急诊结肠镜在急性下消化道出血诊断及治疗中的应用价值
2012-09-14赵晓军王海红李爱琴余东亮盛剑秋
赵晓军,李 娜,王海红,李爱琴,王 昕,谢 惠,余东亮,盛剑秋
北京军区总医院消化内科,北京 100700
急诊结肠镜在急性下消化道出血诊断及治疗中的应用价值
赵晓军,李 娜,王海红,李爱琴,王 昕,谢 惠,余东亮,盛剑秋
北京军区总医院消化内科,北京 100700
目的 探讨急诊结肠镜对急性下消化道出血的诊断价值。方法 对293例接受急诊结肠镜检查的急性下消化道出血患者临床资料进行分析,比较急诊结肠镜组与常规结肠镜组在平均住院日及输血量之间的差异。结果 急诊结肠镜组检查成功率90.1%,总体诊断率64.5%。急诊结肠镜组平均住院天数6.9 d,常规结肠镜组7.8 d,急诊结肠镜组平均输血量275 mL压积红细胞,常规结肠镜组478 mL。结论 急诊结肠镜对活动性出血可采取内镜下止血,为急诊外科手术治疗提供可靠依据,同时可减少急性下消化道出血患者的住院天数及平均输血量。
急性下消化道出血;急诊结肠镜;诊断;治疗
结肠镜检查是急性下消化道出血诊断的首选方式,但目前尚缺乏急性下消化道出血危险评估标准,对于急诊结肠镜检查的时机和适应证等尚存争议[1-2]。本研究对我院10年来行急诊结肠镜的急性下消化道出血患者的临床资料进行分析,以探讨急诊结肠镜对急性下消化道出血的诊断及治疗价值。
1 资料及方法
1.1 临床资料 2002年1月-2012年1月在我院急诊就诊及住院共598例急性下消化道出血患者行结肠镜检查(排除息肉切除术后出血者),293例患者在入院或就诊后12~24 h内行急诊结肠镜检查,305例行常规结肠镜检查。急诊结肠镜组男187例,女106例,年龄21~79岁,平均年龄(56.8±11.4)岁;常规结肠镜组男204例,女101例,年龄26~87岁,平均年龄(60.8±6.3)岁。急诊结肠镜组与常规结肠镜组平均年龄及性别比例无显著差异(P>0.05)。
1.2 方法 急诊结肠镜组150例口服泄剂清肠(口服硫酸镁或舒泰清),69例清洁灌肠(温水或生理盐水),74例未行肠道准备。常规结肠镜组患者常规口服泄剂清肠(口服硫酸镁或舒泰清)。
2 结果
2.1 全结肠镜检查完成情况 结肠镜检查以到达回盲部或回肠末端为完成全结肠检查。急诊结肠镜组中清肠组182例患者完成全结肠(包括回肠末端)检查;未清肠组56例患者完成全结肠(回肠末端)检查。清肠组与未清肠组完成全结肠检查率无显著差异(清肠组83.1%,未清肠组 75.7%,P=0.589,见表 1)。常规结肠镜组均完成全结肠镜检查。
2.2 结肠镜检查诊断率
2.2.1 急诊结肠镜组诊断率及处理情况:189例首次急诊结肠镜检查发现病变部位,诊断率64.5%(189/293)。36例二次结肠镜检查(清肠后)发现病变部位(36/293,12.3%),43 例未发现明确出血部位(43/293,14.7%)。189例首次急诊结肠镜检查共发现出血病灶196处,其中活跃性出血病灶97处。88处活跃性出血病灶行结肠镜下止血治疗(88/97,90.7%),包括病变部位喷洒止血药物、钛夹止血、黏膜下注射等方法,83处病灶(83/88,94.3%)止血成功,患者治愈出院,5例内镜下止血失败,3例外科手术,1例术后多脏器功能衰竭死亡,2例DSA止血。6例小肠活跃性出血分别行紧急DSA及急诊经肛小肠镜检查,3例经DSA止血成功,另3例小肠镜发现活跃性出血病变急诊外科手术。
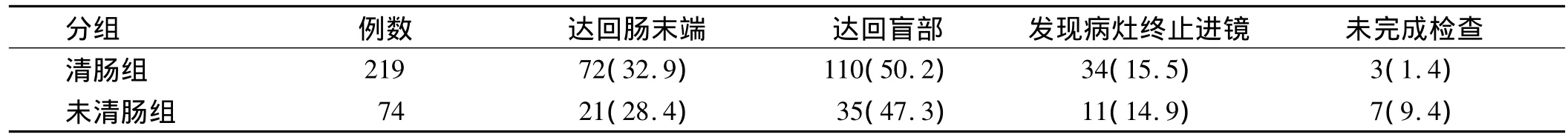
表1 急诊结肠镜组全结肠镜检查完成情况[例数(%)]Tab 1 The data of accomplishment of urgent colonoscopic interventions[n(%)]
