Mattress sutures for the modif i cation of end-toend dunking pancreaticojejunostomy
2013-06-01
Adana, Turkey
Mattress sutures for the modif i cation of end-toend dunking pancreaticojejunostomy
Nurkan Torer, Ali Ezer and Tarık Zafer Nursal
Adana, Turkey
Despite the improvement of surgical techniques, the rate of anastomotic failure of pancreaticojejunostomy remains high (30%-50%). Here we describe the use of vertical mattress sutures in the modif i cation of dunking pancreaticojejunal anastomosis. In 7 patients who used this technique, neither anastomotic failure nor any major postsurgical complication developed. This technique is an easy, safe, and promising for the performance of pancreaticojejunostomy.
pancreaticoduodenectomy; pancreaticojejunostomy; technique
Introduction
Leakage from a pancreaticojejunostomy (PJ) anastomosis is a life-threatening complication. Despite the improvement of surgical techniques, the rate of anastomotic failure of PJ remains high (30%-50%).[1,2]There are 2 commonly accepted PJ anastomosis techniques [end-to-end anastomosis (invaginating and/or dunking PJ) and end-to-side anastomosis (duct-to-mucosa Wirsung-jejunostomy)]. Furthermore, there are multiple modif i cations of these techniques. In this report, we describe the use of mattress sutures in the modif i cation of dunking pancreaticojejunal anastomosis.
Surgical technique
In end-to-end anastomosis (dunking PJ), the transected end of the jejunum is approximated to the pancreatic end through the transverse mesocolon. The pancreatic stump is isolated 2 to 3 cm from the splenic vein. Three or 4 straight 2/0 silk sutures are used during the anastomosis, and the sutures are not tied until all have been applied. The fi rst suture is placed at the caudal (mesenteric) side of the jejunum 3 to 4 cm from the cut edge of the jejunum. A needle is passed through the outer side of the jejunum to the inner side and is then passed through the caudal side of the pancreas from the anterior to the posterior side, 2 to 3 mm from the cut edge of the pancreas. In the third step, the needle is passed from the inner side of the jejunum to the outer side posteriorly and back into the lumen 2 to 3 mm closer to the cut edge of the jejunum. The needle is then passed through the pancreatic stump from the posterior to the anterior side 3 to 4 mm apart from the cut edge. Finally, the needle is passed out of the jejunal lumen from the inner side in an anterior direction (Fig. 1). Other sutures are applied in the same manner (Fig. 2). It is important not to pass through the pancreatic duct.
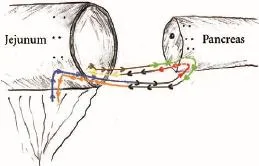
Fig. 1.Horizontal mattress sutures of internal suture line for PJ. The pathway of the first suture. A needle is passed as follows: 1) through the outer side of the jejunum to the inner side (blue line); 2) from the anterior of the pancreas to the posterior side (red line); 3) from the inner side of the jejunum to the outer posterior side (yellow line); 4) back into the lumen 2 to 3 mm closer to the cut edge of the jejunum (brown line); 5) passed through the pancreatic stump from the posterior to the anterior side 3 to 4 mm from the cut edge (green line); 6) passed out of the jejunal lumen from the inner side in an anterior direction (orange line).
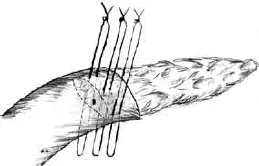
Fig. 2.Three horizontal mattress sutures passed.
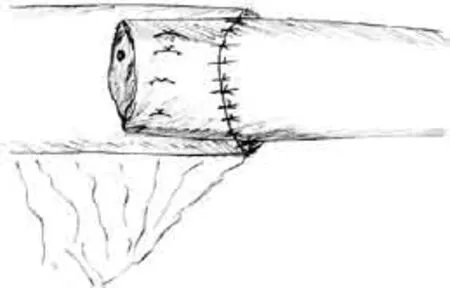
Fig. 3.Final appearance of anastomosis after all sutures are applied and tied.
Before these sutures are tied, it would be easy to insert a posterior external anastomotic suture line with 2/0 silk sutures. Posterior sutures are applied to the cut edge of the jejunum (full thickness) and to the pancreatic capsule 3 cm from the cut edge.
After this step, mattress sutures (the internal suture line) are tied fi rmly, and the pancreas is fi tted into the jejunum. Then the posterior external sutures are tied gently. Finally, we form the anterior part of the external suture line with interrupted 2/0 silk sutures (Fig. 3). The sump drains were placed to the anterior and posterior sides of the anastomosis. The Wirsung is not stented.
At our clinic, we generally prefer to perform Wirsungjejunostomy in the presence of dilated duct of at least 2-3 mm. However, when the Wirsung is narrow, dunking PJ is performed. At our institution, modif i ed PJ was performed in 7 patients (5 men and 2 women; median age 51 years, range 32-61) by a surgeon. All patients were operated upon for a mass at the head of the pancreas detected by computed tomography. Postoperatively, ductal adenocarcinoma was diagnosed in 5 patients, intraductal papillary mucinous neoplasm in 1, and autoimmune pancreatitis in 1, respectively. The pancreatic tissues were fragile, and the Wirsung ducts were narrow (1-3 mm) in all patients. Neither anastomotic failure nor any major postsurgical complications developed. We did not analyze the amylase/lipase levels in the drain fl uids. Only two patients had generated grade A postoperative pancreatic fi stula according to the International Study Group on Pancreatic Fistula guidelines. Drains of these two patients were withdrawn at postoperative days 11 and 15 respectively without any clinical complications. The median postoperative hospital stay was 8 days (range 8-14), and the median time until the resumption of feeding was 7 days (range 6-9). The median time required for the removal of the intra-abdominal drains was 8 days (range 7-15).
