Predictors of patient survival following living donor liver transplantation
2011-06-11
Chengdu,China
Introduction
Liver transplantation is widely accepted as the only curative therapy for patients with end-stage liver disease.It may cure cirrhosis,malignancies and severe liver dysfunction.[1]Excellent long-term survival rates for patients with both benign liver diseases and malignancies have been reported.[2,3]However,these encouraging outcomes are greatly limited by the shortage of grafts,especially in Asian countries.[4]Since 1989,when Strong et al[5]performed the first successful liver transplantation from a living donor to her son who was diagnosed with biliary atresia,living donor liver transplantation (LDLT) has emerged as one of the effective alternatives to deceased donor liver transplantation (DDLT).However,right hepatectomy may impose a high surgical risk on the donor.[4]Determining which recipients will benefit from LDLT is a realistic problem that is of concern not only to transplant surgeons but also to the donor and recipient families.Studies in the literature have reported some risk factors that affect recipient and graft survival after liver transplantation.[6,7]However,those risk factors are based on DDLT.Whether they pertain to LDLT has not been well established.The purpose of this study was to determine which pre- and intra-operative factors in fluence the outcome of LDLT.
Methods
Patients and clinical characteristics
All adult patients (≥18 years; n=102) with benign liver diseases who had undergone their first LDLT between 2002 and 2009 at our center were considered for this study.Transplantations were approved by the Ethics Committee of West China Hospital,Sichuan University.We examined the characteristics of the donors,recipients,grafts and intraoperative factors,including age,gender,body mass index (BMI),gender disparity,ABO blood-type disparity,model for end-stage liver diseases (MELD) score,Child-Pugh score,preoperative renal dysfunction,graft-to-recipient weight ratio (GRWR),cold ischemia time (CIT),surgical duration,transfusion of red blood cells (RBCs) and platelets.[8]MELD scores were calculated according to the formula:MELD score=9.57×Ln creatinine (mg/dL)+11.2×(Ln INR)+3.78×Ln bilirubin(mg/dL)+6.43.[9]The decision for transfusions was based on clinical and hemodynamic criteria.RBCs were used to maintain hemoglobin levels above 7.0 g/dL.[7,10]Platelet concentrates were administered if platelet counts decreased to 50×109/L.[7,10]Preoperative renal dysfunction was defined as the level of serum creatinine greater than 1.5 mg/dL.[11]The cut-off point of BMI was 23,as suggested by the World Health Organisation.[12]
The clinical characteristics of recipients and donors are shown in Table 1.The primary etiologies thatnecessitated transplantations included:hepatitis B (66 patients),fulminant hepatic failure (17),hepatolithiasis(4),Budd-Chiari syndrome (4),primary biliary cirrhosis(3),hepatic hydatid disease (2),alcoholic cirrhosis (2),hepatitis C (2),autoimmune hepatitis (1),and hepatic cyst (1).Five patients were diagnosed with diabetes mellitus before LDLT.Insulin injections were used to control blood sugar levels in one patient,whereas the other four were given oral diabetes medications.The median age of the recipients was 41 years (range 18-69 years) and the median age of the donors was 37 years (range 19-65 years).A higher proportion of both recipients and donors were male (84.31% and 57.84%,respectively).The mean of recipient and donor BMI was 22.38±2.93 and 22.85±2.05,respectively.In addition,39.22% (n=40) of the donors had BMIs >23,and 49.02%(n=50) of the recipients had BMIs >23.Although the transplantations were carefully performed,54 patients required transfusions of >5 units of allogenic RBCs.Due to preoperative hypersplenism and intra-operative bleeding,9 recipients required platelet transfusions.Overall,32 patients had high MELD scores (>25),and 32 had Child-Pugh A,50 Child-Pugh B,and 20 Child-Pugh C.Furthermore,14 patients had preoperative renal dysfunction due to hepatorenal syndrome,and 3 underwent pre-transplant dialysis due to severe renal dysfunction.The GRWR ranged from 0.63% to 1.27%with a mean of 0.91%; 23 recipients received small grafts(GRWR <0.8%).
