EFNS 的神经病理性痛药物治疗指南:2010 修订
2012-11-04李建萍李焰生摘译
李建萍,李 颖,林 智,李焰生 摘译
(上海交通大学医学院附属仁济医院神经内科,上海 200127)
背景和目的
神经病理性痛(Neuropathic pain,NP)是由躯体感觉系统的病灶或疾病所导致[1],其发生率在欧洲总体人群中达7%~8%[2,3]。尽管以往的各种努力试图建立一个更为基本的治疗方法,但由于NP 对多数药物的反应不可预见,以致NP 的治疗仍颇为困难[4-6]。欧洲神经病学协会联盟(EFNS)在2006年提出了第1个NP 药物治疗指南[6],此后,针对各种NP 的新的随机对照试验(RCT)不断发表,使得指南的更新成为必然。本次目的是检索2005年以后发表的所有针对NP 的RCT,提出推荐意见以帮助选择针对NP 的治疗方案,出研究方案以澄清目前未决问题。
方法
在Cochrane 数据库中对2005年以来的相关研究进行了一个基本检索。如果不能找到针对某个NP 或者针对某个具有潜在有效性的药物的高级别研究,我们就将检索范围扩大到Medline和其他的电子数据库,包括未经发表的公司研究(2005年1 月~2009年9 月)。证据等级和推荐级别依据EFNS标准[8]。
入选标准包括:有对照的Ⅰ类或Ⅱ类研究(低级别研究仅在没有高级别研究的情况下入选);研究对象为很可能或确定的NP 或三叉神经痛的患者;慢性NP(≥3 月);疼痛为主要终点事件(排除以感觉减退为主要终点事件的研究,如化疗性神经病研究);样本量不少于10例患者;有明确的疗程和随访时间;治疗方案可应用于门诊患者;研究药物为目前已经使用或进入3 期临床研究的药物;全文以英语撰写。
排除标准包括:研究的患者组重复,无躯体感觉系统存在病损的证据(如复杂的局部疼痛综合征Ⅰ、纤维肌痛症、下背痛),使用无法验证的主要终点事件评估方法的研究;使用病因治疗(如α -硫辛酸治疗糖尿病)和预先治疗的研究。
我们重点关注药物治疗对于改善疼痛、症状/体征、生活质量、睡眠和情绪的有效性以及其相关的不良反应(见附录1和2)。
结果
检索到64 项2005年1 月以后发表的RCT,均使用安慰剂或活性药物作为参照系,分为3个亚组或者对先前的RCT 进行事后分析。
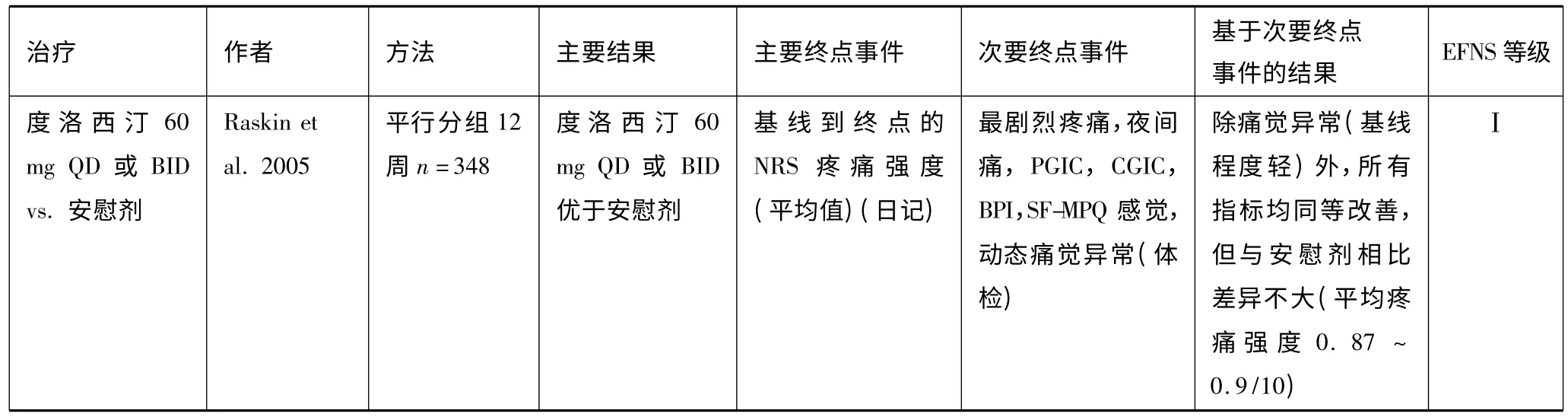
痛性多发性神经病
抗抑郁剂三环类抗抑郁剂(TCA)的疗效在痛性周围神经病(PPN)(主要是糖尿病性)治疗性试验中得到证实,包括3 项Ⅰ类或Ⅱ类的单中心研究[7,9,10]。3个RCT 报道文拉法辛在PPN 中的疗效,但对比研究显示其在受试者反应和生活质量上的疗效不及丙咪嗪[7,11]。不良作用主要是胃肠道反应,有5%患者出现血压升高和有临床意义的ECG 改变。度洛西汀在3个大样本的糖尿病性PPN 治疗研究中显示有效[12],1个企业资助的meta分析提示其具有与加巴喷丁、普瑞巴林类似的疗效[13],有效性可持续1年[14]。常见的不良作用包括恶心、嗜睡、口干、便秘、腹泻、多汗和头晕,由此导致的停药率达15%~20%[15,16]。度洛西汀没有或仅有轻微的心血管不良反应,但有肝毒性的罕见报道[15]。选择性5 -羟色胺再摄取抑制剂(SSRI)或米安舍林没有或仅有轻微的止痛效果[7,17]。
加巴喷丁和普瑞巴林对于糖尿病性PPN 有效[18,19],普瑞巴林的疗效呈现剂量依赖的形式[19]。1 项Ⅰ类试验显示加巴喷丁与去甲替林疗效相当[20]。不良反应包括头晕、嗜睡、周围性水肿、体重增加、虚弱、头痛和口干。在1 项比较研究中,口干多见于去甲替林,而注意集中困难多见于加巴喷丁[20]。普瑞巴林的停药率从0%(150 mg/d)[19]~20%(600 mg/d)[21]。其他抗癫 药物在NP 治疗研究的结果不一致。小样本的Ⅲ类研究提示卡马西平有效[7],但大样本安慰剂对照试验总体显示无效或有限疗效(见表1)[7,22-29]。无效的一个重要原因是安慰剂效应很大[30]。
