Necessity and indications of invasive treatment for Budd-Chiari syndrome
2011-06-11
Zhengzhou,China
Introduction
Budd-Chiari syndrome (B-CS) is caused by obstruction of the main hepatic veins (MHVs)and/or inferior vena cava (IVC).In Western countries,its spontaneous mortality was reported to approach 70% at 1 year and 90% at 3 years.[1]Therefore,early treatment was instituted as soon as the diagnosis was established in the past decades.[2]Compared to the administration of routine anticoagulation,surgical shunting and bypass procedures have long been used.[3]However,clinical data failed to show a favorable perioperation mortality and long-term outcomes.[4-6]
Blockage of two or more major hepatic veins increases the sinusoidal pressure and reduces sinusoidal blood flow,which leads to the development offibrosis,cirrhosis and the formation of intrahepatic or subcapsular venous collaterals during the course of this disease.[7-9]This collateral system can improve liver function and make this disease silent and asymptomatic for many years,demonstrating that intra- and extra-hepatic collaterals are of great clinical importance in guiding the treatment of B-CS.[10,11]Nonetheless,clinical usage of collateral circulation is just diagnostic and no studies have included these characteristics in the management strategy.The indications,benefits,and clinical impact of the collateral system in the management of B-CS remain unclear and only limited attempts have been made to adjust the comparisons between procedures for the baseline severity of the disease.This prompted us to reconsider treatment indications for the management of B-CS which takes collateral compensation into account.
Treatment of B-CS generally follows a least invasive to a most invasive strategy.[12]According to this principle,we hypothesized that the patients with sufficient collaterals have good compensation for clinical manifestations and these patients might not need invasive treatment.
Methods
Patients
From March 2004 to January 2010,29 out of 1207 consecutive adult patients with B-CS treated at our unit were enrolled into this study.The criteria for inclusion were (1) diagnosis of primary B-CS with IVC and MHV obstruction without evidence of other liver diseases (viral,autoimmune,biliary,or alcoholic); (2)patent portal veins and no malignant tumor; (3) arrest of acute variceal hemorrhage either spontaneously or by medication; (4) absence of life-threatening comorbidities and other chronic diseases (i.e.,tumors,diabetes or cardiovascular and respiratory disease); and(5) willingness to return for regular follow-up.
All of the patients (12 women and 17 men; median age 33 years,range 21-63 years) were Chinese and their main characteristics were typical of primary B-CS.According to the characteristics and treatment strategy,the patients were divided into two groups:18 patients underwent radiological intervention (group A),the other 11 had no invasive treatment (group B).At the time of diagnosis,the disease course and sex ratio were not significantly different between the two groups.In group A,ascites was present in 3 patients and bleeding from esophageal varices occurred in 1 before treatment.All the patients in group B underwent gastric endoscopy and/or double-contrast barium examination of the upper gastrointestinal tract.The detailed data of the patients in groups A and B are shown in Tables 1 and 2.
This clinical protocol was approved by the Ethics Committee at our institution and informed written consent was obtained from patients or their relatives before inclusion.
