Fine needle aspirating and cutting is superior to Tru-cut core needle in liver biopsy
2013-06-01
Shanghai, China
Fine needle aspirating and cutting is superior to Tru-cut core needle in liver biopsy
Guo-Ping Li, Gao-Quan Gong, Xiao-Lin Wang, Yi Chen, Jie-Min Cheng and Chang-Yu Li
Shanghai, China
BACKGROUND:Liver biopsy is the "gold standard" for evaluating liver disorders, but controversies over the potential risk of complications and patient discomfort still exist. Using a 21G fi ne needle, we developed a new biopsy procedure, fi ne needle aspirating and cutting (FNAC). Our procedure obtains enough tissue for pathological examination and meanwhile, reduces the risk of biopsy complications. The present study was to determine the safety and eff i ciency of 21G FNAC compared with 18G Tru-cut core needle (TCN) in liver tumor biopsies.
METHODS:Ninety-four patients with unresectable malignant tumors were included in this study. Patients were divided into 2 groups: 18G TCN and 21G FNAC. The total positive rate (TPR) and safety of both groups were compared.
RESULTS:TPR was not different between the two groups. Liver puncture track subcapsular hemorrhage and arteriovenous shunt were reported with 18G TCN but not with 21G FNAC. The incidence of pain caused by biopsy was higher for the 18G TCN group compared to the 21G FNAC group (P<0.05). About 82.6% of the patients in the 18G TCN group had a sample length >0.5 cm, but 52.1% in the 21G FNAC group (P<0.05). More than 50% of patients in both groups had suff i cient tissue for immunohistochemical examination.
CONCLUSIONS:TPR is not different between the 21G FNAC and 18G TCN biopsy procedures, but the safety of 21G FNAC is superior to that of 18G TCN. Tissues obtained by either of these two procedures are suff i cient for a pathological diagnosis.
(Hepatobiliary Pancreat Dis Int 2013;12:508-511)
biopsy;tumor; chemoembolization; diagnostic; liver
Introduction
Percutaneous liver biopsy is one of the most important and widely used methods for the diagnosis of liver diseases and considered as the most specif i c method to assess the nature, the grade and the stage of certain liver diseases[1,2]and therefore, it is regarded as the "gold standard". Liver biopsy is more reliable than noninvasive modalities. Bialecki et al[3]recommended a greater role for image-guided biopsy of lesions greater than 1 cm that are clinically suspicious for HCC, in order to allow for adequate treatment planning, because the risks of biopsy appear small and the potential benef i ts are signif i cant. However, controversies related to the potential risk of complications and patient discomfort still exist.[4-6]
To pathologists, a suff i cient biopsy tissue sample length is one of the most important factors in obtaining a reliable pathological diagnosis. Guido and Rugge[7]integrated previous and more recent data, and found that a biopsy sample length of 2 cm that contains at least 11 complete portal tracts should be suff i cient for reliable grading and staging of chronic viral hepatitis. Kugelmas[8]suggested that a reliable sample should be at least 2.5 cm in length, but approximately 3 entries into the tumor tissue are required to obtain this length, which increases the risk of bleeding. More punctures mean a higher rate of bleeding after the procedure. Szymczak and colleagues[4]retrospectively analyzed 1412 percutaneous liver biopsies, and 259 (18.3%) of them had complications, of which pain was the most common one (15.3%). Nine serious biopsy-related complications showed hemorrhage, hemothorax and biliary peritonitis. But there was no liver biopsy-associated fatality. Huang et al[9]reported that the bleeding rate after biopsy was about 0.32%; Own et al[10]reported that the main percutaneous liver biopsy complications were bleeding, bile leakage, hemothorax, and abdominal organ perforation, and that the overall incidence and mortality rates were approximately 3.2% and 0.01% to 0.1%, respectively.
The development of immunohistochemistry allowedfor a more accurate diagnosis with less tissue. It is not known whether enough tissue can be obtained from tumors using a 21G fi ne needle. We developed a new biopsy procedure using a 21G fi ne needle, which we called fi ne needle aspirating and cutting (FNAC), to obtain enough tissues and meanwhile, to reduce complications. This study aimed to determine the safety and eff i ciency of 21G FNAC and to compare FNAC with 18G Tru-cut core needle (TCN) in tumor biopsies.