阿片类羟考酮、曲马多[31,32]和曲马多与对乙酰氨基酚合剂[33]能够减轻糖尿病性PPN 的疼痛。不良反应主要有恶心和便秘,长期使用可导致药物滥用(1 项羟考酮治疗糖尿病性NP 的3年研究中,药物滥用的发生率为2.6%,更高的发生率也有报道)[4,34]。由于可能发生意识模糊,曲马多在老年患者中应慎用,不建议与SSRIs 合用[7,32]。曲马多与对乙酰氨基酚合剂的耐受性似乎更好一些[33]。
其他有研究报道A 型肉毒毒素[35]、硝酸盐衍生物[36,37]和一种烟碱激动剂(nicotinic agonist)[38]对NP 有效。其他PPN 治疗研究取得阳性结果的有左旋多巴,结果不一致的有N -甲基-D -天冬氨酸(NMDA)拮抗剂,其余均为有限疗效或者无效(见表1)[10,39]。
联合用药3 项Ⅰ类研究发现加巴喷丁加阿片类(吗啡、羟考酮)或加巴喷丁加去甲替林联合用药对于糖尿病性PN 的疗效优于单药使用,其中2 项研究包含有疱疹后神经痛(PHN)[20,40,41],而1 项小样本研究提示加巴喷丁与文拉法辛合用优于加巴喷丁与安慰剂合用[7]。
HIV神经病早期的人类免疫缺陷病毒(HIV)神经病治疗研究多数结果阴性(见表1)[7,42]。仅拉莫三嗪对接受抗病毒治疗的患者有一定的疗效[43]。近期的RCT 发现吸食大麻(使用1%~8%的四氢大麻酚5 d)可有效减轻疼痛程度,但无助于疼痛改善和功能[44,45]。不同浓度辣椒素贴剂疗效不一,但对感觉阈值无变化[46],但系统综述认为无效[47]。
推荐
推荐TCA、加巴喷丁、普瑞巴林和选择性5-HT及去甲肾上腺素再摄取抑制剂(SNRI)(度洛西汀、文拉法辛)作为PPN 的一线治疗用药(尤其是糖尿病相关性)(A 级证据)。曲马多作为二线用药(A 级证据),除非疼痛加剧(曲马多对乙酰氨基酚合剂)或同时合并有显著的非NP(鉴于曲马多对伤害性疼痛的确切疗效)。三线治疗包括强效阿片类,但考虑到其长期用药的安全性,包括成瘾的可能和滥用,需要进一步的RCT 研究证据。表1 列举了无效或效果不肯定的治疗药物。对HIV 相关性多发性神经病,只有拉莫三嗪(接受抗逆转录病毒治疗的患者)(B 级证据)、大麻(A 级证据)和辣椒素贴剂(A 级证据)被证明有一定疗效。
疱疹后神经痛
抗抑郁药物系统综述显示TCA 治疗PHN 有效,且疗效优于SSRI[7,50]。没有关于SNRI 的试验。
加巴喷丁和普瑞巴林对PHN 有效,比较研究显示加巴喷丁与去甲替林无疗效差别[20,49]。加巴喷丁缓释剂的疗效优于安慰剂[50]。小样本的RCT 报道丙戊酸钠对PHN 有较好的疗效[51],但试验仅报道了完成试验者的数据[52]。
阿片类羟考酮、吗啡和美沙酮对PHN 有效[49]。1 项比较试验提示三者等效或略优于TCA,但患者常因不良反应而停药[7,49]。1个关于曲马多的I 类研究得出阴性结果[7]。
局部用药5 项Ⅰ类或Ⅱ类的RCT 证实5%利多卡因对PHN 伴轻触诱发性痛觉异常(allodynia)有效,但疗效仅稍优于安慰剂,且较全身用药疗效差[7,53]。1个大型试验入选伴或不伴痛觉异常患者,主要结局阴性,但入选患者的基线资料不均衡[54]。非盲法开放试验提示利多卡因软膏比普瑞巴林有更好的耐受性[55]。利多卡因软膏因其系统吸收率低,仅有局部的不良反应(轻微的皮肤反应)而安全性高,耐受性良好[54,56]。RCT 已证实0.075%辣椒素局部用药有效[7],但因引起局部烧灼感,故盲法设计被破坏。在12 周的研究中,高浓度辣椒素贴剂的疗效优于低浓度贴剂[57]。不良反应主要是用药部位疼痛、红斑。系统综述显示辣椒素贴剂有效[47]。