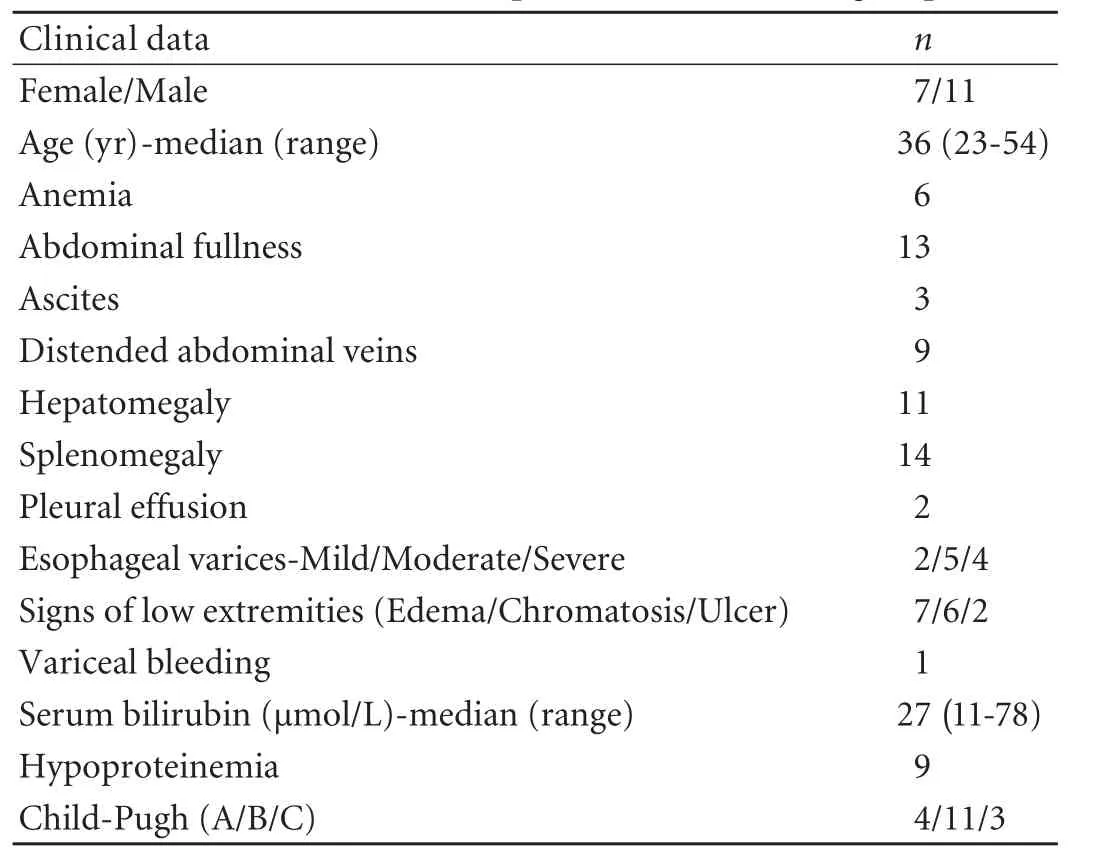
Table 1.Clinical data of 18 patients with B-CS in group A
Therapeutic strategy
After diagnosis of B-CS,clinical data on collateral circulation,manifestations and biochemical tests were comprehensively evaluated.The treatment indications and feasibility were determined based on comprehensive assessment of these data.
The therapeutic strategy was as follows:Invasive management was performed in patients of group A or group B with deterioration in the course of follow-up.In these patients,the indications for invasive treatment were obvious clinical presentation and/or biochemical abnormality.After the treatment,these patients were subjected to anticoagulation treatment with low molecularweight heparin or warfarin targeting an international normalized ratio of 2 to 3,and then the anticoagulation was substituted by aspirin within a couple of weeks when the patients were discharged and went into follow-up.
No invasive treatment was performed because of the good condition of the patients in group B.B-CS was considered asymptomatic when there was no evidence of unusual abdominal pain,jaundice,ascites,portal hypertension-related bleeding,or encephalopathy,and serum transaminase levels were persistently below twice the upper limit of the normal value.[13,14]Liver function of most of these patients was Child-Pugh A.In addition,very few patients in group B were given medical treatment because of mild symptoms.
Imaging analysis and radiological angioplasty
Doppler ultrasound and three-dimensional computed tomographic angiography were performed and the presence of intra- and extrahepatic collaterals was assessed before treatment.IVC angiography was carriedout in all the patients.Balloon angioplasty of the IVC and/or hepatic vein with or without stenting was performed for group A.At the same time,when possible,the mean IVC pressure and free hepatic pressure (FHP)were measured in the supine position and during respiratory apnea to minimize the effects of positive pressure ventilation.