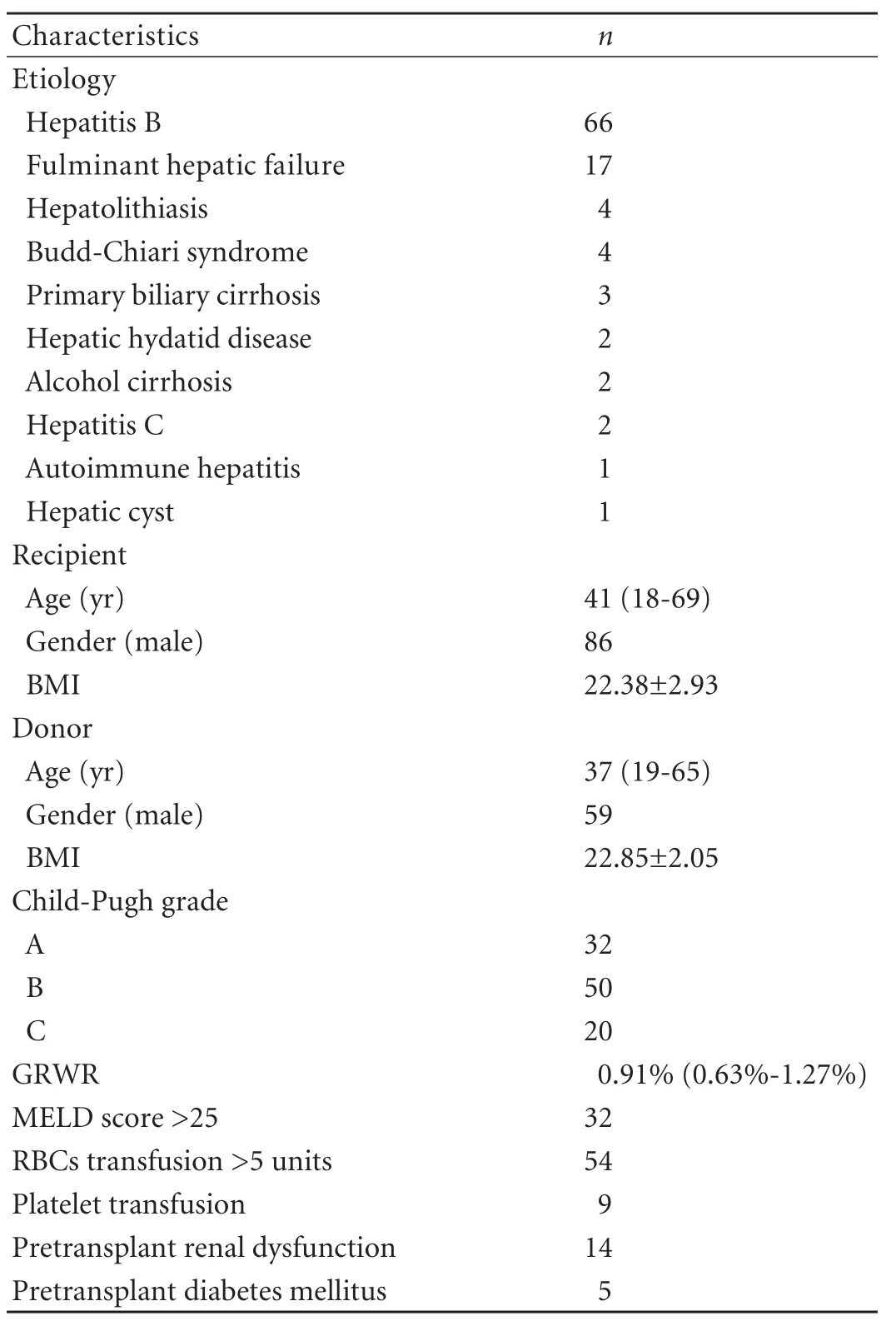
Table 1.Clinical characteristics of recipients and donors
Donor selection and surgical procedure
Donors were required to be healthy adult relatives with compatible ABO blood type and negative serum tests for HBV,HCV and human immunodeficiency virus.The donors were evaluated using computed tomography and volumetry to ensure that a right lobe without a middle hepatic vein that measured >40%of the estimated standard liver weight of the recipient and ≥30% of the total liver volume of the donor could possibly be removed.If not,dual LDLT was suggested.