其他NMDA 拮抗剂、劳拉西泮和选择性Cox-2抑制剂不能缓解PHN 的疼痛症状(见表1)[7,58]。
推荐推荐TCA 或加巴喷丁/普瑞巴林作为PHN 的一线治疗用药(A 级证据)。局部利多卡因软膏(A 级证据,结果有轻度不一致性)以其优良的耐受性可考虑作为老年患者的一线用药,尤其是在担心口服药物产生中枢神经系统不良反应的情况下。对于这样的患者,可以先试用利多卡因软膏2~4 周后再考虑其他治疗。推荐强效阿片类(A 级证据)和辣椒素霜作为二线用药(见第1 部分)。辣椒素贴剂是有效的(A 级证据),但反复使用后的长期作用尤其是对感觉的影响尚不清楚。
三叉神经痛
三叉神经痛(TN)的典型表现是非常短暂的疼痛发作(电击样),可分为经典性和症状性。前者继发于血管压迫三叉神经或未能发现明确病因,后者继发于桥小脑角的占位或多发性硬化[59]。
卡马西平,奥卡西平卡马西平是TN 的首选药物,但其疗效受到耐受性不佳和药代动力学相互作用的限制。2 项Ⅱ类RCT 发现奥卡西平在减少疼痛发作次数和改善综合评价方面与卡马西平疗效相当[60,61]。
其他小样本研究报道数种药物(拉莫三嗪、巴氯芬)对TN 有效(见表1)[61,62],但Cochrane 综述认为目前的证据不足以推荐这些药物用于TN[63]。还有小型非盲研究提示肉毒毒素-A和一些抗癫 药物对TN 有疗效。
症状性TN对于多发性硬化引起的TN,只有一些小样本的非盲法的Ⅳ类研究[62]。一项小型的开放性研究亦显示肉毒毒素-A和某些抗癫 药物有效[62,64,65](表1)。
推荐与以前的指南意见一致[7,61,62],卡马西平(A 级证据)和奥卡西平(B 级证据)被证实为典型性TN 的一线用药。因奥卡西平的药物相互作用小,可作为首选。若患者出现无法耐受的不良反应,可使用拉莫三嗪(C 级证据),但也应考虑外科手术干预。
中枢性神经病理性痛
最常见的中枢性神经病理性痛(CP)由中枢性卒中后疼痛(CPSP)、脊髓损伤(SCI)或多发性硬化(MS)引起。
抗抑郁剂TCA 治疗CPSP 有效,但TCA 治疗SCI 疼痛的1个大规模试验却得出阴性结果,原因可能是治疗剂量偏低且缺乏特异性评价指标[7,66]。针对SCI 的RCT 显示大剂量阿米替林(150 mg/d)较之苯海拉明和加巴喷丁(3 600 mg/d)能够更有效地缓解伴有抑郁者的疼痛[67]。尽管研究有局限性,但提示TCA 可用于治疗SCI 患者,特别是那些患有抑郁症的患者。尚没有开展SNRI 对CP 的RCT。
1 项多中心研究报道普瑞巴林对外伤性SCI 疼痛的疗效[68],单中心研究则证实普瑞巴林可用于治疗各种CP[20,69]。加巴喷丁和拉莫三嗪的研究结果不一致[7,43,67,70]。其他抗癫 药物未发现有效[7,71](见表1)。
阿片类仅1 项研究比较了大剂量和小剂量的左啡诺对周围性或中枢性NP 患者的疗效[72]。1个RCT 发现曲马多能减轻疼痛强度,但不能改善疼痛的影响,并且因多种不良反应致43%的患者脱落(安慰剂组的脱落率为17%)[73]。
大麻两项Ⅰ类研究报道大麻(四氢大麻酚,口腔黏膜喷雾,2.7 mg 的δ -9 -四氢大麻酚/2.5 mg大麻二酚)对MS 相关疼痛有效[7]。随访3年,发现90%的患者出现不良反应(头晕、口干、镇静、疲劳、胃肠道反应、口腔不适),但无耐受性发生[74]。
其他小剂量美西律对SCI 疼痛无效。S -氯胺酮(S-ketamine)经皮电离子透入疗法对CP 无效[7,75]。
推荐推荐普瑞巴林(A 级证据)、阿米替林(B级证据)或加巴喷丁为CP 的一线治疗药物。曲马多(B 级证据)为二线药物。在不需要长期治疗的情况下,推荐强效阿片类(B 级证据)为二线或三线用药。拉莫三嗪可用于治疗CPSP 或伴有轻触诱发性痛觉异常的不完全脊髓损伤性SCI 疼痛(B 级证据)。大麻(A 级证据)仅在其他所有治疗无效的情况下用于治疗MS 相关性疼痛。