2.2.2 常规结肠镜组诊断率:常规结肠镜组225例首次检查发现病灶,总体诊断率73.8%(225/305),其中活跃性出血病灶23处(23/225,10.2%)。
2.3 平均住院天数及输血量 急诊结肠镜组平均住院天数6.9 d,常规结肠镜组平均住院天数7.8 d。急诊结肠镜组平均输血量275 mL压积红细胞/例,常规结肠镜组平均输血量478 mL压积红细胞/例。
3 讨论
急性下消化道出血(ALGB)是消化科常见急症,其与患者死亡率、医疗花费、住院时间有明显关系,因此有效的评估及治疗非常重要[3-5]。既往研究表明,结肠镜对ALGB的诊断率为74% ~100%,治疗率为8% ~ 37%[6-12]。Ríos 等[13]的研究显示,同常规结肠镜检查比较急诊结肠镜可显著提高消化道出血的诊断率。但最近Laine等[14]的研究显示急诊结肠镜与常规结肠镜的诊断率无明显差异。本组病例急诊结肠镜检查总体诊断率64.5%,常规结肠镜组诊断率70.4%,两组比较诊断率无显著差异,但急诊结肠镜组活跃性出血病灶数量与常规肠镜组相比差异显著,且90.7%活跃性出血病灶内镜下止血,止血成功率94.3%,提示急诊肠镜可早期明确伴活跃性出血ALGB的出血部位并进行内镜下止血,缩短诊断时间,减少患者输血量及平均住院日。
ALGB常见病因国外资料按其发病率,占前4位的分别为:结肠憩室、血管畸形、结直肠恶性肿瘤和缺血性肠病。本组资料显示急诊结肠镜组ALGB病因前4位的是:结肠溃疡性病变、血管畸形、结肠肿瘤、缺血性肠病等,似与总体疾病构成略不同,考虑与本组患者中活跃性出血比例较高,且溃疡性病变及血管性病变多合并活动性出血有关。本组资料提示结肠溃疡及血管畸形等病变多合并活跃性出血,内镜下可实施止血夹、喷洒药物等方法止血,止血效果可靠。
综合既往临床资料以及本组病例资料,考虑急诊结肠镜对于ALGB的诊断及治疗意义在于以下几方面:①判断出血部位位于结肠或下段小肠;② 早期发现活跃性出血病变并内镜下治疗,减少患者输血量,如止血失败可为进一步检查治疗如DSA止血及外科治疗提供依据。急诊结肠镜也存在一定局限性,如患者肠腔内积血及肠道清洁度较差,会增加进镜及观察病变的难度。文献报道在ALGB患者中未行肠道准备的结肠镜检查仅55% ~70%到达回盲部[15-17],本组资料显示,接受急诊结肠镜检查的清肠组与未清肠组总体完成检查情况无显著差异。我们的体会是大量下消化道出血者肠道内积存粪便较少,主要为鲜血及血块,检查者进镜时可根据黏膜皱襞走形判断进镜方向,根据患者肠道积血情况,初步判断出血部位,对可疑部位重点冲洗、观察,有利于提高结肠镜检查成功率及病变检出率。本组内镜检查医师均为有2 000~3 000例结肠镜检查经验的内镜医师,有经验的内镜医师可提高检查成功率,缩短检查时间,提高患者检查顺应性。
[1] Strate LL.Editorial:Urgent colonoscopy in lower GI bleeding:not so fast[J].2010,105(12):2643-2645.
[2] Jensen DM,Machicado GA,Jutabha R,et al.Urgent colonoscopy for the diagnosis and treatment of severe diverticular hemorrhage[J].N Engl J Med,2000,342(2):78-82.
[3] Lanas A,García-Rodríguez LA,Polo-Tomás M,et al.The changing face of hospitalisation due to gastrointestinal bleeding and perforation[J].Aliment Pharmacol Ther,2011,33(5):585-591.
