A new scoring system for assessment of liver function after successful hepatectomy in patients with hepatocellular carcinoma
2011-06-11
Chengdu,China
Introduction
Hepatocellular carcinoma (HCC) is a common malignancy worldwide.Surgery,including hepatectomy and liver transplantation,is most efficacious for the treatment of patients with HCC.[1,2]Because of insufficient donation,however,liver resection is widely accepted as the first treatment for localized HCC after careful patient selection,even in patients with chronic liver disease.[3,4]With the advances in surgical techniques and perioperative management,in-hospital mortality and morbidity have greatly improved,[5]but the mortality rate still ranges from 5% to 8%.[6]In cases of liver resection,postoperative liver failure is the major cause of early postoperative death.[7,8]
Despite numerous studies,it is not yet possible to predict postoperative liver failure and the safe limit for hepatectomy.Thus a reevaluation of the factors linked to postoperative liver failure is necessary.Indocyanine green (ICG) is a water-soluble,nontoxic tricarbocyanine dye that is extracted exclusively by hepatic parenchymal cells without enterohepatic circulation and excreted entirely into the bile.[9]The ICG clearance test has been used for many years to measure hepatic blood flow and to more precisely assess liver functional reserve before hepatectomy.[10-12]On the other hand,some authors prefer the standard remnant liver volume (SRLV) to prevent postoperative liver failure in cirrhotic patients.This retrospective study was focused on the ICG test,the SRLV,and a score combining both factors to determine the safe limit for liver resection.
Methods
Patients
From March 2007 to June 2010,a total of 86 patients who had undergone liver resection for HCC at our department were included in this study.There were 73 men and 13 women,with a mean age of 50.9±12.3 years (range 29-74 years).All patients underwent blood tests and conventional simple liver function tests to investigate the liver impairment before resection.The surgical modalities inluded trisectionectomy (right in 21,left in 8) for 29 patients,and bisegmentectomy(right posterior sectionectomy in 17,right anterior sectionectomy in 9,and left lateral sectionectomy in 14)for 40,and partial resection for 17.A total of 67 patients(77.9%) were cirrhotic.Blood tests and conventional simple liver function tests were performed during days 1,3,and 7 after resection.Postoperative liver dysfunction was defined as a total bilirubin (TB) >85.5 μmol/L for 7 days after hepatectomy.[13]The clinical course of the patients was followed up for a minimum of 1 month after hepatectomy.
ICG test
All the patients in this study had a preoperative ICG test which consisted of injecting 0.5 mg/kg of ICG into a peripheral vein.During the first 5-10 minutes after injection,blood ICG concentrations were monitored at every pulse interval via pulse spectrophotometry.The KICGvalue (clearance rate constant) and R15 (retention rate at 15 minutes) were then calculated automatically from the time course of the blood ICG concentration.[14]
Liver volume
All patients underwent a CT scan to evaluate total liver volume (TLV) before surgery.The displacement method,on the other hand,can be used to accurately obtain the resected liver volume in operation.The remnant liver volume (RLV) was calculated by TLV minus the resected liver volume.Then the standard remnant liver volume (SRLV) was calculated by the equation:SRLV (mL/m2)=RLV÷body surface area (BSA,m2).BSA was calculated using body weight (BW) and body height (BH) (DuBois formula),BSA=BW(kg)0.425×BH(cm)0.725×0.007184.[15]
Statistical analysis
Continuous data are expressed as mean±standard deviation.The data were analyzed by Scheffe's test,the Chi-square test and logistic regression.The statistical analysis was performed with Statistical Package for the Social Sciences (version 13.0).For the determination of the receiver operating characteristic (ROC) curve,we used ROC curve analysis software (MedCale,version 7.5.0.0).P values <0.05 were considered statistically significant.
Results
Patients were classified into two groups according to the levels of TB after hepatectomy.Sixty-nine patients (80.23%) without TB >85.5 μmol/L for 7 days after hepatectomy had good clinical outcomes(group I),but 17 recipients (19.77%) who experienced postoperative liver dysfunction (with TB >85.5 μmol/L for 7 days after hepatectomy) needed prolonged intensive management,and showed poor clinical courses (group II).Group II was further divided into two subgroups:subgroup a,with 14 patients,all of whom recovered from postoperative liver dysfunction,and subgroup b,with 3 patients all of whom died of liver failure.There were no differences in age,Child-Pugh score,MELD score,prothrombin time,international normalized ratio,TB,albumin,alanine aminotransferase,aspartateaminotransferase, alkaline phosphatase, gammaglutamyl transferase,creatinine and TLV between the two groups (P>0.05).But the ICG test variables (KICGand R15) showed significant differences between the two groups.The SRLV in groups I and II was 542±89 mL/m2and 394±80 mL/m2,respectively,and the difference was statistically significant (Table 1).