其他情况
针对其他NP 的治疗药物的证据等级(见表2)。
癌性NP:A 级证据证实加巴喷丁有效(1个研究),B 级证据证明TCA和曲马多有效,丙戊酸钠无效[7,76,77]。外伤性NP:1 项多大型试验显示加巴喷丁对主要结局无效[78],但改善了数个次要结局;虽然有效反应的预测因素尚有待确定,但加巴喷丁可能对某些亚组患者有益(A 级证据)。B 级证据证实抗抑郁剂的疗效,有报道肉毒毒素-A 有较,其他药物却无效或不一致结果[79,80]。神经根病:加巴喷丁(A级证据)、TCA和阿片类以及两者的复合制剂(B 级证据)无效或仅有轻微疗效[81-83]。幻肢痛:曲马多和吗啡有效(A 级证据),加巴喷丁的疗效不一致[84,85]。多重病因NP:有效药物是抗抑郁剂(安非他酮、TCA)、阿片类(左啡诺、美沙酮)和大麻[7,86-92]。
对疼痛症状和体征的效果及有效反应的预测因素
RCT 越来越多地评估疼痛的症状和体征[60],并提示不同药物对不同性质的NP(如灼痛、深部痛、发作性疼痛)有不同的疗效[7,93,94]。一些药物(TCA、普瑞巴林、大麻、利多卡因、文拉法辛、NMDA 拮抗剂)可减轻轻触诱发的和(或)机械性痛觉异常[7,50,87,88,95]。虽事后分析显示阿片类和利多卡因软膏可能有疗效的预示因素[79,96,97],但还没有基于基线疼痛资料的用以查找有效性预测因素的RCT 设计(C 级证据)。
对生活质量、睡眠和情绪的影响
NP 患者的生活质量(QOL)、睡眠和情绪深受疼痛影响[98,99]。通常,药物对疼痛的疗效与QOL 的改善相关[100]。试验证实度洛西汀、普瑞巴林和加巴喷丁对这些事件有益[7,40,99,101]。普瑞巴林和加巴喷丁改善睡眠的效果最为肯定[40,98],6 项研究显示普瑞巴林改善QOL 或情绪的作用不佳。3个试验报道TCA可改善QOL[40,90,102]。阿片类和曲马多能减轻疼痛对睡眠的影响,但对QOL 的疗效不一致[99];大麻可以改善QOL 或睡眠[44,45,87],但总体而言这些药物对改善情绪无效[32,72,73,76,87]。
对未来试验的推荐建议
本修订指南证实TCA(25~150 mg/d)、加巴喷丁(1 200~3 600 mg/d)和普瑞巴林(150~600 mg/d)为各种NP(除TN)的一线用药,利多卡因软膏为PHN,尤其是老年人的一线药物(3 次/d)。基于证据,推荐SNRI(度洛西汀60~120 mg/d、文拉法辛150~225 mg/d)为痛性糖尿病性多发性神经病的一线用药。TCA 价格便宜[98],但在大剂量及在老年人使用时存在安全性问题,并且有对比研究提示TCA 疗效不及加巴喷丁[20]。相比加巴喷丁,普瑞巴林具有药代动力学优势(每日2 次给药,疗效呈剂量依赖性),但meta分析提示两者的疗效和耐受性相近。二线治疗药物包括曲马多(200~400 mg/d)及辣椒素霜治疗PHN。尽管强效阿片类对非癌性NP 的疗效确切,但由于长期使用有发生滥用的潜在风险,且目前仍然缺乏长期治疗NP 的安全性研究,因此强效阿片类推荐作为二线/三线用药。辣椒素贴剂对痛性HIV神经病或PHN 有效(A 级证据)。大麻推荐用于难治性病例(MS和周围性NP,A 级证据)。联合用药推荐用于对单一药物反应不佳的患者(加巴喷丁加阿片类或加TCA,A 级证据)。
目前,对不同治疗的选择主要基于其各自的效益/风险比及患者的临床状况(共病、禁忌证、其他治疗)。近期对2 000 多例糖尿病性神经病和PHN 的研究[103]显示,可按患者的感觉特征进行亚组分类;基于感觉特征而非病因的分类方法,有助于最大限度地减少同一研究组别病理生理学的异质性,提高对治疗反应[104,105]。