[4] Ríos A,Montoya MJ,Rodríguez JM,et al.Acute lower gastrointestinal hemorrhages in geriatric patients[J].Dig Dis Sci,2005,50(5):898-904.
[5] Comay D,Marshall JK.Resource utilization for acute lower gastrointestinal hemorrhage:the Ontario GI bleed study[J].Can J Gastroenterol,2002,16(10):677-682.
[6] Angtuaco TL,Reddy SK,Drapkin S,et al.The utility of urgent colonoscopy in the evaluation of acute lower gastrointestinal tract bleeding:a 2-year experience from a single center[J].Am J Gastroenterol,2001,96(6):1782-1785.
[7] Jensen DM,Machicado GA,Jutabha R,et al.Urgent colonoscopy for the diagnosis and treatment of severe diverticular hemorrhage[J].N Engl J Med,2000,342(2):78-82.
[8] Green BT,Rockey DC,Portwood G,et al.Urgent colonoscopy for evaluation and management of acute lower gastrointestinal hemorrhage:a randomized controlled trial[J].Am J Gastroenterol,2005,100(11):2395-2402.
[9] Bloomfeld RS,Rockey DC,Shetzline MA.Endoscopic therapy of acute diverticular hemorrhage [J].Am J Gastroenterol,2001,96(8):2367-2372.
[10] Richter JM,Christensen MR,Kaplan LM,et al.Effectiveness of current technology in the diagnosis and management of lower gastrointestinal hemorrhage[J].Gastrointest Endosc,1995,41(2):93-98.
[11] Colacchio TA,Forde KA,Patsos TJ,et al.Impact of modern diagnosticMethodson the management of active rectal bleeding.Ten year experience[J].Am J Surg,1982,143(5):607-610.
[12] Al Qahtani AR,Satin R,Stern J,et al.Investigative modalities for massive lower gastrointestinal bleeding[J].World J Surg,2002,26(5):620-625.
[13] Ríos A,Montoya MJ,Rodríguez JM,et al.Severe acute lower gastrointestinal bleeding:risk factors for morbidity and mortality[J].Langenbecks Arch Surg,2007,392(2):165-71.
[14] Laine L,Shah A.Randomized trial of urgent vs.elective colonoscopy in patients hospitalized with lower GI bleeding[J].Am J Gastroenterol,2010,105(12):2636-2641.
[15] Chaudhry V,Hyser MJ,Gracias VH,et al.Colonoscopy:the initial test for acute lower gastrointestinal bleeding[J].Am Surg,1998,64(8):723-728.
[16] Tada M,Shimizu S,Kawai K.Emergency colonoscopy for the diagnosis of lower intestinal bleeding[J].Gastroenterol Jpn,1991,26(3):121-124.
[17] Ohyama T,Sakurai Y,Ito M,et al.Analysis of urgent colonoscopy for lower gastrointestinal tract bleeding[J].Digestion,2000,61(3):189-192.
Value of urgent colonoscopy in acute lower gastrointestinal bleeding
ZHAO Xiaojun,LI Na,WANG Haihong,LI Aiqin,WANG Xin,XIE Hui,YU Dongliang,SHENG Jianqiu
Department of Gastroenterology,the Military General Hospital of Beijing PLA,Beijing 100700,China
ObjectiveTo explore the value of urgent colonoscopy(<12 h from admission)in acute lower gastrointestinal bleeding(ALGB).MethodsThe data of 293 patients with ALGB undergoing urgent colonoscopy were analyzed.Average length of hospital stay and volume of blood transfusion were compared between urgent colonoscopy and routine colonoscopy groups.ResultsThe success rate of accomplishment of urgent colonoscopy was 90.1%,and the diagnostic rate was 64.5%.The average length of stay was 6.9 days in the urgent colonoscopy group and 7.8 days in the routine colonoscopy group.The average volume of blood transfusion was 275 mL in the urgent colonoscopy group and 478 mL in the elective colonoscopy group.ConclusionIt is suggested that the urgent colonoscopy can provide therapeutic interventions and improve success rate of hemostasis.It can provide the reliable evidence for the surgery and decrease hospital length of stay and the average volume of blood transfusion.
Acute lower gastrointestinal bleeding;Urgent colonoscopy;Diagnosis;Treatment
R574
A
1006-5709(2012)08-0730-03
2012-07-03
10.3969/j.issn.1006-5709.2012.08.013
盛剑秋,E-mail:jianqiu@263.net