Methods
The study population comprised 94 patients (69 males and 25 females, aged 18 to 74 years) diagnosed with malignant tumors using CT/MRI or other tumor biomarkers. All of the tumors were unresectable and transarterial chemoembolization (TACE) was planned for palliative treatment. All patients were hospitalized in the Department of Interventional Radiology, Zhongshan Hospital, Fudan University from January 2009 to December 2011. To prepare for the procedure, a coagulation parameter assessment, blood morphology tests, liver and kidney function tests, and a chest X-ray were performed. The liver function grade (Child-Pugh classif i cation) was also assessed, and patients who had a Child-Pugh grade of "C" were excluded. This study was approved by the Ethics Committee of Zhongshan Hospital, Fudan University. All patients gave informed consent before the liver biopsy.
Patients were divided into 2 groups: 18G TCN (Trucut core needle, COOK, USA,n=46) and 21G FNAC (f i ne needle aspirating and cutting, HAKKO, Japan,n=48). A 2% lidocaine solution was administered for local anesthesia. In some cases, intramuscular diazepam was administered as premedication. An arterial angiography was performed before every liver biopsy, and the catheter was placed in a liver tumor artery. All biopsies were punctured transhepatically and guided by B-ultrasound (BUS). Every biopsy in the 18G TCN group was completed with an 18G TCN. All biopsies were performed by skillful senior physicians with more than 4 years of experience in manipulating and diagnosing of BUS. In the FNAC group, a 21G fi ne needle was used to puncture into the targeted mass, and then the inner stylet was pulled out. The core needle was pushed and pulled 3-5 times in the targeted mass so that the tumor tissues were cut off and fi lled the needle core. At the same time, a negative pressure was maintained by a syringe concatenated with the needle. All tissues and puncture fl uids underwent pathological and cytological examination. After biopsy, another arterial angiography was carried out to roll out bleeding in needle tracks. TACE was performed according to the patient's situation. The needle was sterilized using an absolute alcohol gauze before every repeated puncture into the same patient's lesion. After the procedure, the patient's vital signs were closely monitored and symptomatic and supportive treatments were given. A visual analogue scale (VAS) was applied in assessing post-biopsy pain. Analgesia was administrated to patients according to the intensity of pain. After recovered, the patients were discharged and followed as outpatients.
Data collected from archived medical documentation included age, sex, tumor biomarkers, laboratory test results, complications and outcomes, success of procedures, results of histological or cytological tissue sample evaluation, and records of biopsy processes. Assessing the procedure success and obtaining a representative sample was based on the pathologist's experience.
Statistical analysis
Statistical analysis was made using the SPSS 13.0 package (SPSS Inc., Chicago, IL, USA). The biopsy total positive rate (TPR) was obtained by counting the number of positive histological and cytological examinations. The TPR and the safety of both groups were statistically analyzed and compared. All samples were evaluated by a single pathologist. The Chi-square test and Student'sttest were used for statistical analysis. APvalue of <0.05 was considered statistically signif i cant.
Results
No signif i cant difference was noted in gender, mean age and tumor diameter between the 18G TCN and 21G FNAC groups (P>0.05, Table 1). All biopsy procedures were completed successfully. All tumors were diagnosed as malignant. The 18G TCN TPR was 89.1% and the 21G FNAC TPR was 81.3%; there was no statistically signif i cant difference in the TPRs between the two groups (P>0.05, Table 2).

Table 1.Demographics of patients
About 82.6% (38/46) of sample's length was greater than 0.5 cm in the 18G TCN group, while 52.1% (25/48) in the 21G FNAC group. Forty (87.0%) of the samples in the 18G TCN group and 36 (75.0%) in the 21G FNAC group are enough for immunohistochemistry. Hepatocellular carcinoma was the main pathologic type in more than 50% of these patients. Broken cellular structure was the main reason for negative results in the 21G FNAC group, and other negative results included inf l ammatory lesions, necrotic tissue, sludged blood, and liver tissue (Table 2).