未来试验的策略应该是:①有效性应基于标准化的结局[60],应包括总体疼痛、相关症状和体征、QOL;②使用感觉检查和特定的疼痛问卷对症状和体征进行详细的描述以确定治疗有效者的特征,有助于提高治疗成功率;③使用统一的有害事件评估标准;④开展大型的药物对比研究;⑤需要更多的大型研究以确定联合用药的疗效。
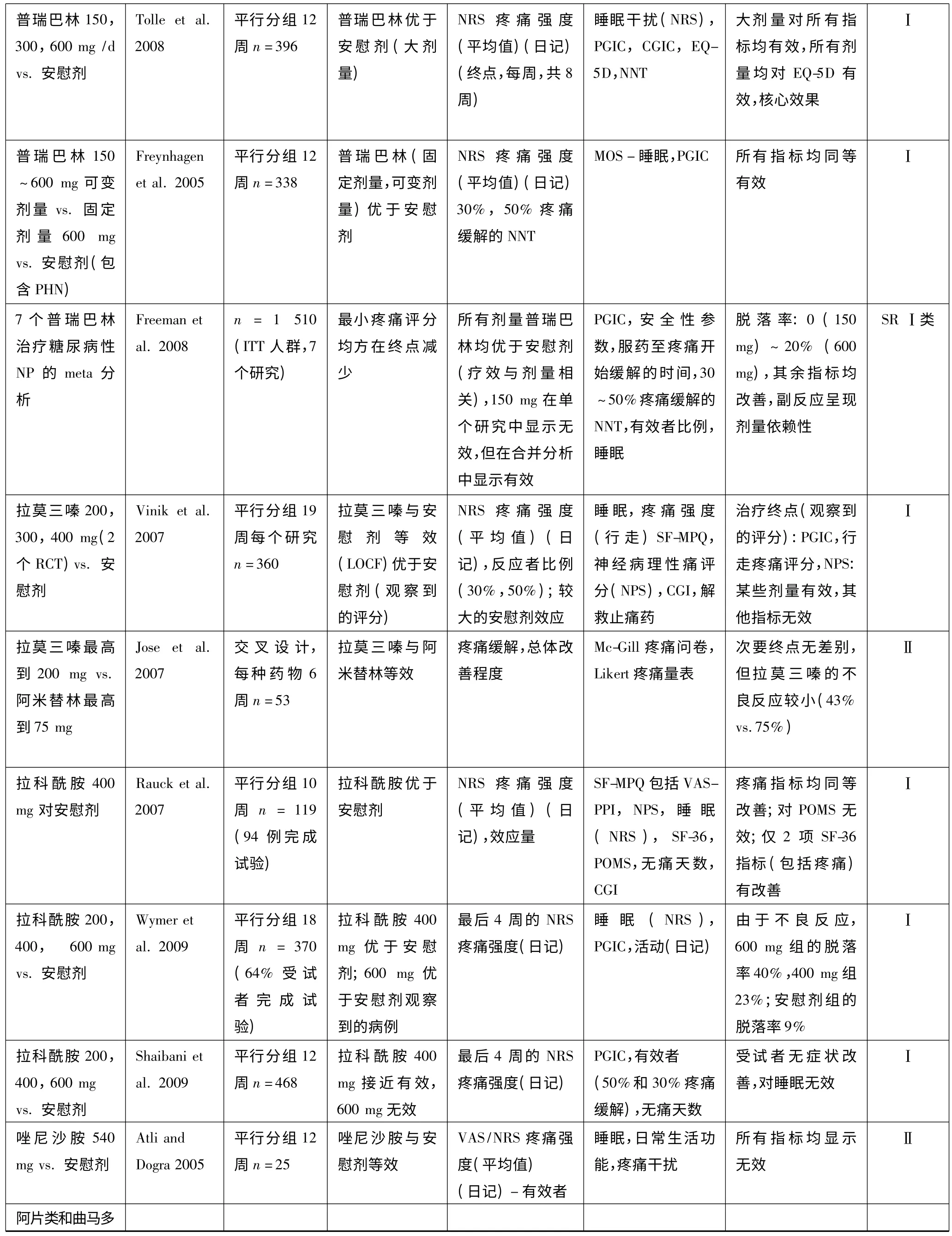
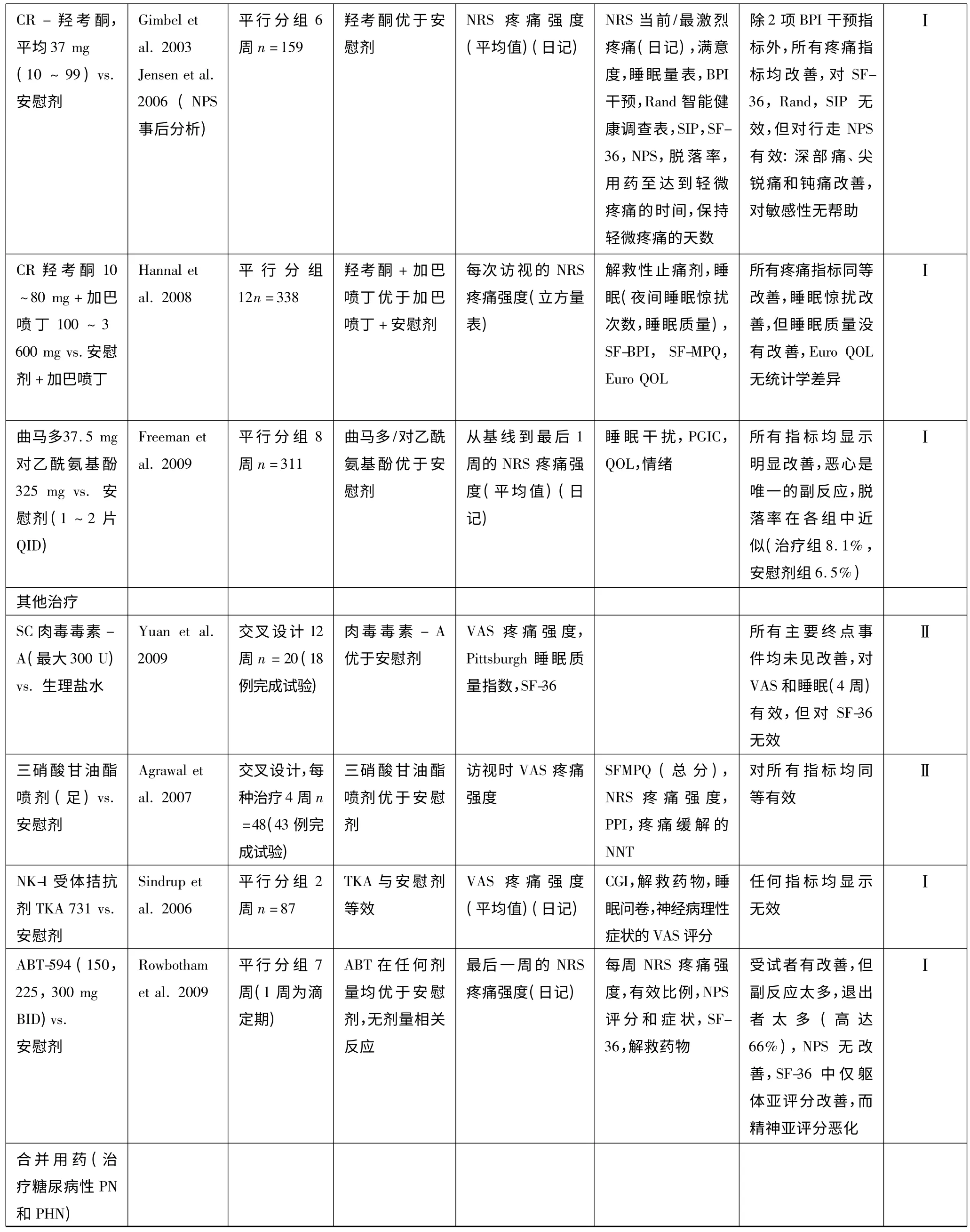
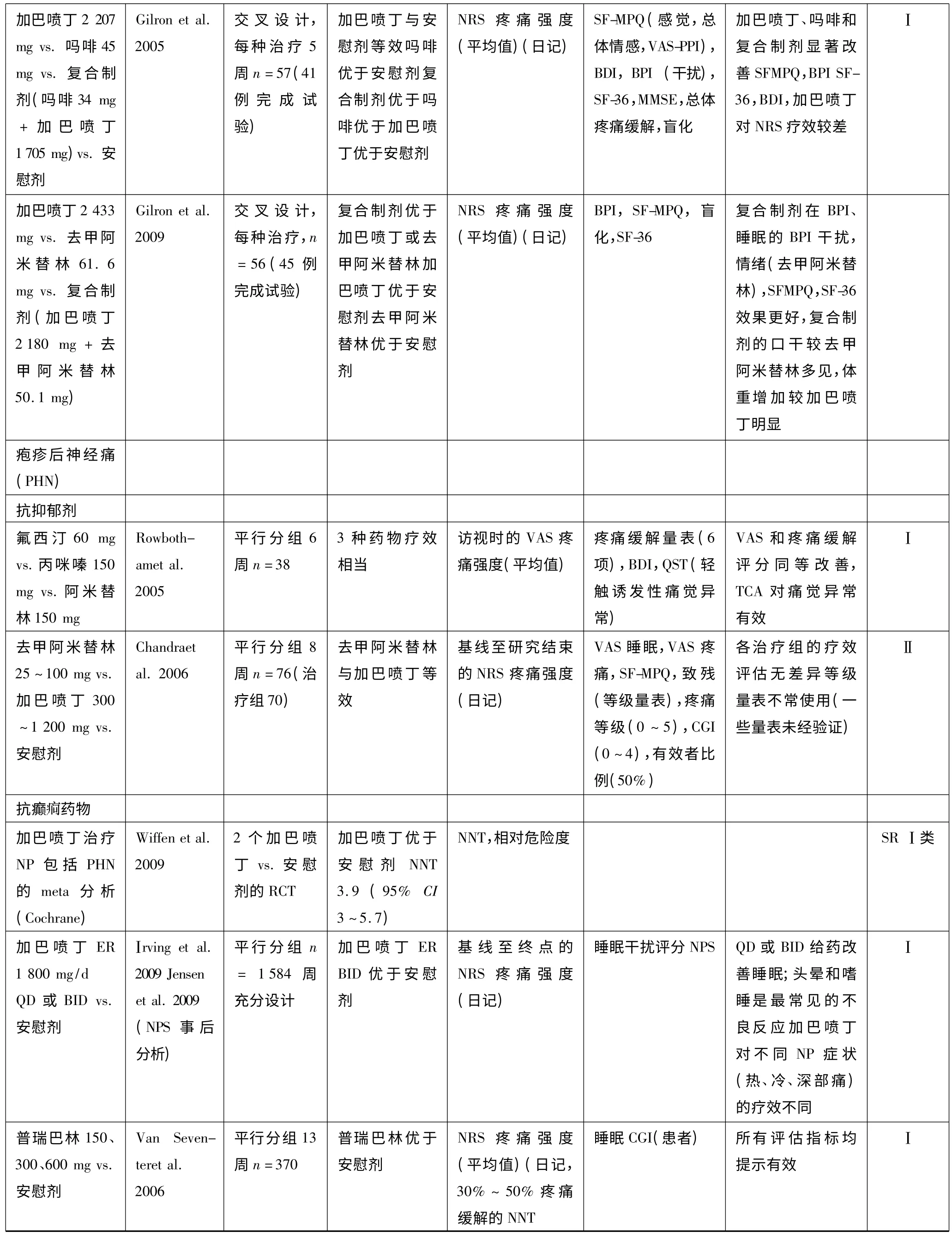
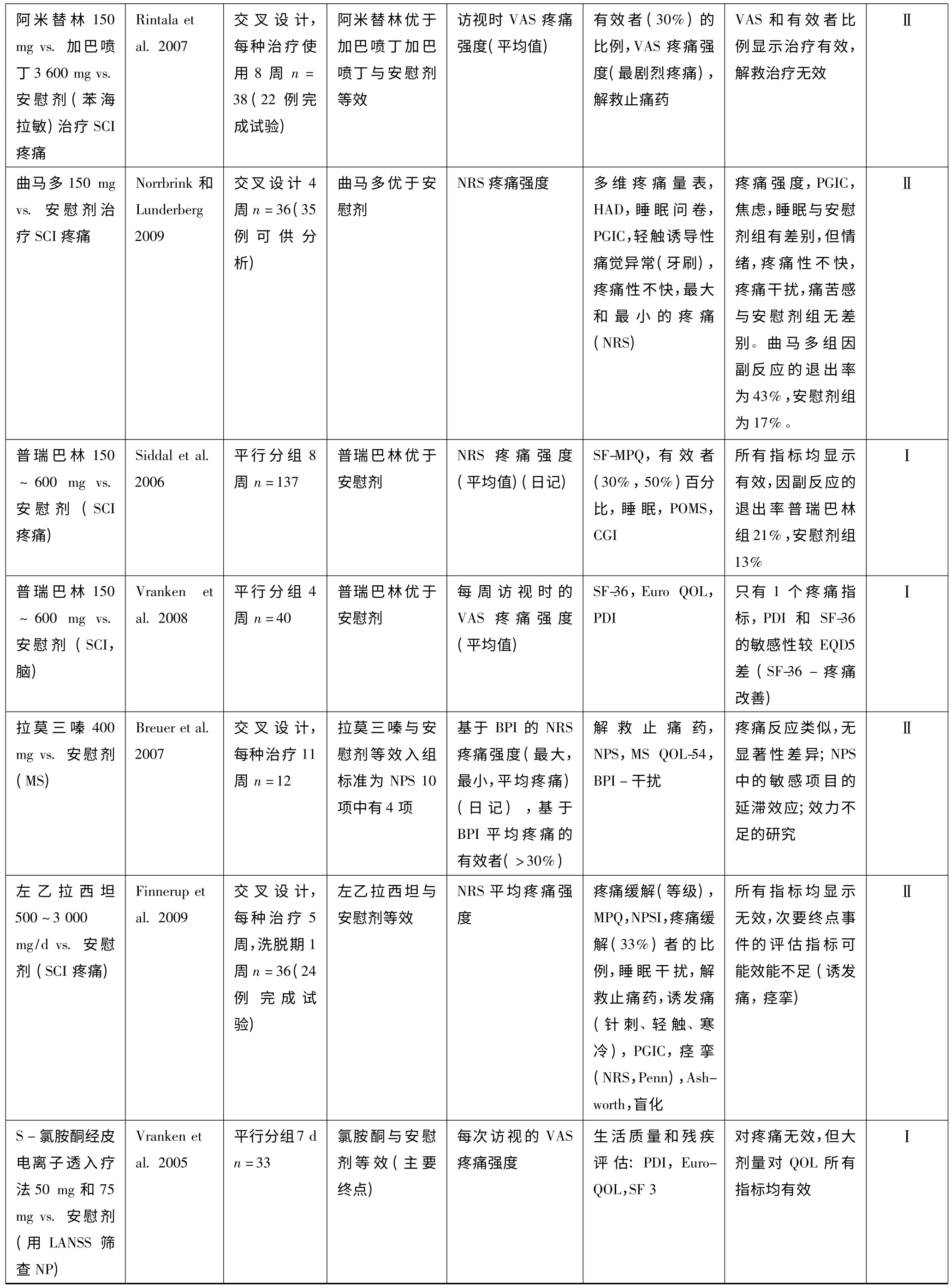
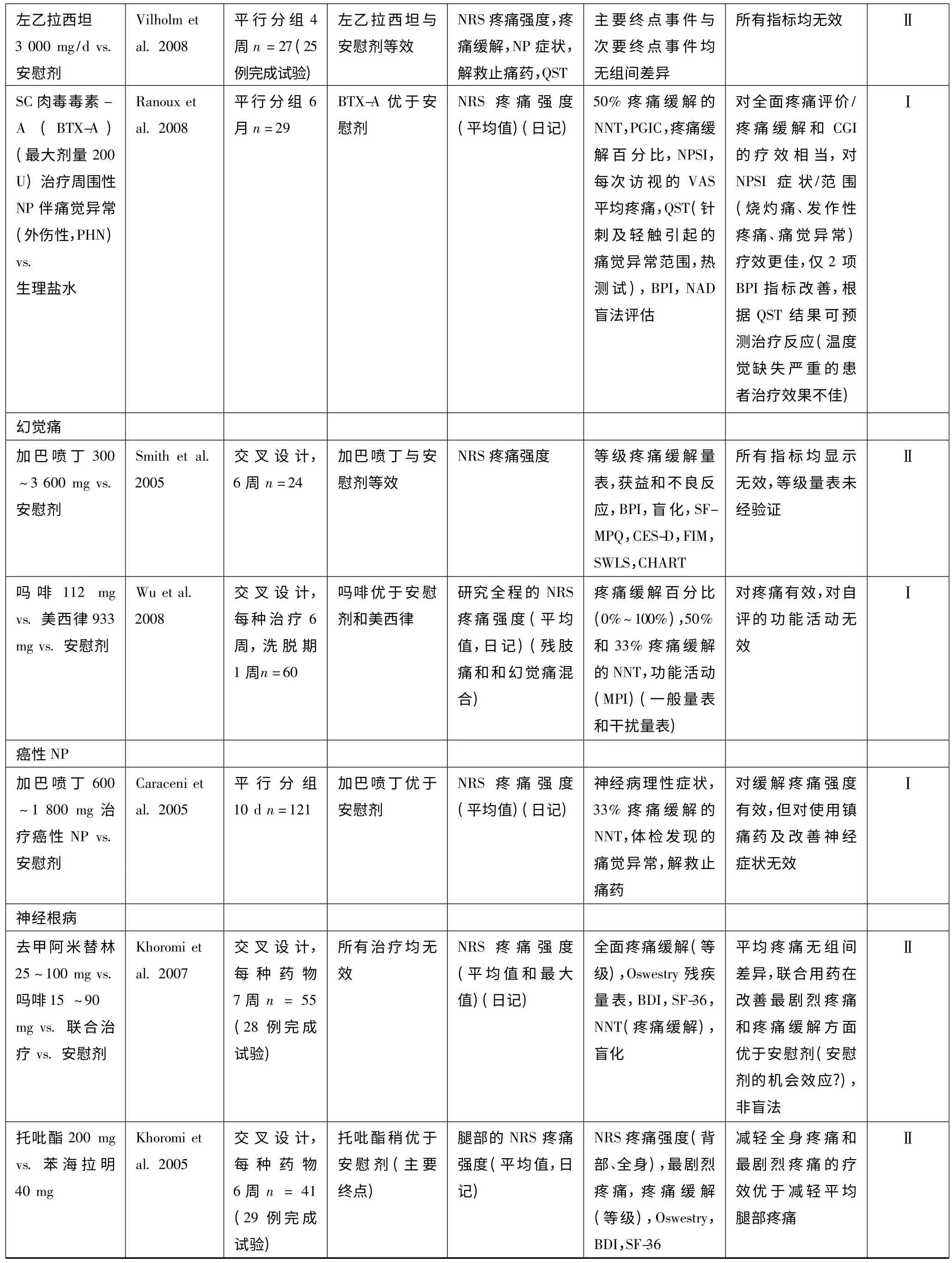
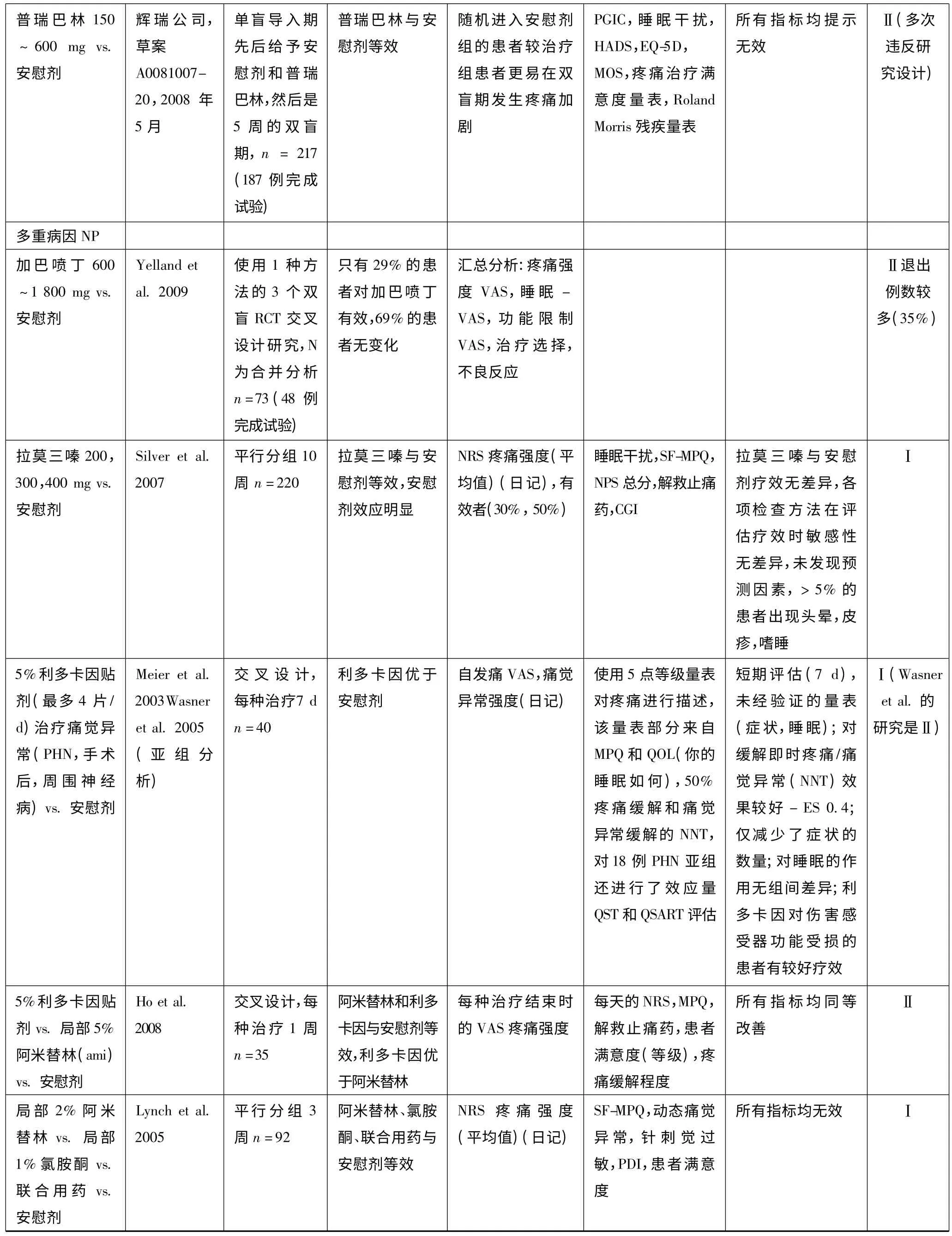
表1 常见神经病理性痛药物治疗研究的证据分级和使用建议
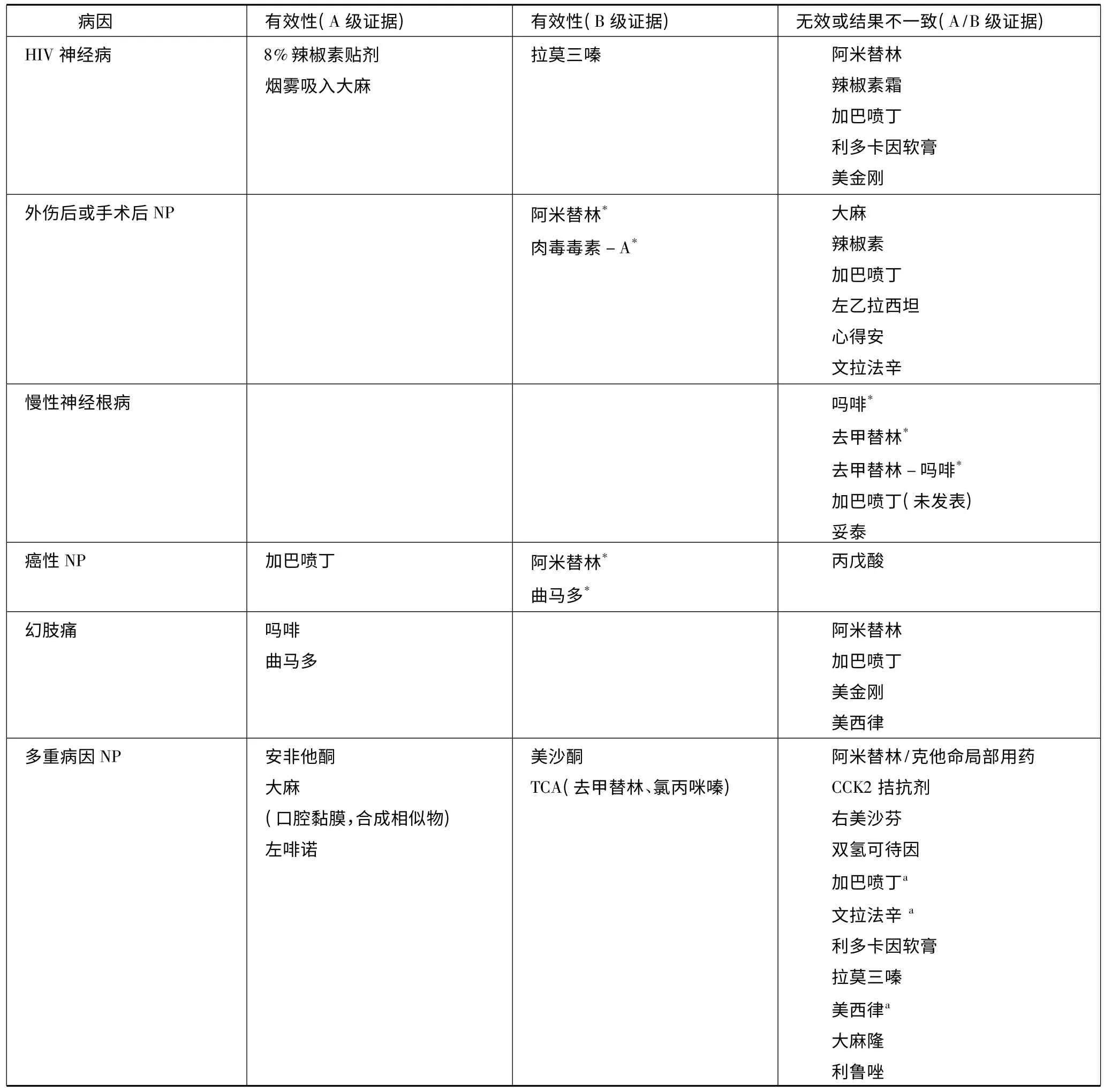
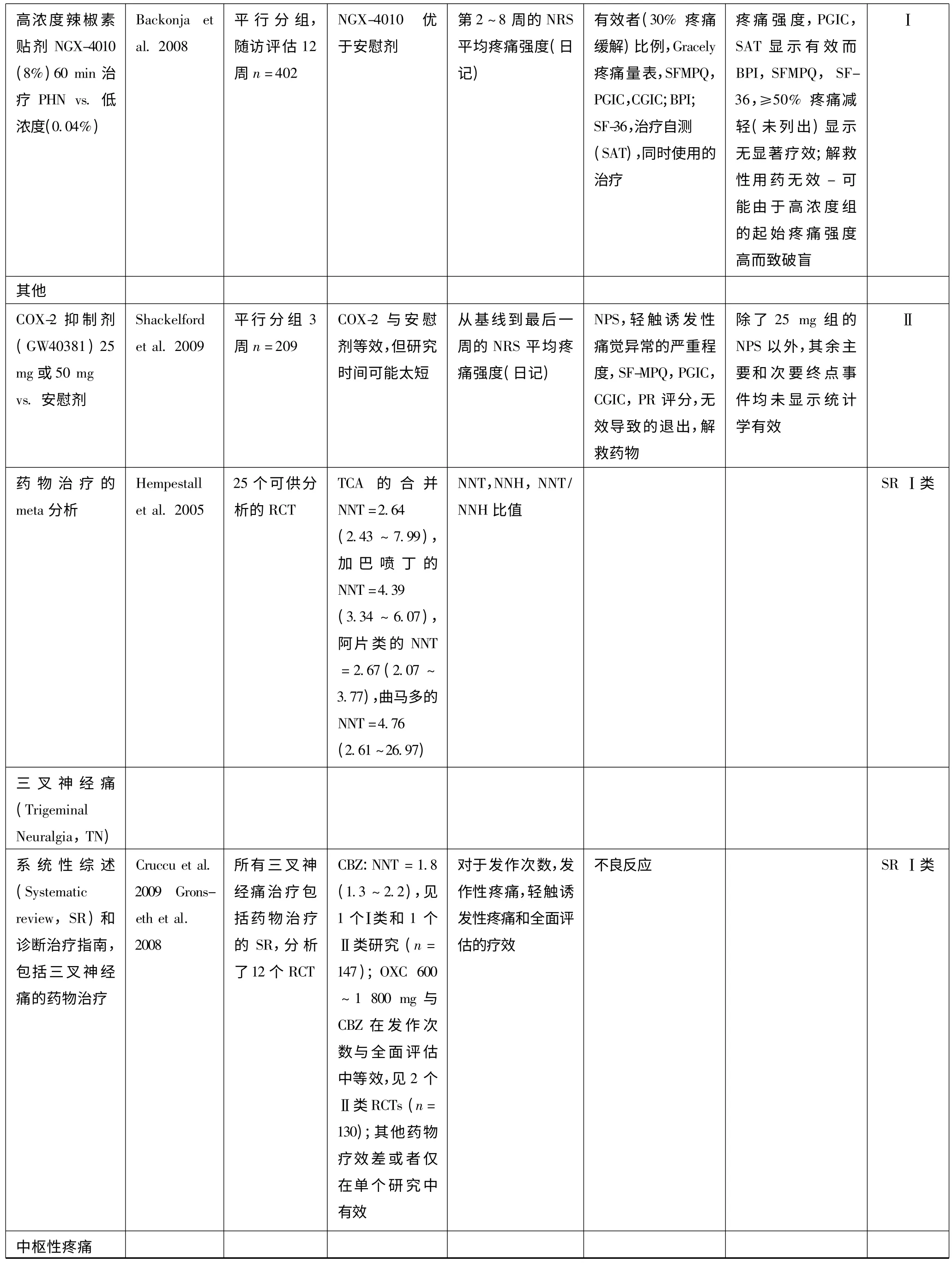
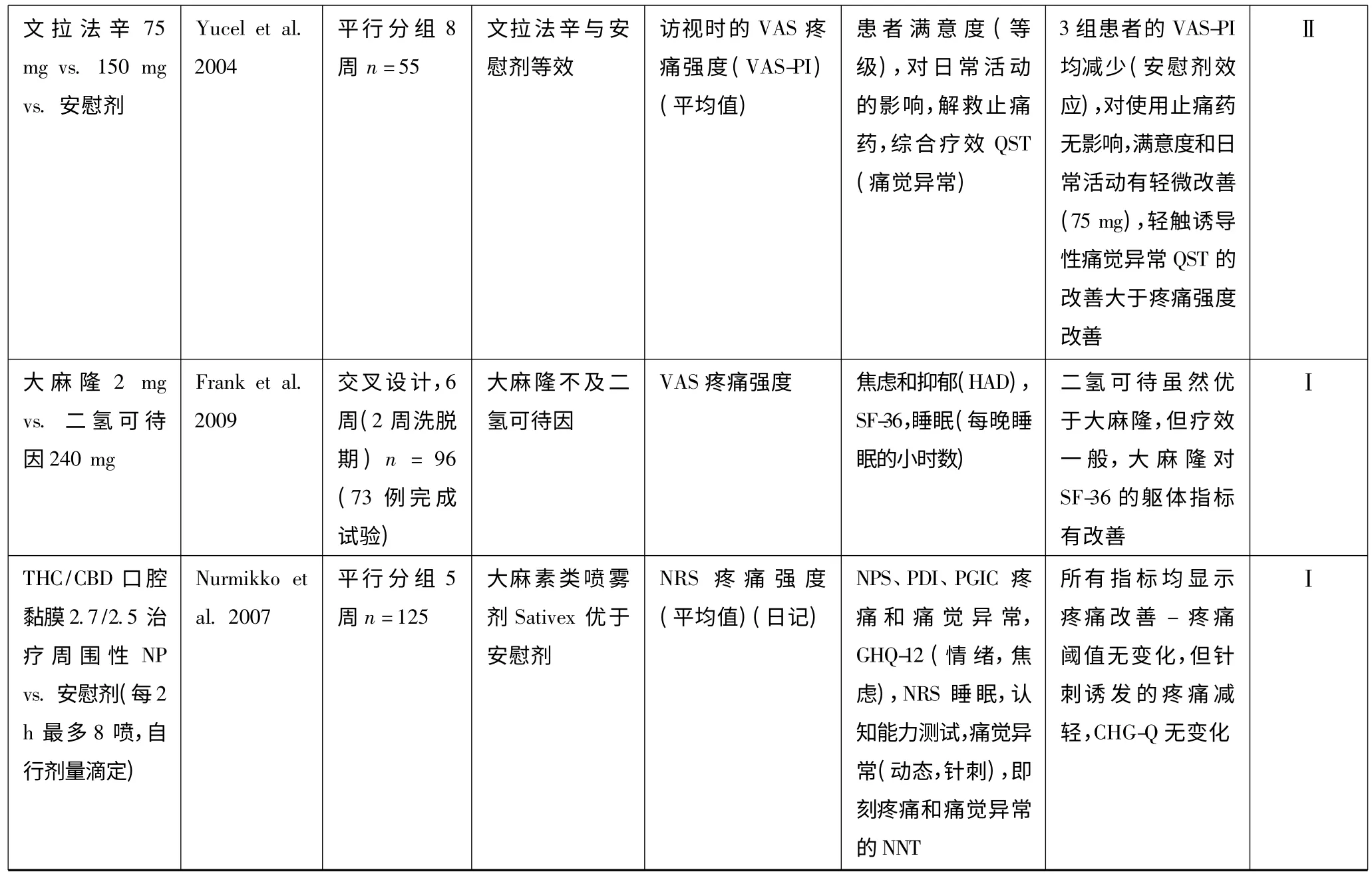
表2 少见的神经病理性痛的药物治疗研究的证据分级
附录1



BDI,贝克抑郁自评问卷;BOCF,基线观察推进法;BPI,简明疼痛问卷;CGIC,临床变化总体印象;HDRS,汉密尔顿抑郁量表;LANSS,利兹神经病理性症状和体征量表;LOCF,末次观测值结转法;MDI,重症抑郁问卷;MMSE,简易智能状态检查;MPI,多维疼痛调查表;MPQ,Mc Gill 疼痛问卷;NIS,神经病变损伤评分;NNT:需要治疗的病例数;NPS,神经病理性痛量表;NPSI,神经病理性痛症状问卷;NRS,数字疼痛分级量表(或Likert 量表);NS,无显著性;NWC,选出词的总数;PDI,疼痛残疾指数;PHN,疱疹后神经痛;PN,多发性神经病;PGIC,患者对临床变化总体印象;POMS,心境状态量表;PPI,现时疼痛强度;QST,定量感觉检查;SF-MPQ,Mc Gill 疼痛问卷简表;SIP,疼痛影响程度量表;SF-36,医疗结局研究36 条目健康调查简表(生活治疗指标);STAI,斯皮尔伯格特质焦虑量表;Trt,治疗;VAS,视觉模拟量表;VRS,语言描述量表;vs.,比。
[1]Treede RD,Jensen TS,Campbell JN,et al.Neuropathic pain:redefinition and a grading system for clinical and research purposes[J].Neurology,2008,70:1630 -1635.
[2]Bouhassira D,Lantéri-Minet M,Attal N,et al.Prevalence of chronic pain with neuropathic characteristics in the general population[J].Pain,2008,136:380 -387.
[3]Torrance N,Smith BH,Bennett MI,et al.The epidemiology of chronic pain of predominantly neuropathic origin.Resultsfrom a general population survey[J].J Pain,2006,7:281 -289.