Table 2.Clinical data of 11 patients with B-CS in group B
Histological analysis
Two tissue samples were collected by liver biopsy from the right and left lobe,not only during invasive treatment but in the course of follow-up.The samples werefixed in 10% buffered formalin,sliced at 0.4-mm intervals in the transverse plane,and then HE stained.Thereafter the presence of ischemic necrosis was determined,andfibrosis was graded on a scale of 0 to 4.
Follow-up
Follow-up was initiated from the first invasive treatment or the determination of no invasive treatment.Follow-up evaluation was at least every 2 weeks for 1 month then monthly for 2 months,every 3 months for a year,and every 6 months thereafter.In this course,the clinical data of physical examination,biochemical tests and ultrasound studies of all the patients were collected.In some cases,catheterization with pressure measurement and angiographic studies were performed.In addition,liver biopsy was performed whenever it was feasible to help determine further considerations of treatment.
Statistical analysis
Data handling and analysis were performed with SPSS 13.0 (SPSS Inc.,Chicago,IL).Quantitative variables are expressed as mean±SD,or median and range.For single comparisons,normally distributed data were analyzed using unpaired,two-tailed t test.Results were considered statistically significant if P<0.05.
Results
Imaging characteristics
Gross liver changes were present in treated patients,characterized by hepatomegaly,or hypertrophy of segment I associated with variable atrophy.A mottled appearance was noted related to inhomogeneous perfusion of the liver.Images clearly depicted the pathologic classifications of the IVC and MHVs and there was no statistical difference between the two groups.
In most cases,intra- and extrahepatic collaterals were identified,especially in group B.In general,the untreated patients had much richer collaterals than those in treated patients.They were identified either by the typical "spider web" sign or by large connecting veins between the accessory and main hepatic veins (Fig.1A).Two forms of intrahepatic collaterals may develop:those that communicate with systemic veins via the subcapsular vessels and those that shunt blood from the occluded to the nonoccluded segments of the hepatic vein.Almost all the patients demonstrated extrahepatic collaterals to different extents.Among these collaterals,esophageal veins,left renal-hemiazygos pathway,vertebrolumbarazygos pathway and super-ficial collaterals of the abdominal wall were the most common pathways(Fig.1B-E).Renal-inferior phrenic-pericardiophrenic collaterals were infrequently displayed in some patients(Fig.1F).
Treatment
According to the pathologic classification and presentation,18 patients safely underwent IVC balloon angioplasty.Among them,4 also underwent hepatic vein angioplasty.In addition,two cases of long-length obstruction of the IVC underwent balloon angioplasty plus stenting simultaneously.
In group A,the IVC pressure and FHP were almost equal.Of these patients,the mean IVC pressure before and after treatment was statistically different (29.3±9.2 vs 15.1±4.6 mmHg,t=5.88,P<0.01).The mean IVC pressure was much lower in group B than in group A(12.9±2.4 vs 29.3±9.2 mmHg,t=5.77,P<0.01) but it was not significantly different from that of patients after radiological treatment (12.9±2.4 vs 15.1±4.6 mmHg,t=1.44,P>0.05).
Fewer and slight complications occurred after all the procedures performed.Among the treated patients,one patient developed a local hematoma at the puncture site and the other had transient right heart failure which was cured conservatively.
Pathological findings
In order to investigate the pathologic changes in B-CS patients,32 liver samples were collected during operation or by biopsy.Hepatic parenchymal congestion,sinusoidal dilatation and moderate to severe necrosis and hemorrhage were identified.Fibrosis was also seen in both groups and was heterogeneously distributed;the global grading evaluation was grade 1 in 3 patients,grade 2 in 7,grade 3 in 13,and grade 4 in 6.Otherwise,in these patients,thefibrosis alternated with regional congestion and necrosis.

