characterized by moderate to severe degrees of pancreatic injury[33].This study was performed to develop a one-stage model of experimental ANP in rats characterized by simple performance and a high degree of repeatability.
In general,noninvasive models are relatively simple and inexpensive to create,and have become quite popular.However,none of these models are relevant to human disease with respect to etiology(such as triggering event)[33].In addition to the attractive feature of possibly mimicking the event that triggers human biliary pancreatitis,invasive AP models require anesthesia of the animal,which can be challenging.Postoperative problems,such as infection and difficulties in maintaining nutrition,can cause difficulties in interpreting the results[33].
The currently available AP/ANP experimental model(Lugovoy AO,2007)is not free from drawbacks in that it is difficult to find the Wirsung’s duct hidden in duodenum mesentery adipose aggregations[23].The use of a microirrigator for suture conduction increases duodenum mesentery injury and dramatically increases the bleeding risk due to vessel damage.The exteriorization of the microirrigator to the abdominal cavity dorsal wall can increase the injury risk for retroperitoneal vessels in the kidney and ureter and can cause portal vein cross-clamping.Moreover,in case of experimental model reproduction,even an increase(up to 2~3 h)in the gland duct system cross-clamping time does not always lead to development of pancreatic necrosis.
The model presented in this study is virtually free of the previously stated drawbacks,and duration of the artery cross-clamping leads to 98%~99%efficiency in development of experimental pancreatic necrosis without preoperative lethality and lethality within the 1st day.The main disadvantages of the present model are the need for anesthesia and a sufficiently long time-consuming surgery.
Laboratory analysis of the experimental ANPcourse showed that the patterns of disturbances are similar to those observed during the course of pancreatic necrosis in humans as soon as the first day.General blood analysis revealed increased leukocytosis and alterations in the leukogram characteristics of acute inflammation.Blood amylase,AST and creatinine significantly increased.Hemostatic indicators showed alterations indicating formation of disseminated intravascular coagulation(increases in D-dimers,fibrinogen and antithrombin III).Signs of endotoxicosis(albumin coupling capacity reduction to 88%and concentration changes of low-and average-molecular weight substances in plasma and erythrocytes)were also observed.
This typical pattern of pancreatic necrosis disturbances was validated by the results of histological investigation.On the 1st day of experimental ANP,a distinctive phase of exudative inflammation without leukocytic bank formation around the disturbed zone was observed in the necrotic focus of pancreatic exocrine region.On the 5th day,the necrosis zone increased and occupied several pancreatic lobes.Intensive infiltration of necrotic parenchymatous structures and stromal elements accompanied by destruction of trabecular collagen fibers was observed.In some cases,this was accompanied by abscess formation.On the 7th day,exudative inflammation had spread to adjacent mesentery and omentum structures and signs of organization via granulation tissue formation represented by functionally active fibroblasts,sinusoidal capillaries,and elastic fibers were observed in the affected zone.
Conclusively,the histological changes and laboratory indicators of the experimental rats indicate development of a suitable ANP model.Specific features of this method are applicable for experiments with large groups of small laboratory animals to enable the study of disease pathogenesis and testing novel treatment methods.
ACKNOWLEDGMENTS
The authors would like to thank the Ural Branch of RASfor providing financial means and laboratory facilities.
This manuscript has been edited by experts of BioMed Proofreading.