The operation was performed through a right subcostal incision extended to the upper midline under general anesthesia.Abdominal exploration,liver biopsy and intraoperative cholangiograms were initially performed to assess the ratio of steatosis and the biliary anatomy of the donor.Thereafter,the first hepatic hilum was dissected,the right lobe of the liver was mobilized and the vena cava was dissected.Any short hepatic veins larger than 0.5 cm were preserved until harvesting for potential anastomosis in the recipient.The CUSAExceldevice was used to divide the liver parenchyma without in flow occlusion.The falciform ligament was reconstructed,the stumps of the right hepatic and portal veins were closed by continuous non-absorbable sutures,and a drain was inserted into the right subphrenic cavity before closure.[13]
Post-transplant management and follow-up
The post-transplant immunosuppression consisted of calcineurin inhibitors (CNI; tacrolimus or cyclosporine),mycophenolate mofetil and steroids.Steroid pulse therapy was administered to patients with rejection.The postoperative anti-HBV protocols consisted of lamivudine combined with therapy with a low-dose of intramuscular hepatitis B immune globulin.Hepatitis B immune globulin was administered to all recipients with HBV infection during and after the transplantation.[13-15]The recipients were followed up regularly until death or the termination of this study (May 2010).
Statistical analysis
Categorical variables were compared with the chisquare test or Fisher's exact test,whereas the analysis of variance was performed for continuous variables.Cox regression was used to assess the variables that were significantly associated with negative outcomes of LDLT in univariate analysis.Post-transplant survival was estimated using the Kaplan-Meier method with the log-rank test.The diagnostic accuracy of the predictors was assessed using receiver operating curve (ROC)analysis.For all analyses,we used SPSS version 13.0,and considered a P value of <0.05 to be statistically significant.
Results
Survival analysis
The median post-transplant follow-up was 27.32 months(range 0.03-101.7 months).During the study period,a total of 19 patients died.The causes of death were infection (n=8),multiple organ failure (6),renal failure(2),rejection (1),graft failure (1),or cerebrovascular accident (1).Among patients with pre-transplant renal dysfunction,6 recipients died of various causes,7 recovered,and 1 survived with slight renal dysfunction(without the need for dialysis).Overall,the 1-,3-,and 5-year survival rates for the recipients were 84%,76%,and 70%,respectively.
Risk factors for survival
After the clinical features were analyzed by univariate analysis,we found that preoperative renal dysfunction,RBCs transfusions greater than 5 units,female to male gender match,and recipients older than 60 years were significantly associated with recipient survival (Table 2).Pre-transplant MELD scores were not correlated with post-transplant survival.There were also no significant differences in survival among the patients with Child-Pugh A,B or C.GRWR less than 0.8% did not have any predictive power.
Multivariate analysis,using Cox regression,showed that preoperative renal dysfunction,RBC transfusions greater than 5 units,and female to male gender match were independent risk factors for death (Table 3).Significant differences were found among recipients with zero,one only,two and three risk factors usingthe Kaplan-Meier method with the log-rank test (Fig.A,P<0.0001).When the number of risk factors was analyzed and confirmed by multivariate analysis with an ROC,the best cut-off value for the number of risk factors was determined to be 2 (Fig.C).The corresponding area under the ROC was 0.704.We also compared the survival curve between patients with fewer than two risk factors and those with two or three of the risk factors.The overall 1-,3-,and 5-year survival rates of patients with one or less and two or more risk factors were 91%,86%,and 83% and 67%,56%,and 47%,respectively.There were significant differences in these rates (Fig.B,P<0.0001).