Fig.1.Intra- and extrahepatic collaterals in patients with B-CS.A:Typical "spider web" sign or large connecting veins between accessory and MHVs; B:Establishment of spontaneous porto-systemic shunt by enlarged coronary vein and esophageal veins; C:Collaterals of left renal-hemiazygos pathway; D and E:Vertebrolumbar-azygos pathway and superficial collaterals of the abdominal wall were the most common pathway; F:Phrenic vein which communicates with the occluded hepatic veins.

Fig.2.Diagnosis and collaterals in one patient with B-CS.A:Connecting veins among the hepatic veins and thrombosis in the IVC; B:Formation of phrenic-pericardiophrenic collateral; C:Deep tributaries of azygos and hemiazygos veins (white arrow) and extrahepatic collaterals from liver capsule to the heart (black arrow).
Outcomes of follow-up
Median follow-up was 32.3 months (mean 21.3;range 3-61).In the course of follow-up,the patients in group A survived with good systemic status except for re-stenosis in one patient who underwent recanalization of the IVC and stent implantation.In group B,10 patients were in good systemic status except one patient had a meso-caval shunt because of deterioration.
Long-term evaluation of liver morphology in 11 invasively-treated patients demonstrated that hepatomegaly disappeared in 8 and the other 3 had no evident change.In addition,splenomegaly and hypersplenism were also ameliorated greatly in these patients (data not shown).In comparing pre-treatment values offibrosis grades,significant improvement was seen in the patients with lower gradefibrosis.In untreated patients,16 biopsies obtained from 8 patients indicated mild to severefibrosis but no pathologic progress was identified in the course of follow-up.The results of endoscopy and/or double-contrast barium examination of the upper gastrointestinal tract did not show deterioration of the varicose veins.
Illustrative case report
A 54-year-old man with mild ascites and edema of the lower extremities was treated at our hospital.Four years ago,he had a medical history of upper gastrointestinal bleeding.Liver function indicated Child-Pugh B.Doppler ultrasound examination confirmed the diagnosis of B-CS.Owing to the long-term segment obstruction and thrombosis of the IVC,radical resection of the IVC lesion was not suitable.In consideration of medical cost,we could not take invasive measures for the patient.But his systemic condition improved after medical treatment.After 21 days of treatment,the manifestations were greatly alleviated and liver function improved to Child-Pugh A; the ascites receded gradually twelve months later.The patient came six months later for a regular follow-up visit,and CT angiography demonstrated not only the segmental obstruction of the IVC and MHVs but the development of intra- and extrahepatic collaterals (Fig.2).At his last follow-up visit,4.2 years after the admission,the patient is alive without disease aggravation.
Discussion
B-CS is a complicated syndrome caused by IVC and/or MHV obstruction.Traditionally,early treatment is applied as soon as the diagnosis is established.[2]However,clinical data failed to show favorable peri-operative mortality and long-term outcomes.[15-17]In the past decades,identification of collaterals by imaging is highly diagnostic of B-CS.[18-20]Owing to these collaterals,asymptomatic cases of B-CS usually present fortuitously and these patients come to a spontaneous stabilization without any invasive treatment.[12]Therefore,the collaterals play an important role in the management strategy.[21]For patients without apparent symptoms and signs,the indications for invasive treatment have never been discussed and the feasibility of follow-up without special treatment had never been investigated.In the present study,intra- and extrahepatic collaterals to some extent were demonstrated in most patients,especially those in group B.Our results indicated that for some B-CS patients with complete compensation by collaterals,invasive treatment is not necessary and it is possible to manage in the outpatient department by regular follow-up.
The natural history of B-CS is poorly understood as most patients receive some form of treatment.[22,23]The primary objective of treatment is to prevent further deterioration of liver function by reconstructing the occluded IVC and/or reopening the occluded hepatic veins.[24,25]However,slow obstruction of 2 or 3 major veins produces a chronic presentation or,when accompanied by extensive collaterals,no symptoms at all.[14]Therefore,in clinical practice,presentation varies from a fulminant picture to an asymptomatic condition.For the latter,therapy may not be needed.[14,26]It is noted that in spite of marked development of intra- and extrahepatic collaterals,rich collaterals are only observed in a proportion of B-CS patients.The relationship between stage of liver pathology,disease history and diameter of the collateral vein is individually different.