[4]Dworkin RH,O'Connor AB,Backonja M,et al.Pharmacologic management of neuropathic pain:evidence based recommendations[J].Pain,2007,132:237 -251.
[5]Finnerup NB,Jensen TS.Mechanisms of disease:mechanism-based classification of neuropathic pain-a critical analysis[J].Nat Clin Pract Neurol,2006,2:107 -115.
[6]Baron R.Mechanisms of disease:neuropathic pain:a clinical perspective[J].Nat Clin Pract Neurol,2006,2:95 -106.
[7]Attal N,Cruccu G,Haanpää M,et al.EFNS guidelines on pharmacological treatment of neuropathic pain[J].Eur J Neurol,2006,13:1153 -1169.
[8]Brainin M,Barnes M,Baron JC,et al.Guidance for the preparation of neurological management guidelines by EFNS scientific task forces-revised recommendations[J].Eur J Neurol,2004,11:577-581.
[9]Saarto T,Wiffen PJ.Antidepressants for neuropathic pain[J].Cochrane Database Syst Rev,2007,4:CD005454.
[10]Finnerup NB,Otto M,McQuay HJ,et al.Algorithm for neuropathic pain treatment:an evidence based proposal[J].Pain,2005,118:289 -305.
[11]Kadiroglu AK,Sit D,Kayabasi H,et al.The effect of venlafaxine HCl on painful peripheral diabetic neuropathy in patients with type 2 diabetes mellitus[J].J Diabetes Complications,2008,22:241 -245.
[12]Kajdasz DK,Iyengar S,Desaiah D,et al.Duloxetine for the management of diabetic peripheral neuropathic pain:evidence-based findings from post hoc analysis of three multicenter,randomized,double-blind,placebo-controlled,parallel-group studies[J].Clin Ther,2007,29 (Suppl):2536 -2546.
[13]Quilici S,Chancellor J,Löthgren M,et al.Meta-analysis of duloxetine vs.pregabalin and gabapentin in the treatment of diabetic peripheral neuropathic pain[J].BMC Neurol,2009,9:6.