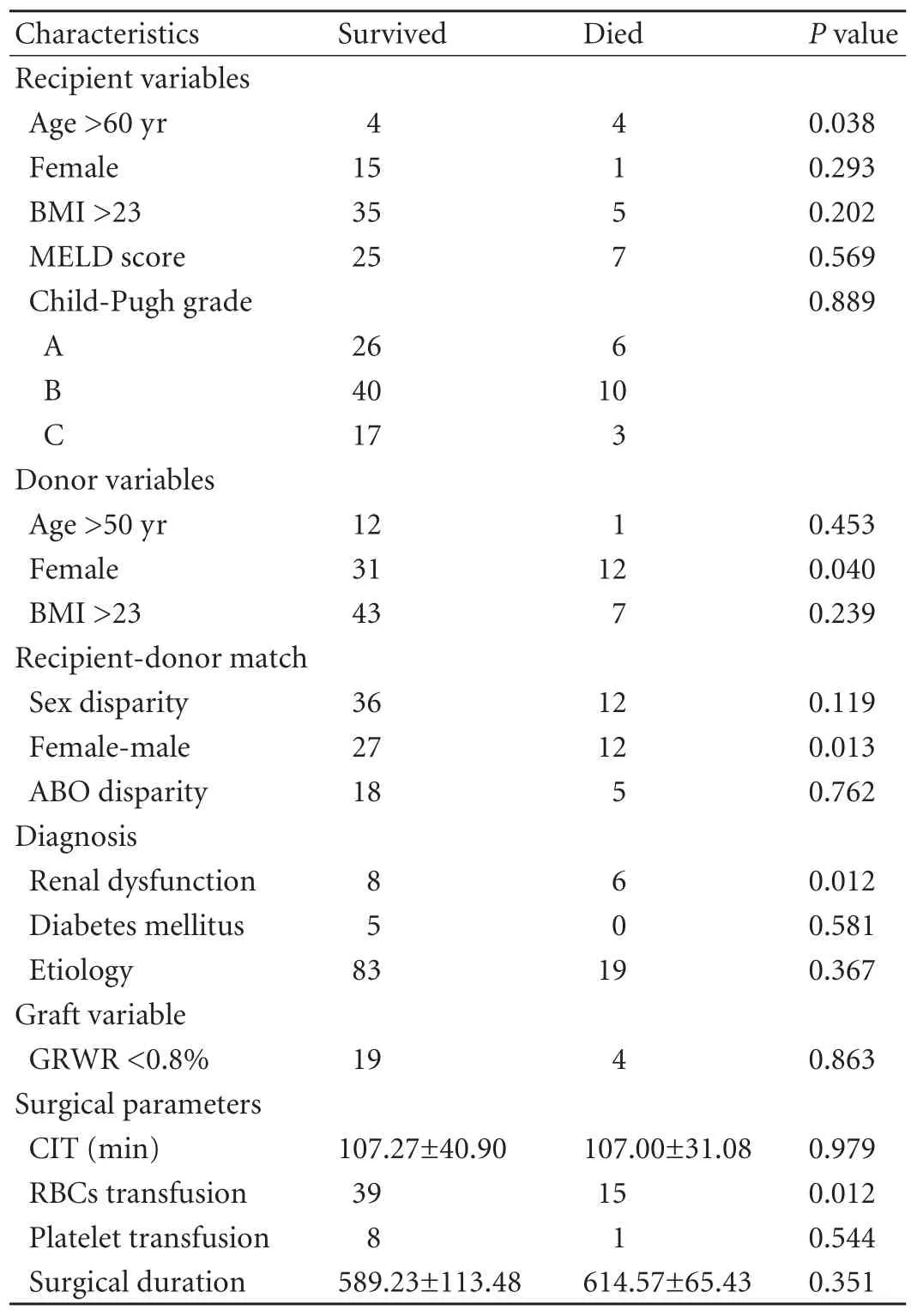
Table 2.Univariate analysis of factors associated with patients survival
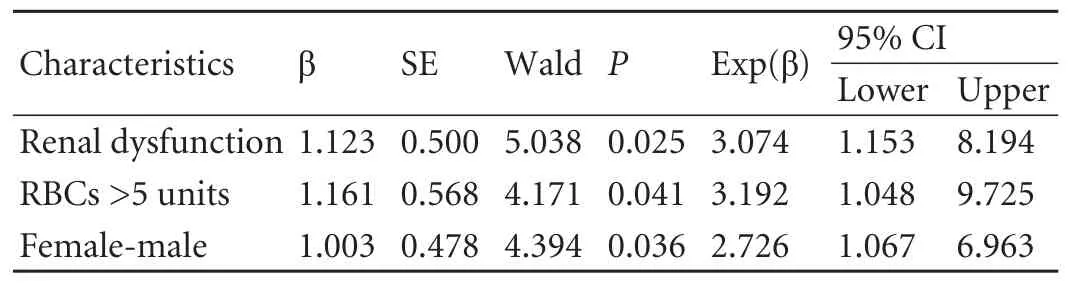
Table 3.Independent risk factors in the Cox regression for overall survival
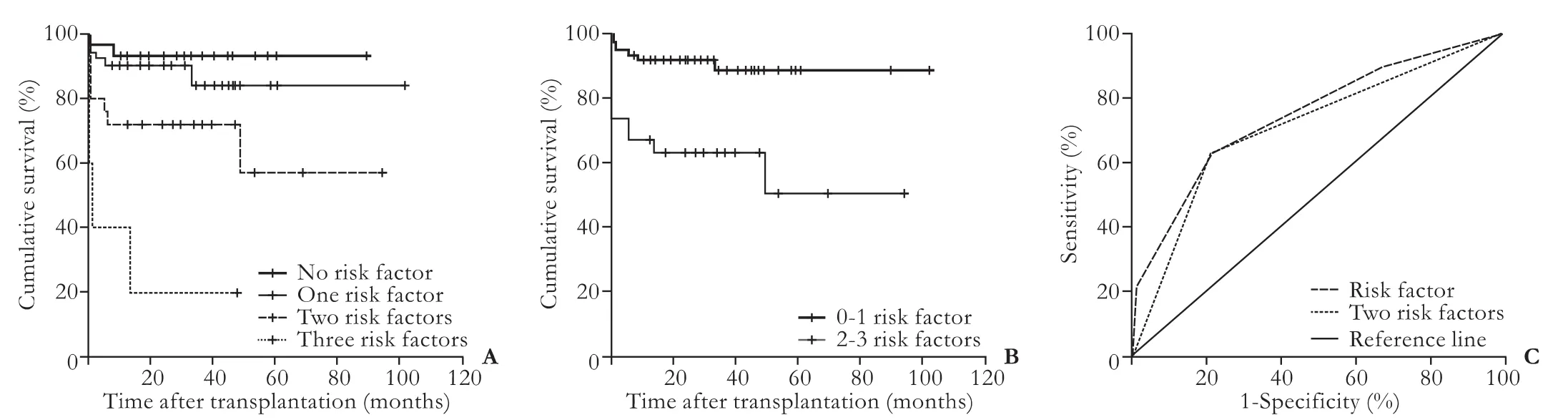
Fig.A:Cumulative survival curves for patients with zero,one,two or three risk factors that were confirmed by multivariate analysis(P<0.0001); B:Cumulative survival curves of patients with 0-1 risk factor and 2-3 risk factors that were confirmed by multivariate analysis (P<0.0001); C:ROC curve for the predictive risk factors that were confirmed by multivariate analysis.
Discussion
A number of studies have confirmed that MELD scores and Child-Pugh category may be good indicators for prediction of the outcome of liver transplantation.[4,6,16,17]However,our data showed that recipient mortality was closely associated with preoperative renal dysfunction,RBC transfusion and female to male gender match.These results were not surprising; in our previous study,[18]we confirmed that high pre-transplant MELD scores do not negatively impact short-term survival after liver transplantation.Although patients with high pre-transplant MELD scores are in extremely poor condition,they also experience a similar incidence of post-transplant complications,and the biochemical parameters recover quickly after LDLT.[18]Jacob et al[19,20]suggested that the outcomes after liver transplantation may depend on unpredictable events that occur during the perioperative period rather than on the severity of the underlying liver disease.
Pre-transplant renal dysfunction was an independent risk factor in our study.The correlations between recipient serum creatinine and early post-transplant sepsis,[21]length of stay in the intensive care unit,[22]the need for preoperative and postoperative dialysis,[21]financial burden,[23]hospital death,and postoperative survival[21,24-27]have been well defined by many investigators.In our study,14 patients were diagnosed with pre-transplant renal dysfunction.Unfortunately,six died from various causes.Among the six patients,five died during the perioperative period.This result is consistent with that reported previously.Furthermore,it was suggested that preoperative renal dysfunction also predicts a worse outcome in the long-term postoperative period.[24]
Our study confirmed that RBC transfusions of greater than 5 units have a negative impact on the outcome of LDLT.Many risks are involved in allogeneic blood transfusions,such as transfusion-related acute lung injury,bacterial sepsis and immunosuppressive effects.[10]A study[28]confirmed that massive blood product transfusions are not only associated with longer hospital stays but also are associated with reduced survival.However,in our study many patients received RBCs transfusions of greater than 5 units.We speculate that this may be due to massive hemorrhage of the upper gastrointestinal tract in many of the patients before transplantation.Moreover,many patients in our study had chronic anemia associated with digestive tract hemorrhage,hypersplenism and malnutrition.