According to our clinical experience,asymptomatic patients are commonly identified,especially in recent years.With the compensation by collaterals,the pressure of the IVC and portal vein decrease greatly and some patients have no obvious symptoms or just mild discomfort and physical signs.Although traditional surgical procedures such as mesoatrial,mesojugular,and splenoatrial shunts are performed to decompress the portal hypertension (PHT) directly and achieve effective short-term outcomes,the perioperative mortality and morbidity are very high and a long prosthetic graft can thrombose despite anticoagulation therapy.[2,4,15,16]Therefore,it is doubtful whether these treatment modalities are suitable for the management of these B-CS patients.However,the necessity,indications and feasibility of invasive management for B-CS patients were not clear.
In the present study,we found that the mean IVC pressure and FHP in patients without invasive treatment were almost equal,and a little higher than the normal IVC pressure (12.3±3.9 mmHg).[27]For B-CS patients,assessment of the compensational situation of IVC hypertension by collaterals was difficult.Thus,for the first time,we propose that if the IVC pressure and FHP are lower than 12.9 mmHg and the patients have no apparent symptoms and signs,intervention is not necessary.These patients attained complete compensation spontaneously by the development of intra- and extrahepatic collaterals.These collaterals developed in an attempt to shunt venous blood to the systemic system via varied routes effectively alleviating the IVC hypertension and PHT.
Although the possibility of non-therapy was indicated practically in this study,with anticoagulation alone,some patients with acute presentation may recover spontaneously,at least partially,as judged from a rapid decrease in serum aminotransferase levels,disappearance or easy control of ascites,and improvement in liver function.[28]The results of this study further confirmed this point.However,aggravation may occur unpredictably in the form of ascites becoming refractory,wasting,recurrent gastrointestinal bleeding,or development of liver failure.So,in the management of our patients,careful follow-up was conducted and 1 patient underwent surgical treatment in the course of follow-up.
B-CS is a type of retro-hepatic PHT and its prognosis is very different from that of intrahepatic PHT(such as HBV-associated cirrhosis).In the management of HBV-associated PHT,medical treatment is carried out in most cases and invasive procedures are only performed when complications such as refractory ascites and gastroesophageal bleeding develop due to hepatic pathology.It remains to be seen whether this strategy is suitable for the management of B-CS patients,and further investigation is needed of more cases and longterm follow-up results.
In this study,we obtained information on IVC pressure and FHP which related to pathology of the IVC and MHVs.But for patients with lesions of the MHVs alone,the measurement of hepatic venous wedge pressure and the hepatic venous pressure gradient,which are indices of portal pressure,was technically difficult.Therefore,direct assessment of the compensation for PHT on the clinical manifestations and biochemical tests alone are not dependable.In order to get a comprehensive understanding of the compensation situation,endoscopy and/or double-contrast barium examination of the upper gastrointestinal tract was also performed in our study,which helped us assess the possibility of variceal bleeding.In addition,changes of liver pathology reminded us of the progression of the disease through inhomogeneous distribution and sampling variation.[7]
In conclusion,our new strategy demonstrates that,for some B-CS patients with rich collaterals which compensate for the manifestations of IVC hypertension and/or PHT,the indications for invasive treatment should be stricter despite technical improvements.Because clinical manifestations may be subtle,and liver biopsy usually provides nonspecific information in B-CS patients,a general note of caution is therefore necessary with regard to the progression of the disease.In order to get a complete evaluation of the patients who need invasive treatment,the comprehensive assessment of clinical data,advantages and disadvantages should be taken into consideration especially for patients with complicated pathologies in the IVC and MHVs.