[14]Skljarevski V,Desaiah D,Zhang Q,et al.Evaluating the maintenance of effect of duloxetine in patients with diabetic peripheral neuropathic pain[J].Diab Met Res Rev,2009,25:623 -631.
[15]Gahimer J,Wernicke J,Yalcin I,et al.A retrospective pooled analysis of duloxetine safety in 23,983 subjects[J].Curr Med Res Opin,2007,23:175 -184.
[16]Sultan A,Gaskell H,Derry S,et al.Duloxetine for painful diabetic neuropathy and fibromyalgia pain:systematic review of randomised trials[J].BMC Neurol,2008,8:29.
[17]Otto M,Bach FW,Jensen TS,et al.Escitalopram in painful polyneuropathy:a randomized,placebo-controlled,cross-over trial[J].Pain,2008,139:275 -283.
[18]Wiffen P,McQuay H,Edwards J,et al.Gabapentin for acute and chronic pain[J].Cochrane Database Syst Rev,2005,20:CD005452.
[19]Freeman R,Durso-Decruz E,Emir B.Efficacy,safety and tolerability of pregabalin treatment for painful diabetic peripheral neuropathy,findings from seven randomized controlled trials across a range of doses[J].Diabetes Care,2008,31:1448 -1454.
[20]Gilron I,Baley JM,Tu D,et al.Nortriptyline and gabapentin,alone and in combination for neuropathic pain:a double-blind,randomised controlled crossover trial[J].Lancet,2009,374:1252 -1261.
[21]Moore RA,Straube S,Wiffen PJ,et al.Pregabalin for acute and chronic pain in adults[J].Cochrane Database Syst Rev,2009,3:CD007076.
[22]Rauck RL,Shaibani A,Biton V,et al.Lacosamide in painful diabetic peripheral neuropathy:a phase 2 double-blind placebo-controlled study[J].Clin J Pain,2007,23:150 -158.
[23]Wymer JP,Simpson J,Sen J,et al.Efficacy and safety of lacosamide in diabetic neuropathic pain:an 18 weeks double blind placebo controlled trial of fixed doses regimens[J].Clin J Pain,2009,25:376 -385.
[24]Dogra S,Beydoun S,Mazzola J,et al.Oxcarbazepine in painful diabetic neuropathy:a randomized,placebo-controlled study[J].Eur J Pain,2005,9:543 -554.
[25]Grosskopf J,Mazzola J,Wan Y,et al.A randomized,placebo-controlled study of oxcarbazepine in painful diabetic neuropathy[J].Acta Neurol Scand,2006,114:177 -180.
[26]Beydoun A,Shaibani A,Hopwood M,et al.Oxcarbazepine in painful diabetic neuropathy:results of a dose-ranging study[J].Acta Neurol Scand,2006,113:395 -404.
[27]Vinik AI,Tuchman M,Safirstein B,et al.Lamotrigine for treatment of pain associated with diabetic neuropathy:results of two randomized,double-blind,placebo-controlled studies[J].Pain,2007,128:169 -179.
[28]Atli A,Dogra S.Zonisamide in the treatment of painful diabetic neuropathy:a randomized,double-blind,placebo-controlled pilot study[J].Pain Med,2005,6:225 -234.
[29]Shaibani A,Fares S,Selam JL,et al.Lacosamide in painful diabetic neuropathy:an 18-week double-blind placebo-controlled trial[J].J Pain,2009,10:818 -828.
[30]Katz J,Finnerup NB,Dworkin RH.Clinical outcome in neuropathic pain :relationship to study characteristics[J].Neurology,2008,28:263 -272.
[31]Eisenberg E,McNicol ED,Carr DB.Efficacy of muopioid agonists in the treatment of evoked neuropathic pain:systematic review of randomized controlled trials[J].Eur J Pain,2006,10:667 -676.
[32]Hollingshead J,Dühmke RM,Cornblath DR.Tramadol for neuropathic pain[J].Cochrane Database Syst Rev,2006,3:CD003726.
[33]Freeman R,Raskin P,Hewitt DJ,et al.Randomized study of tramadol/acetaminophen versus placebo in painful diabetic peripheral neuropathy[J].Curr Med Res Opin,2007,23:147 -161.
[34]Portenoy RK,Farrar JT,Backonja MM,et al.Longterm use of controlled-release oxycodone for noncancer pain:results of a 3-year registry study[J].Clin J Pain,2007,23:287 -299.
[35]Yuan RY,Sheu JJ,Yu JM,et al.Botulinum toxin for diabetic neuropathic pain:a randomized double-blind crossover trial[J].Neurology,2009,72:1473 -1478.
[36]Yuen KC,Baker NR,Rayman G.Treatment of chronic painful diabetic neuropathy with isosorbide dinitrate spray:a double-blind placebo-controlled cross-over study[J].Diabetes Care,2002,25:1699 -1703.
[37]Agrawal RP,Choudhary R,Sharma P,et al.Glyceryl trinitrate spray in the management of painful diabetic neuropathy:a randomized double blind placebo controlled cross-over study[J].Diabetes Res Clin Pract,2007,77:161 -167.
[38]Rowbotham MC,RachelDuan W,Thomas J,et al.A randomized,double-blind,placebocontrolled trial evaluating the efficacy and safety of ABT-594 in patients with diabetic peripheral neuropathic pain[J].Pain,2009,146:245 -252.
[39]Sindrup SH,Graf A,Sfikas N.The NK1-receptor antagonist TKA731 in painful diabetic neuropathy:a randomised,controlled trial[J].Eur J Pain,2006,10:567 -571.
[40]Gilron I,Bailey JM,Tu D,et al.Morphine,gabapentin,or their combination for neuropathic pain[J].N Engl J Med,2005,352:1324 -1334.
[41]Hanna M,O_Brien C,Wilson MC.Prolonged-release oxycodone enhances the effects of existing gabapentin therapy in painful diabetic neuropathy patients[J].Eur J Pain,2008,12:804 -813.
[42]Schifitto G,Yiannoutsos CT,Simpson DM,et al.A placebo-controlled study of memantine for the treatment of human immunodeficiency virus-associated sensory neuropathy[J].J Neurovirol,2006,12:328 -331.
[43]Wiffen PJ,Rees J.Lamotrigine for acute and chronic pain[J].Cochrane Database Syst Rev,2007,2:CD006044.
[44]Abrams DI,Jay CA,Shade SB,et al.Cannabis in painful HIV-associated sensory neuropathy:a randomized placebo-controlled trial[J].Neurology,2007,68:515 -521.
[45]Ellis RJ,Toperoff W,Vaida F,et al.Smoked medicinal cannabis for neuropathic pain in HIV:a randomized,crossover clinical trial[J].Neuropsychopharmacology,2009,34:672 -680.
[46]Simpson DM,Brown S,Tobias J,et al.Controlled trial of high-concentration capsaicin patch for treatment of painful HIV neuropathy[J].Neurology,2008,70:2305 -2313.
[47]Noto C,Pappagallo M,Szallasi A.NGX-4010,a highconcentration capsaicin dermal patch for lasting relief of peripheral neuropathic pain[J].Curr Opin Investig Drugs,2009,10:702 -710.
[48]Eisenberg E,McNicol ED,Carr DB.Efficacy and safety of opioid agonists in the treatment of neuropathic pain of nonmalignant origin:systematic review and meta-analysis of randomized controlled trials[J].JAMA,2005,293:3043 -3052.
[49]Hempenstall K,Nurmikko TJ,Johnson RW,et al.Analgesic therapy in postherpetic neuralgia:a quantitative systematic review[J].PLOS Medicine,2005,2:e164.
[50]Rowbotham MC,Reisner LA,Davies PS,et al.Treatment response in antidepressant-naive postherpetic neuralgia patients:doubleblind,randomized trial[J].J Pain,2005,6:741 -746.
[51]Irving G,Jensen M,Cramer M,et al.Efficacy and tolerability of gastric-retentive gabapentin for the treatment of postherpetic neuralgia[J].Clin J Pain,2009,25:185 -192.
[52]Chandra K,Shafiq N,Pandhi P,et al.Gabapentin versus nortriptyline in post-herpetic neuralgia patients:a randomized,double-blind clinical trial-the GONIP Trial[J].Int J Clin Pharmacol Ther,2006,44:358 -363.
[53]Khaliq W,Alam S,Puri N.Topical lidocaine for the treatment of postherpetic neuralgia[J].Cochrane Database Syst Rev,2007,18:CD004846.
[54]Binder A,Bruxelle J,Rogers P,et al.Topical 5% lidocaine (lignocaine)medicated plaster treatment for post-herpetic neuralgia[J].Clin Drug Investig 2009,29:393 -408.
[55]Baron R,Mayoral V,Leijon G,et al.5% lidocaine medicated plaster versus pregabalin in post-herpetic neuralgia and diabetic polyneuropathy:an open-label,non-inferiority two-stage RCT study[J].Curr Med Res Opin,2009,27:1663 -1676.
[56]Hans G,Sabatowski R,Binder A,et al.Efficacy and tolerability of a 5% lidocaine medicated plaster for the topical treatment of postherpetic neuralgia:results of a long-term study[J].Curr Med Res Opin,2009,25:1295 -1305.
[57]Backonja M,Wallace MS,Blonsky ER,et al.NGX-4010,a high concentration capsaicin patch,for the treatment of postherpetic neuralgia:a randomised,double-blind study[J].Lancet Neurol,2009,7:1106 -1112.
[58]Shackelford S,Rauck R,Quessy S,et al.A randomized,doubleblind,placebo controlled trial of a selective COX2 inhibitor GW406381 in patients with postherpetic neuralgia[J].J Pain,2009,10:654 -660.