The incidence rate of liver puncture track subcapsular hemorrhage (according to arterial angiography) and an arteriovenous shunt (A-V shunt) incidence rate was 6.5% (3/46) and 8.7% (4/46) in the 18G TCN group, while there were no detectable hemorrhage and A-V shunt in the 21G FNAC group. The incidence of pain (VAS≥1) caused by biopsy was 78.3% (36/46) in the 18G TCN group and 22.9% (11/48) in the 21G FNAC group. The average VAS score in the 21G FNAC group was signif i cantly lower than that in the 18G TCN group (0.3 ± 0.6 vs 1.2±0.7). All patients felt slight pain (VAS<3) atpuncture points and recovered 2 to 3 days later without analgesia or intervention. No patient in either group suffered from pneumothorax, pleural effusion, and peritonitis, or had severe complications such as massive bleeding or exsanguine shock. No tumor implantation was found in puncture tracks in any patient after 3 months of follow-up (Table 3).

Table 2.Pathological diagnosis of 94 patients with liver masses (n, %)
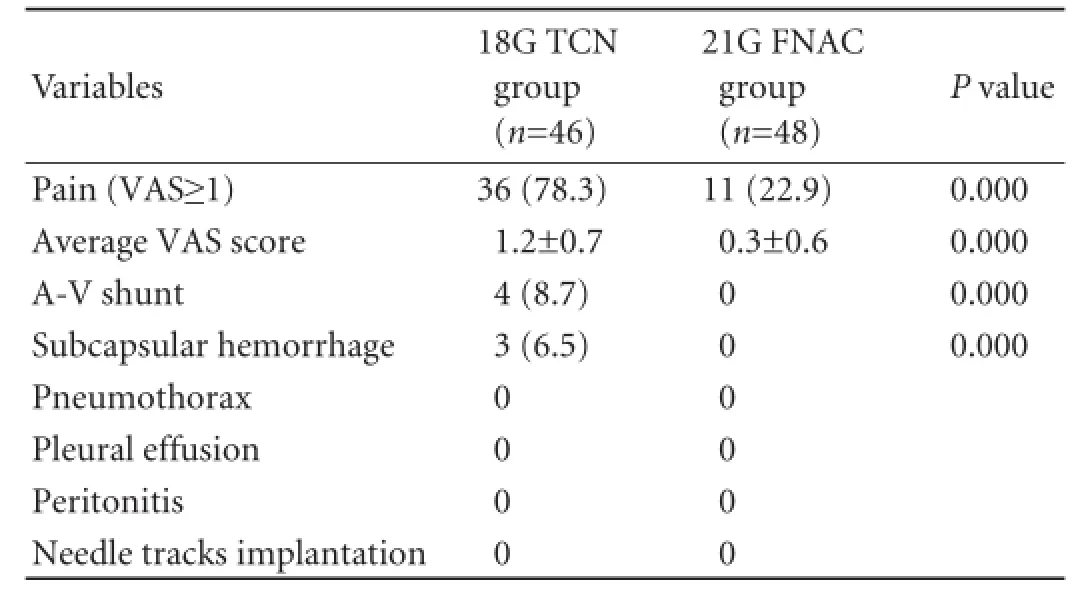
Table 3.Liver biopsy complications in the two groups (n, %)
Discussion
Many studies in the last decade evaluated the safety and risk of complications in liver biopsy.[11-13]The patients analyzed varied in indications, underlying conditions, methods, needles used, and guiding techniques. These studies demonstrated that percutaneous liver biopsy is commonly accepted as an eff i cient and safe way to diagnose liver masses. However, because biopsy is an invasive method, there are inevitable risks of complications.[14-17]These complications can be reduced by using currently available instruments and by choosing a proper process. New biopsy procedures need to be developed in order to minimize complications and to increase biopsy eff i ciency.
Currently, the 18G TCN is used most commonly in liver biopsy and it has shown a high degree of safety and eff i ciency. However, an 18G needle can cause bleeding especially in the aff l uent blood supply or perivascular masses. In patients with Chilaiditi syndrome, a liver biopsy should avoid puncturing the colon, a thin biopsy needle is preferred. When the lesions are deep-seated or close to vital structures, such as pancreatic cancer, retroperitoneal tumor or mediastinal masses, a thick needle with a diameter of more than 18G means a greater risk of bleeding and of other complications.[18-20]Fine needle aspiration (FNA) is safer for these tumors, but the tissues obtained from FNA are usually only suitable for cytological examination.[21]FNAC may partially resolve the above-mentioned drawbacks of 18G TCN and FNAC. A core fi ne needle, by "pushing and pulling", cut off the tissue and left a cavity behind. If the needle punctures throughout the tumor, there is a chance of obtaining the tissue from the whole puncture track. Additionally, if the fi ne needle is punctured into the tumor for 3-5 times at different angles, enough tissue may be obtained for histology.