Table 1.Comparison of the variables in the two groups (mean±SD)

Table 2.The covariates included in the model by logistic regression
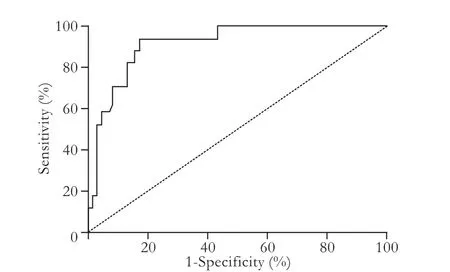
Fig.1.By ROC analysis,the sensitivity and specificity of an LFC value ≤13.01 were 94.1% and 82.6%,respectively,for predicting postoperative liver dysfunction (area under the ROC curve=0.916;standard error=0.030; 95% confidence interval=0.836 to 0.965).
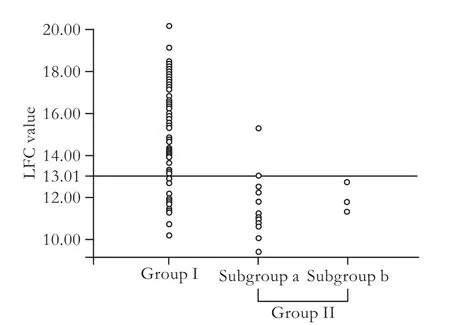
Fig.2.On the left,the majority of patients have a LFC value >13.01,and on the middle,the majority of patients have a LFC value ≤13.01,showing postoperative liver dysfunction,and on the right,all patients have a LFC value ≤13.01 and all of them died of postoperative liver failure.A LFC value ≤13.01 can predict postoperative liver dysfunction.
A logistic regression model was used to identify the predictors of liver dysfunction.The covariates included in the model were the preoperative KICGvalue and SRLV (Table 2).Then we defined the liver function compensatory (LFC) value which is calculated by thepreoperative KICGvalue×22.487+SRLV×0.020.The critical point of the LFC value to predict postoperative liver dysfunction was 13.01 according to ROC analysis(Figs.1 and 2).The sensitivity and specificity were 94.1%and 82.6%.Then we divided patients into two groups according to this standard.A total of 28 patients had an LFC ≤13.01,16 (57.1%) of whom had postoperative liver dysfunction.In contrast,of 58 patients with an LFC >13.01,only one (1.7%) had postoperative liver dysfunction.This difference was statistically significant(Table 3).The rate of postoperative liver dysfunction was greater when LFC ≤13.01.
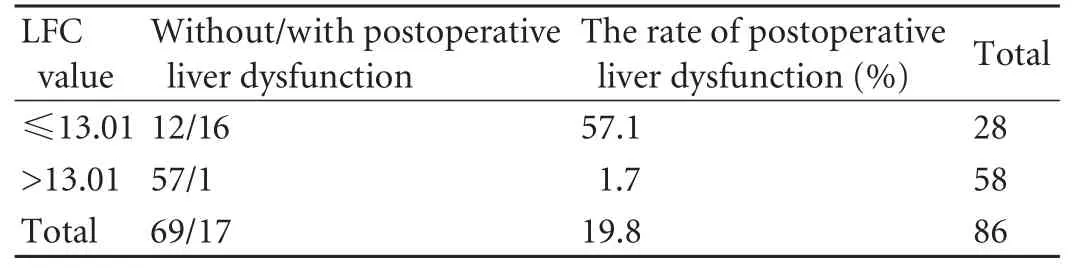
Table 3.The differences of the rate of postoperative liver dysfunction between both groups divided by LFC value (P=0.000)
Discussion
The liver has a substantial regenerative ability and an immense reserve capacity.Seventy-five percent of a healthy liver can be resected safely.With improvement in operative and anesthetic techniques,and pre- and postoperative management,the mortality of patients after liver resection has decreased.However,the incidence of postoperative liver failure is still high,particularly that of patients with HCC associated with liver cirrhosis.These patients bear a high risk of developing liver insufficiency,since liver function and regeneration are impaired.Therefore an objective method to determine the safe limit of liver resection based on the severity of hepatic injury would be valuable.