[59]Cruccu G,Truini A.Trigeminal neuralgia and orofacial pains.In:Pappagallo M,ed.The Neurological Basis of Pain[M].New York:McGraw Hill,2005:401 -414.
[60]Cruccu G,Sommer C,Anand P,et al.EFNS guidelines on neuropathic pain assessment:revised 2009[J].Eur J Neurol,2010,17:1010 -1018.
[61]Gronseth G,Cruccu G,Alksne J,et al.Practice parameter:the diagnostic evaluation and treatment of trigeminal neuralgia (an evidence-based review):report of the Quality Standards Subcommittee of the American Academy of Neurology,and the European Federation of Neurological Societies[J].Neurology,2008,71:1183 -1190.
[62]Cruccu G,Gronseth G,Alksne J,et al.AAN-EFNS guidelines on trigeminal neuralgia management[J].Eur J Neurol,2008,15:1013 -1028.
[63]He L,Wu B,Zhou M.Non-antiepileptic drugs for trigeminal neuralgia[J].Cochrane Database Syst Rev,2006,3:CD004029.
[64]Nurmikko T,Cruccu G.Botulinum toxin for trigeminal neuralgia[J].Eur J Neurol,2009,16:e104.
[65]Lemos L,Flores S,Oliveira P,et al.Gabapentin supplemented with ropivacaine block of trigger points improves pain control and quality of life in trigeminal neuralgia patients when compared with gabapentin alone[J].Clin J Pain,2008,24:64 -75.
[66]Klit H,Finnerup NB,Jensen TS.Central post-stroke pain:clinical characteristics,pathophysiology,and management[J].Lancet Neurol,2009,9:857 -868.
[67]Siddall PJ,Cousins MJ,Otte A,et al.Pregabalin in central neuropathic pain associated with spinal cord injury:a placebo-controlled trial[J].Neurology,2006,67:1792 -1800.
[68]Vranken JH,Dijkgraaf MG,Kruis MR,et al.Pregabalin in patients with central neuropathic pain:a randomized,doubleblind,placebocontrolled trial of a flexible-dose regimen[J].Pain,2008,136:150 -157.
[69]Rintala DH,Holmes SA,Courtade D,et al.Comparison of the effectiveness of amitriptyline and gabapentin on chronic neuropathic pain in persons with spinal cord injury[J].Arch Phys Med Rehab,2007,88:1547 -1560.
[70]Breuer B,Pappagallo M,Knotkova H,et al.A randomized,doubleblind,placebo-controlled,two-period,crossover,pilot trial of lamotrigine in patients with central pain due to multiple sclerosis[J].Clin Ther,2007,29:2022 -2030.
[71]Finnerup NB,Grydehoj J,Bong J,et al.Levetiracetam in spinal cord injury pain:a randomized controlled trial[J].Spinal cord,2009,47:861 -867.
[72]Rowbotham MC,Twilling L,Davies PS,et al.Oral opioid therapy for chronic peripheral and central neuropathic pain[J].New Engl J Med,2003,348:1223 -1232.
[73]Norrbrink C,Lundeberg T.Tramadol in neuropathic pain after spinal cord injury:a randomized double blind placebo-controlled trial[J].Clin J Pain,2009,25:177 -184.
[74]Rog DJ,Nurmikko TJ,Young CA.Oromucosal delta9-tetrahydro cannabinol cannabidiol for neuropathic pain associated with multiple sclerosis:an uncontrolled,openlabel,2-year extension trial[J].Clin Ther,2007,29:2068 -2079.
[75]Vranken JH,Dijkgraaf MG,Kruis MR,et al.Iontophoretic administration of S(+)-ketamine in patients with intractable central pain:a placebo-controlled trial[J].Pain,2005,118:224 -231.
[76]Arbaiza D,Vidal O.Tramadol in the treatment of neuropathic cancer pain:a double-blind,placebo-controlled study[J].Clin Drug Investig,2007,27:75 -83.
[77]Hardy JR,Rees EA,Gwilliam B,et al.A phase II study to establish the efficacy and toxicity of sodium valproate in patients with cancerrelated neuropathic pain[J].J Pain Symptom Manage,2001,21:204 -209.
[78]Gordh TE,Stubhaug A,Jensen TS,et al.Gabapentin in traumatic nerve injury pain:a randomized,double-blind,placebo-controlled,cross-over,multi-center study[J].Pain,2008,138:255 -266.
[79]Ranoux D,Attal N,Morain F,et al.Botulinum toxin a induces direct analgesic effects in neuropathic pain:a double blind placebo controlled study[J].Ann Neurol,2008,64:274 -283.
[80]Vilholm OJ,Cold S,Rasmussen L,et al.Effect of levetiracetam on the postmastectomy pain syndrome[J].Eur J Neurol,2008,15:851 -857.
[81]Khoromi S,Patsalides A,Parada S,et al.Topiramate in chronic lumbar radicular pain[J].J Pain,2005,6:829 -836.
[82]Khoromi S,Cui L,Nackers L,et al.Morphine,nortriptyline and their combination vs.placebo in patients with chronic lumbar root pain[J].Pain,2007,130:66 -75.
[83]pdf.clinicalstudyresults.org/documents/company-study 4268.
[84]Wu CL,Agarwal S,Tella PK,et al.Morphine versus mexiletine for treatment of postamputation pain:a randomized,placebo-controlled,crossover trial[J].Anesthesiology,2008,109:289 -296.
[85]Wilder-Smith CH,Hill LT,Laurent S.Postamputation pain and sensory changes in treatment-naive patients:characteristics and responses to treatment with tramadol,amitriptyline,and placebo[J].Anesthesiology,2005,103:619 -628.
[86]Karst M,Salim K,Burstein S,et al.Analgesic effect of the synthetic cannabinoid CT-3 on chronic neuropathic pain:a randomized controlled trial[J].JAMA,2003,290:1757 -1762.
[87]Nurmikko TJ,Serpell MG,Hoggart B,et al.Sativex successfully treats neuropathic pain characterised by allodynia:a randomised,double-blind,placebo-controlled clinical trial[J].Pain,2007,133:210 -220.
[88]Yucel A,Ozyalcin S,Koknel Talu G,et al.The effect of venlafaxine on ongoing and experimentally induced pain in neuropathic pain patients:a double blind,placebo controlled study[J].Eur J Pain,2005,9:407 -416.
[89]Frank B,Serpell MG,Hughes J,et al.Comparison of analgesic effects and patient tolerability of nabilone and dihydrocodeine for chronic neuropathic pain:randomised,crossover,double blind study[J].BMJ,2008,336:199 -201.
[90]Ho KY,Huh BK,White WD,et al.Topical amitriptyline versus lidocaine in the treatment of neuropathic pain[J].Clin J Pain,2008,24:51 -55.
[91]Silver M,Blum D,Grainger J.Double blind placebocontrolled trial of lamotrigine in combination with other medications for neuropathic pain[J].J Pain Symptom Manage,2007,34:446 -454.
[92]Yelland MJ,Poulos CJ,Pillans PI,et al.N-of-1 randomized trials to assess the efficacy of gabapentin for chronic neuropathic pain[J].Pain Med,2009,10:754 -761.
[93]Jensen MP,Friedman M,Bonzo D,et al.The validity of the neuropathic pain scale for assessing diabetic neuropathic pain in a clinical trial[J].Clin J Pain,2006,22:97 -103.
[94]Jensen MP,Chiang Y-K,Wu J.Assessment of pain quality in a clinical trial of gabapentin extended release for postherpetic neuralgia[J].Clin J Pain,2009,25:286 -292.
[95]Stacey BR,Barrett JA,Whalen E,et al.Pregabalin for postherpetic neuralgia:placebo-controlled trial of fixed and flexible dosing regimens on allodynia and time to onset of pain relief[J].J Pain,2008,9:1006 -1017.
[96]Edwards RR,Haythornthwaite JA,Tella P,et al.Basal heat pain thresholds predict opioid anal-gesia in patients with postherpetic neuralgia[J].Anesthesiology,2006,104:1243 -1248.
[97]Wasner G,Kleinert A,Binder A,et al.Postherpetic neuralgia:topical lidocaine is effective in nociceptor deprived skin[J].J Neurol,2005,252:677 -686.
[98]Jensen MP,Chodroff MJ,Dworkin RH.The impact of neuropathic pain on health-related quality of life:review and implications[J].Neurology,2007,68:1178 -1182.
[99]O'Connor AB.Neuropathic pain.Quality-of-life impact,costs and cost effectiveness of therapy[J].Pharmacoeconomics,2009,27:95 -112.
[100]Deshpande MA,Holden RR,Gilron I.The impact of therapy on quality of life and mood in neuropathic pain:what is the effect of pain reduction[J].Anesth Analg,2006,102:1473 -1479.
[101]Armstrong DG,Chappell AS,Le TK,et al.Duloxetine for the management of diabetic peripheral neuropathic pain:evaluation of functional outcomes[J].Pain Med,2007,8:410 -418.
[102]Otto M,Bach FW,Jensen TS,et al.Health-related quality of life and its predictive role for analgesic effect in patients with painful polyneuropathy[J].Eur J Pain,2007,11:572 -578.
[103]Baron R,Tölle TR,Gockel U,et al.A cross-sectional cohort survey in 2100 patients with painful diabetic neuropathy and postherpetic neuralgia:differences in demographic data and sensory symptoms[J].Pain,2009,146:34 -40.
[104]Cruccu G,Truini A.Sensory profiles:a new strategy for selecting patients in treatment trials for neuropathic pain[J].Pain,2009,146:5 -6.
[105]Attal N,Fermanian C,Fermanian J,et al.Neuropathic pain:are there distinct subtypes depending on the aetiology or anatomical lesion[J].Pain,2008,138:343 -353.