TPR did not reach signif i cant difference between the two groups which implied that the eff i ciency of 21G FNAC was similar to that of 18G TCN. Furthermore, tissues obtained by 21G FNAC were comparable to those by 18G TCN in term of immunohistochemical staining, suggesting that 21G FNAC could harvest enough tissue for a pathological diagnosis as did 18G TCN. In termsof tissue length, 18G TCN is superior to 21G FNAC. However, less complication may compensate this shortness: no hemorrhage and A-V shunts in the 21G FNAC group, while 8.7% (4/46) of 18-TCN patients had A-V shunts and 6.5% (3/46) subcapsular hemorrhage. The pain complaint (VAS≥1) rate was signif i cantly lower in the 21G FNAC group than that in the 18G TCN group. The biopsy needle diameter is an important factor in causing complications, and the results of this study suggest that 21G FNAC is safer than 18G TCN.
The operator's experience and skill plays an important role in the safety and the success rate of liver biopsy.[22,23]In our study, all biopsies were performed by senior physicians who were skillful at BUS. During FNAC procedure, the actions of "pushing and pulling" were guided under ultrasonography. The cutting speed and force power could be controlled well by a skillful operator, and therefore, complications could be reduced.
We also found some drawbacks of FNAC: less tissue for histology, especially when the tumors were hard or rich in connective tissues; blood clots in the sample could also disturb the examination results.
In conclusion, tissues obtained using either of 21G FNAC or 18G TCN in liver biopsy are enough for a pathological diagnosis. There is no statistical difference in the TPR between the two biopsy procedures. However, the safety of 21G FNAC may be superior to that of 18G TCN biopsy.
Contributors:GGQ and WXL proposed the study. LGP wrote the fi rst draft. LGP and GGQ collected and analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. GGQ is the guarantor.
Funding:This study was supported by a grant from the Project of Shanghai Health Bureau (2010022).
Ethical approval:This study was approved by the Ethics Committee of Zhongshan Hospital, Fudan University (2010-105).
Competing interest:No benef i ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Bravo AA, Sheth SG, Chopra S. Liver biopsy. N Engl J Med 2001;344:495-500.
2 Campbell MS, Reddy KR. Review article: the evolving role of liver biopsy. Aliment Pharmacol Ther 2004;20:249-259.
3 Bialecki ES, Ezenekwe AM, Brunt EM, Collins BT, Ponder TB, Bieneman BK, et al. Comparison of liver biopsy and noninvasive methods for diagnosis of hepatocellular carcinoma. Clin Gastroenterol Hepatol 2006;4:361-368.
4 Szymczak A, Simon K, Inglot M, Gladysz A. Safety and effectiveness of blind percutaneous liver biopsy: analysis of 1412 procedures. Hepat Mon 2012;12:32-37.
5 West J, Card TR. Reduced mortality rates following elective percutaneous liver biopsies. Gastroenterology 2010;139:1230-1237.
6 Younossi ZM, Teran JC, Ganiats TG, Carey WD. Ultrasoundguided liver biopsy for parenchymal liver disease: an economic analysis. Dig Dis Sci 1998;43:46-50.
7 Guido M, Rugge M. Liver biopsy sampling in chronic viral hepatitis. Semin Liver Dis 2004;24:89-97.
8 Kugelmas M. Liver biopsy. Am J Gastroenterol 2004;99:1416-1417.
9 Huang JF, Hsieh MY, Dai CY, Hou NJ, Lee LP, Lin ZY, et al. The incidence and risks of liver biopsy in non-cirrhotic patients: An evaluation of 3806 biopsies. Gut 2007;56:736-737.