Acknowledgement
The authors thank Yan Wu,Department of Radiology and Rui-Fang Zhang,Department of Ultrasound Diagnosis,Zhengzhou University,School of Medicine,for their excellent technical assistance.
Funding:This study was supported by a grant from the Zhengzhou University Fund (340600532015) and Henan Provincial Natural Science Foundation (112300410116).
Ethical approval:Not needed.
Contributors:SYL proposed the study.FY wrote the first draft and analyzed the data.All authors contributed to the design and interpretation of the study and to further drafts.SYL is the guarantor.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Darwish Murad S,Valla DC,de Groen PC,Zeitoun G,Hopmans JA,Haagsma EB,et al.Determinants of survival and the effect of portosystemic shunting in patients with Budd-Chiari syndrome.Hepatology 2004;39:500-508.
2 Martin LG,Henderson JM,Millikan WJ Jr,Casarella WJ,Kaufman SL.Angioplasty for long-term treatment of patients with Budd-Chiari syndrome.AJR Am J Roentgenol 1990;154:1007-1010.
3 Prandi D,Rueff B,Benhamou JP.Side-to-side portacaval shunt in the treatment of Budd-Chiari syndrome.Gastroenterology 1975;68:137-141.
4 Behera A,Menakuru SR,Thingnam S,Kaman L,Bhasin DK,Kochher R,et al.Treatment of Budd-Chiari syndrome with inferior vena caval occlusion by mesoatrial shunt.Eur J Surg 2002;168:355-359.
5 Orloff MJ,Girard B.Long term results of treatment of Budd-Chiari syndrome by side to side portacaval shunt.Surg Gynecol Obstet 1989;168:33-41.
6 Vons C,Smadja C,Bourstyn E,Szekely AM,Bonnet P,Franco D.Results of portal systemic shunts in Budd-Chiari syndrome.Ann Surg 1986;203:366-370.
7 Tanaka M,Wanless IR.Pathology of the liver in Budd-Chiari syndrome:portal vein thrombosis and the histogenesis of veno-centric cirrhosis,veno-portal cirrhosis,and large regenerative nodules.Hepatology 1998;27:488-496.
8 Aydinli M,Bayraktar Y.Budd-Chiari syndrome:etiology,pathogenesis and diagnosis.World J Gastroenterol 2007;13:2693-2696.
9 Chawla Y,Kumar S,Dhiman RK,Suri S,Dilawari JB.Duplex Doppler sonography in patients with Budd-Chiari syndrome.J Gastroenterol Hepatol 1999;14:904-907.
10 Terasaki M,Kitai T,Morimoto T,Kumada K,Sasaki H,Nakano M,et al.Hemodynamics and hepatic energy metabolism in canine model of acute hepatic venous occlusion with mesocaval shunt.Eur Surg Res 1994;26:19-27.
11 Meng XC,Zhu KS,Qin J,Zhang JS,Wang XH,Zou Y,et al.Clinical significance of multislice spiral CT scans in hepatic veins occlusion in Budd-Chiari syndrome.Chin Med J (Engl)2007;120:100-105.
12 Plessier A,Sibert A,Consigny Y,Hakime A,Zappa M,Denninger MH,et al.Aiming at minimal invasiveness as a therapeutic strategy for Budd-Chiari syndrome.Hepatology 2006;44:1308-1316.
13 Langlet P,Escolano S,Valla D,Coste-Zeitoun D,Denie C,Mallet A,et al.Clinicopathological forms and prognostic index in Budd-Chiari syndrome.J Hepatol 2003;39:496-501.
14 Hadengue A,Poliquin M,Vilgrain V,Belghiti J,Degott C,Erlinger S,et al.The changing scene of hepatic vein thrombosis:recognition of asymptomatic cases.Gastroenterology 1994;106:1042-1047.