ICG is a synthetic dye that is eliminated by the liver without extrahepatic metabolism and excretion,and its blood clearance has been applied to determine the operative risk before hepatectomy.[16]The rate of elimination of ICG from the blood is delayed when the effective hepatic blood flow is lowered or the dye uptake of hepatocytes is reduced as a result of cirrhosis or other diseases.[17-19]Studies[20,21]of liver function before hepatectomy by the ICG clearance test have suggested a relationship between the preoperative test results and the postoperative outcome.Hence ICG is an ideal dye to re flect hepatic reserve.[22]
On the other hand,liver volume can also re flect hepatic reserve,which can be used to assess the operative risk before hepatectomy and to guide the ideal treatment.[23,24]The remnant liver volume is closely correlated with liver dysfunction or even liver failure after hepatectomy.[17]Shirabe reported that SRLV is a vital factor in liver failure after hepatectomy,and the rate of liver failure of patients with SRLV <250 mL/m2is 38% in contrast to patients with SRLV >250 mL/m2whose rate of liver failure is 0%.[25]
The causes of liver failure are complex because of broad differences in liver function,tumor size and location and operative procedures for each patient; thus no single parameter provides sufficient data for a safe limit of hepatectomy.In this study,we found that the ICG test indices (KICG) and SRLV showed significant differences between the two groups.The ICG test re flects the function of hepatic parenchymal cells and the SRLV re flects the quantity of hepatic parenchymal cells remaining.Therefore we established a prediction score using a combination of the preoperative KICGvalue×22.487+SRLV×0.020 (LFC value) to determine the extent of liver resection.We calculated that the critical point of LFC value was 13.01 according to ROC analysis.Then we divided the groups according to the critical point and found distinctive differences in liver dysfunction posthepatectomy.There was a higher rate of liver dysfunction when the LFC value was ≤13.01.
Every patient can have a preoperative ICG test to obtain the KICGvalue.Then the critical LFC value for predicting good or bad outcomes is divided by the KICGvalue to calculate the absolute borderline value of SRLV.At the same time,a patient may undergo a CT scan to evaluate TLV and estimated resected liver volume to calculate estimated SRLV before surgery.If the estimated SRLV is higher than the absolute borderline value,hepatectomy is relatively safe and it can be predicted that the patient has a low risk of postoperative liver dysfunction.If the estimated SRLV is lower than the absolute borderline value,there is a greater risk of postoperative liver dysfunction in patients; they should get early related and appropriate postoperative treatments or adopt other treatments such as liver transplantation,portal vein embolization to improve remnant liver volume,transcatheter arterial chemoembolization,or radiofrequency ablation.After using this method in our department,the rate of postoperative liver dysfunction has decreased by 12%from 20% to 8%.
In conclusion,though the causes of liver failure are complex,the LFC value appears to be a good predictor of postoperative liver dysfunction.Careful patient selection based on the ICG test and volumetric analysis in such major hepatectomy cases should help to prevent the occurrence of postoperative liver dysfunction.
Funding:None.
Ethical approval:Not needed.
Contributors:DZG proposed the study.DZG and LB wrote the first draft and analyzed the data.All authors contributed to the design and interpretation of the study and to further drafts.LB is the guarantor.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Schwartz M,Roayaie S,Konstadoulakis M.Strategies for the management of hepatocellular carcinoma.Nat Clin Pract Oncol 2007;4:424-432.
2 Llovet JM,Schwartz M,Mazzaferro V.Resection and liver transplantation for hepatocellular carcinoma.Semin Liver Dis 2005;25:181-200.
3 Shimada M,Matsumata T,Akazawa K,Kamakura T,Itasaka H,Sugimachi K,et al.Estimation of risk of major complications after hepatic resection.Am J Surg 1994;167:399-403.
4 Fan ST,Lai EC,Lo CM,Ng IO,Wong J.Hospital mortality of major hepatectomy for hepatocellular carcinoma associated with cirrhosis.Arch Surg 1995;130:198-203.
5 Ziparo V,Balducci G,Lucandri G,Mercantini P,Di Giacomo G,Fernandes E.Indications and results of resection for hepatocellular carcinoma.Eur J Surg Oncol 2002;28:723-728.
6 Belghiti J,Regimbeau JM,Durand F,Kianmanesh AR,Dondero F,Terris B,et al.Resection of hepatocellular carcinoma:a European experience on 328 cases.Hepatogastroenterology 2002;49:41-46.
7 Shimada M,Takenaka K,Fujiwara Y,Gion T,Shirabe K,Yanaga K,et al.Risk factors linked to postoperative morbidity in patients with hepatocellular carcinoma.Br J Surg 1998;85:195-198.