10 Own A, Balzer JO, Vogl TJ. Bleeding hepatic pseudoaneurysm complicating percutaneous liver biopsy with interventional treatment options. Eur Radiol 2005;15:183-185.
11 Bateson MC, Hopwood D, Duguid HL, Bouchier IA. A comparative trial of liver biopsy needles. J Clin Pathol 1980; 33:131-133.
12 Lindor KD, Bru C, Jorgensen RA, Rakela J, Bordas JM, Gross JB, et al. The role of ultrasonography and automatic-needle biopsy in outpatient percutaneous liver biopsy. Hepatology 1996;23:1079-1083.
13 de Man RA, van Buuren HR, Hop WC. A randomised study on the eff i cacy and safety of an automated Tru-Cut needle for percutaneous liver biopsy. Neth J Med 2004;62:441-445.
14 Colombo M, Del Ninno E, de Franchis R, De Fazio C, Festorazzi S, Ronchi G, et al. Ultrasound-assisted percutaneous liver biopsy: superiority of the Tru-Cut over the Menghini needle for diagnosis of cirrhosis. Gastroenterology 1988;95:487-489.
15 Pasha T, Gabriel S, Therneau T, Dickson ER, Lindor KD. Costeffectiveness of ultrasound-guided liver biopsy. Hepatology 1998;27:1220-1226.
16 Songür N, Songür Y, Bircan S, Kapucuoğlu N. Comparison of 19- and 22-gauge needles in EUS-guided fi ne needle aspiration in patients with mediastinal masses and lymph nodes. Turk J Gastroenterol 2011;22:472-478.
17 Amin Z, Theis B, Russell RC, House C, Novelli M, Lees WR. Diagnosing pancreatic cancer: the role of percutaneous biopsy and CT. Clin Radiol 2006;61:996-1002.
18 Cavanna L, Lazzaro A, Vallisa D, Civardi G, Artioli F. Role of image-guided fi ne-needle aspiration biopsy in the management of patients with splenic metastasis. World J Surg Oncol 2007;5:13.
19 Swischuk JL, Castaneda F, Patel JC, Li R, Fraser KW, Brady TM, et al. Percutaneous transthoracic needle biopsy of the lung: review of 612 lesions. J Vasc Interv Radiol 1998;9:347-352.
20 Thanos L, Zormpala A, Papaioannou G, Malagari K, Brountzos E, Kelekis D. Safety and eff i cacy of percutaneous CT-guided liver biopsy using an 18-gauge automated needle. Eur J Intern Med 2005;16:571-574.
21 Böcking A. Cytological vs histological evaluation of percutaneous biopsies. Cardiovasc Intervent Radiol 1991;14:5-12.
22 van der Poorten D, Kwok A, Lam T, Ridley L, Jones DB, Ngu MC, et al. Twenty-year audit of percutaneous liver biopsy in a major Australian teaching hospital. Intern Med J 2006;36: 692-699.
23 Froehlich F, Lamy O, Fried M, Gonvers JJ. Practice and complications of liver biopsy. Results of a nationwide survey in Switzerland. Dig Dis Sci 1993;38:1480-1484.
Received August 30, 2012
Accepted after revision January 15, 2013
AuthorAff i liations:Department of Interventional Radiology, Zhongshan Hospital, Fudan University, Shanghai 200032, China (Li GP, Gong GQ, Wang XL, Chen Y, Cheng JM and Li CY)
Gao-Quan Gong, MD, Department of Interventional Radiology, Zhongshan Hospital, Fudan University, Shanghai 200032, China (Fax: 86-21-64037258; Email: gong.gaoquan@zs-hospital.sh.cn)
© 2013, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(13)60080-6
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Simultaneous recovery of dual pathways for ammonia metabolism do not improve further detoxif i cation of ammonia in HepG2 cells
- Optimal central venous pressure during partial hepatectomy for hepatocellular carcinoma
- Risk factors and clinical characteristics of portal vein thrombosis after splenectomy in patients with liver cirrhosis
- Diagnostic accuracy of enhanced liver fi brosis test to assess liver fi brosis in patients with chronic hepatitis C
- Mattress sutures for the modif i cation of end-toend dunking pancreaticojejunostomy
- Retrohepatic vena cava deroof i ng in living donor liver transplantation for caudate hepatocellular carcinoma