15 Xu PQ,Ma XX,Ye XX,Feng LS,Dang XW,Zhao YF,et al.Surgical treatment of 1360 cases of Budd-Chiari syndrome:20-year experience.Hepatobiliary Pancreat Dis Int 2004;3:391-394.
16 Feng LS,Peng QP,Li K,Ma XX,Zhao YF,Ye XX,et al.Management of severe Budd-Chiari syndrome:report of 147 cases.Hepatobiliary Pancreat Dis Int 2004;3:522-525.
17 Sun YL,Xu PQ,Ma XX,Feng LS,Dang XW,Li DX,et al.Analysis of Peri-operative risk factors in patients with Budd-Chiari syndrome.Zhongguo Pu Tong Wai Ke Za Zhi 2009;18:561-563.
18 Cho OK,Koo JH,Kim YS,Rhim HC,Koh BH,Seo HS.Collateral pathways in Budd-Chiari syndrome:CT and venographic correlation.AJR Am J Roentgenol 1996;167:1163-1167.
19 Erden A,Erden I,Karayalcin S,Yurdaydin C.Budd-Chiari syndrome:evaluation with multiphase contrast-enhanced three-dimensional MR angiography.AJR Am J Roentgenol 2002;179:1287-1292.
20 Naganuma H,Ishida H,Konno K,Komatsuda T,Hamashima Y,Ishida J,et al.Intrahepatic venous collaterals.Abdom Imaging 1998;23:166-171.
21 Sun YL,Ma XX,Xu PQ,Guan S.Stage management of Budd-Chiari syndrome.Zhonghua Pu Tong Wai Ke Za Zhi 2010;25:202-204.
22 Janssen HL,Garcia-Pagan JC,Elias E,Mentha G,Hadengue A,Valla DC,et al.Budd-Chiari syndrome:a review by an expert panel.J Hepatol 2003;38:364-371.
23 Ohta M,Hashizume M,Tomikawa M,Ueno K,Tanoue K,Sugimachi K.Analysis of hepatic vein waveform by Doppler ultrasonography in 100 patients with portal hypertension.Am J Gastroenterol 1994;89:170-175.
24 Koja K,Kusaba A,Kuniyoshi Y,Iha K,Akasaki M,Miyagi K.Radical open endvenectomy with autologous pericardial patch graft for correction of Budd-Chiari syndrome.Cardiovasc Surg 1996;4:500-504.
25 Kuniyoshi Y,Koja K,Akasaki M,Miyagi K,Shimoji M,Kudaka M,et al.Improvement in esophageal varices and liver histology postoperatively in Budd-Chiari syndrome.Ann Thorac Surg 1998;65:1711-1714.
26 Henderson JM,Warren WD,Millikan WJ Jr,Galloway JR,Kawasaki S,Stahl RL,et al.Surgical options,hematologic evaluation,and pathologic changes in Budd-Chiari syndrome.Am J Surg 1990;159:41-50.
27 Hsia TY,Khambadkone S,Redington AN,de Leval MR.Effect of fenestration on the sub-diaphragmatic venous hemodynamics in the total-cavopulmonary connection.Eur J Cardiothorac Surg 2001;19:785-792.
28 Valla DC.The diagnosis and management of the Budd-Chiari syndrome:consensus and controversies.Hepatology 2003;38:793-803.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Predictors of patient survival following living donor liver transplantation
- Hepatocellular carcinoma HepG2 cell apoptosis and caspase-8 and Bcl-2 expression induced by injectable seed extract of Coix lacryma-jobi
- A new scoring system for assessment of liver function after successful hepatectomy in patients with hepatocellular carcinoma
- Relationship between alcohol consumption and clinical manifestation of patients with fatty liver:a single-center study
- Oncofetal antigen glypican-3 as a promising early diagnostic marker for hepatocellular carcinoma
- Evaluation of hepatitis B viral replication and proteomic analysis of HepG2.2.15 cell line after knockdown of HBx