8 Belghiti J,Hiramatsu K,Benoist S,Massault P,Sauvanet A,Farges O.Seven hundred forty-seven hepatectomies in the 1990s:an update to evaluate the actual risk of liver resection.J Am Coll Surg 2000;191:38-46.
9 Wheeler HO,Cranston WI,Meltzer JI.Hepatic uptake and biliary excretion of indocyanine green in the dog.Proc Soc Exp Biol Med 1958;99:11-14.
10 Okochi O,Kaneko T,Sugimoto H,Inoue S,Takeda S,Nakao A.ICG pulse spectrophotometry for perioperative liver function in hepatectomy.J Surg Res 2002;103:109-113.
11 Sugimoto H,Okochi O,Hirota M,Kanazumi N,Nomoto S,Inoue S,et al.Early detection of liver failure after hepatectomy by indocyanine green elimination rate measured by pulse dye-densitometry.J Hepatobiliary Pancreat Surg 2006;13:543-548.
12 Ohwada S,Kawate S,Hamada K,Yamada T,Sunose Y,Tsutsumi H,et al.Perioperative real-time monitoring of indocyanine green clearance by pulse spectrophotometry predicts remnant liver functional reserve in resection of hepatocellular carcinoma.Br J Surg 2006;93:339-346.
13 Fujii Y,Shimada H,Endo I,Morioka D,Nagano Y,Miura Y,et al.Risk factors of posthepatectomy liver failure after portal vein embolization.J Hepatobiliary Pancreat Surg 2003;10:226-232.
14 Sakka SG,Meier-Hellmann A.Non-invasive liver function monitoring by indocyanine green plasma disappearance rate in critically ill patients.International J Intensive Care 2002:66-72.
15 Du Bois D,Du Bois EF.A formula to estimate the approximate surface area if height and weight be known.1916.Nutrition 1989;5:303-313.
16 Mullin EJ,Metcalfe MS,Maddern GJ.How much liver resection is too much? Am J Surg 2005;190:87-97.
17 Schindl MJ,Redhead DN,Fearon KC,Garden OJ,Wigmore SJ;Edinburgh Liver Surgery and Transplantation Experimental Research Group (eLISTER).The value of residual liver volume as a predictor of hepatic dysfunction and infection after major liver resection.Gut 2005;54:289-296.
18 Lam CM,Fan ST,Lo CM,Wong J.Major hepatectomy for hepatocellular carcinoma in patients with an unsatisfactory indocyanine green clearance test.Br J Surg 1999;86:1012-1017.
19 Wakabayashi H,Ishimura K,Izuishi K,Karasawa Y,Maeta H.Evaluation of liver function for hepatic resection for hepatocellular carcinoma in the liver with damaged parenchyma.J Surg Res 2004;116:248-252.
20 Kusaka K,Harihara Y,Torzilli G,Kubota K,Takayama T,Makuuchi M,et al.Objective evaluation of liver consistencyto estimate hepaticfibrosis and functional reserve for hepatectomy.J Am Coll Surg 2000;191:47-53.
21 Poon RT,Fan ST.Hepatectomy for hepatocellular carcinoma:patient selection and postoperative outcome.Liver Transpl 2004;10:S39-45.
22 Faybik P,Hetz H.Plasma disappearance rate of indocyanine green in liver dysfunction.Transplant Proc 2006;38:801-802.
23 Li YM,Lv F,Ji H,Bai ZL,Lei TJ.A study on the correlation between hepatic volume and liver functional reserve.Zhonghua Pu Tong Wai Ke Za Zhi 2003;18:79-81.
24 Schiano TD,Bodian C,Schwartz ME,Glajchen N,Min AD.Accuracy and significance of computed tomographic scan assessment of hepatic volume in patients undergoing liver transplantation.Transplantation 2000;69:545-550.
25 Shirabe K,Shimada M,Gion T,Hasegawa H,Takenaka K,Utsunomiya T,et al.Postoperative liver failure after major hepatic resection for hepatocellular carcinoma in the modern era with special reference to remnant liver volume.J Am Coll Surg 1999;188:304-309.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Predictors of patient survival following living donor liver transplantation
- Hepatocellular carcinoma HepG2 cell apoptosis and caspase-8 and Bcl-2 expression induced by injectable seed extract of Coix lacryma-jobi
- Relationship between alcohol consumption and clinical manifestation of patients with fatty liver:a single-center study
- Oncofetal antigen glypican-3 as a promising early diagnostic marker for hepatocellular carcinoma
- Necessity and indications of invasive treatment for Budd-Chiari syndrome
- Evaluation of hepatitis B viral replication and proteomic analysis of HepG2.2.15 cell line after knockdown of HBx