Discussion
PJ is the most risky anastomosis in gastrointestinal surgery. Because of the histological differences between the pancreas and jejunum, PJ anastomosis has a high rate of failure.[2]Various techniques for PJ anastomosis have been described, but this alone shows that the optimal technique has not yet been established.
The techniques of PJ anastomosis are classif i ed as end-to-end or end-to-side methods. End-to-side Wirsung-jejunostomy, which is one of the most popular techniques used to perform PJ, is recommended especially for patients with dilated Wirsung ducts and is thought by some experts to be the most effective technique in ensuring a histologically compatible PJ.[2]However, end-to-side Wirsung-jejunostomy is a diff i cult and time-consuming technique in the training setting and also is not suitable for patients with narrow Wirsung ducts.[2]
Most of the dunking PJ techniques have similar suture patterns of biting pancreas tissue tangentially. The inner layer of sutures is at high risk of being cut during that type of PJ. When the needle passes through the pancreas 2 to 3 mm proximal to the cut edge, the needle or the suture tie can tear the fragile tissue (a complication that can occur during inkwell PJ).[3]We also believe that invagination techniques can cause leakage through the inverted bulky mesentery, therefore we suggest that end-to-end PJ can be performed in a non-invaginating fashion more safely.
In the consolidation technique, the inner row sutures of PJ are bound to the vertical mattress sutures to prevent tearing of the pancreatic tissue.[4]However, a considerable amount of pancreatic tissue is squeezed between the arms of the U-suture; which may cause ischemia of the pancreas. In our technique, mattress sutures are placed parallel to the long axis of the pancreas, and the blood supply to the cut end of the pancreas is preserved. Further, our mattress sutures are not extra sutures used to consolidate the pancreas; instead, they are a part of the inner layer of PJ. We suggest that this technique is easier to perform than theconsolidation technique.
Langrehr and colleagues[5]used an anastomotic technique similar in some aspects to ours. They performed an end-to-side anastomosis, and mattress sutures were placed vertical to the long axis of the pancreas. In our opinion, end-to-end anastomosis provides a greater space through which the pancreas can be inserted into the jejunum. Furthermore, placing the mattress sutures vertical to the long axis of the pancreas could cause ischemia and might increase the risk of obliteration of the Wirsung duct. We agree with those authors that the use of mattress sutures prevents subjecting the fragile pancreas to tangential shear forces and provides additional padding with the jejunum. Also, these sutures ensure a waterproof approximation of the jejunum and the pancreatic capsule. As with this method, the pitfall of our technique is the danger of passing through the pancreatic duct. In our technique, attention must be paid to catch the Wirsung duct into the suture. We always take an effort to def i ne the duct in order to avoid iatrogenic injury. One could use intraoperative ultrasound to detect the duct or a stent to avoid pinching the pancreatic duct.
It is not appropriate to base fi rm conclusions on the description of the 7 patients described in this report. However, our study indicates that this technique is easy, safe, and promising for PJ. A surgeon who performs pancreatic surgery should be able to perform at least two different types of anastomosis and to modify them according to each patient's medical and surgical needs.
Contributors:TN proposed the study. EA and NTZ wrote the fi rst draft. TN collected and analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. TN is the guarantor.
Funding:None.
Ethical approval:Not needed.
Competing interest:No benef i ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Tewari M, Hazrah P, Kumar V, Shukla HS. Options of restorative pancreaticoenteric anastomosis following pancreaticoduodenectomy: a review. Surg Oncol 2010;19:17-26.
2 Batignani G, Fratini G, Zuckermann M, Bianchini E, Tonelli F. Comparison of Wirsung-jejunal duct-to-mucosa and dunking technique for pancreatojejunostomy after pancreatoduodenectomy. Hepatobiliary Pancreat Dis Int 2005;4:450-455.
3 Rao AC, Gabriel G, Serrano J, Benedicto R. Inkwell pancreaticojejunal anastomosis after pancreaticoduodenectomy. Am J Surg 2004;187:410-412.
4 Landen S. Consolidation of a friable pancreas for pancreaticojejunal anastomosis. Dig Surg 1998;15:297-298.
5 Langrehr JM, Bahra M, Jacob D, Glanemann M, Neuhaus P. Prospective randomized comparison between a new mattress technique and Cattell (duct-to-mucosa) pancreaticojejunostomy for pancreatic resection. World J Surg 2005;29:1111-1121.
Received January 4, 2013
Accepted after revision April 29, 2013
(Hepatobiliary Pancreat Dis Int 2013;12:556-558)
AuthorAff i liations:Department of General Surgery, Baskent University Faculty of Medicine, Adana, Turkey (Torer N, Ezer A and Nursal TZ)
Nurkan Torer, MD, Department of General Surgery, Adana Research and Teaching Center, Baskent University, Dadaloglu Mah. 39. Sk. No. 6 Yuregir, Adana 01250, Turkey (Tel/Fax: 90-322-3271276; Email: ntorer@yahoo.com.tr)
© 2013, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(13)60088-0
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Simultaneous recovery of dual pathways for ammonia metabolism do not improve further detoxif i cation of ammonia in HepG2 cells
- Optimal central venous pressure during partial hepatectomy for hepatocellular carcinoma
- Risk factors and clinical characteristics of portal vein thrombosis after splenectomy in patients with liver cirrhosis
- Fine needle aspirating and cutting is superior to Tru-cut core needle in liver biopsy
- Diagnostic accuracy of enhanced liver fi brosis test to assess liver fi brosis in patients with chronic hepatitis C
- Retrohepatic vena cava deroof i ng in living donor liver transplantation for caudate hepatocellular carcinoma