A number of clinical and animal studies focusing on gender disparity,especially female to male gender match in solid organ transplantation showed that this may be associated with a negative outcome in the kidney,heart,lung,and liver transplantation.This was also revealed in our study.[29-33]Studies have confirmed that estrogens may impair the secretion of bile,resulting in disorders of biliary secretion.[34]Moreover,Wittnich et al[35]found increased acidosis in female livers during ischemia due to a rapid and greater degree of tissue lactate and H+accumulation.Except for metabolic factors,graft size was suggested as a potential explanation for this phenomenon by Gu et al.[36]They hypothesized that the complex in flammatory responses caused by perfusion contribute to the less favourable outcomes in male rat recipients with small-for-size female liver grafts.[36]However,our study confirmed that GRWR<0.8% did not show any prognostic power.Contrary to these studies,Lehner et al[37]suggested that genderincompatible liver transplantation may not achieve a poor outcome.Our data have shown that male recipients of female livers have a worse survival rate that is independent of recipient age and other clinical characteristics.However,currently,the mechanism underlying this is still unclear.
Our study suggested that patients with one or none of the identified risk factors achieved a much better survival than those with two or three risk factors.Pretransplant renal dysfunction is sometimes difficult to treat successfully unless the liver function has recovered.Therefore,intra-operative transfusions and gender matching may be the key to improving the outcome of recipients.Although blood transfusions often cannot be avoided during surgery,studies have struggled to minimize the intra-operative blood requirements.[10,28]Advances in surgical and anesthetic management of patients undergoing LDLT will decrease both intraoperative blood loss and the requirement for blood products.[10]Increased understanding of the risk factors of massive blood loss is another effective method.Ramos et al[28]suggested that preoperative hemoglobin level is an independent risk factor in the prediction of the need for RBCs transfusions.Moreover,Ramos et al[28]also emphasized that the normalisation of preoperative hemoglobin level reduces the intraoperative transfusion requirement.Nonetheless,strategies to reduce intraoperative blood use should be developed.In addition,female to male gender matching should be avoided when there is more than one qualified donor.
There are several limitations to our study.It was a retrospective,single-center study,with a limited number of patients,especially those of advanced age.Moreover,the censored rate of this investigation was slightly high because the follow-up duration was too short for the number of individuals.We believe a larger series and a multicentre study design would minimize these limitations.
In conclusion,our preliminary study showed that preoperative renal dysfunction,intraoperative RBC transfusions of more than 5 units,and female to male gender match were independent risk factors for recipient survival.Patients with two or more of these risk factors would achieve worse outcomes.
Funding:None.
Ethical approval:Not needed.
Contributors:LC and WTF proposed the study and wrote the first draft.LC analyzed the data.All authors contributed to the design and interpretation of the study and to further drafts.WTF is the guarantor.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Llovet JM,Bruix J.Novel advancements in the management of hepatocellular carcinoma in 2008.J Hepatol 2008;48:S20-37.
2 Mazzaferro V,Regalia E,Doci R,Andreola S,Pulvirenti A,Bozzetti F,et al.Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis.N Engl J Med 1996;334:693-699.
3 Abt PL,Desai NM,Crawford MD,Forman LM,Markmann JW,Olthoff KM,et al.Survival following liver transplantation from non-heart-beating donors.Ann Surg 2004;239:87-92.
4 Ishigami M,Honda T,Okumura A,Ishikawa T,Kobayashi M,Katano Y,et al.Use of the Model for End-Stage Liver Disease(MELD) score to predict 1-year survival of Japanese patients with cirrhosis and to determine who will benefit from living donor liver transplantation.J Gastroenterol 2008;43:363-368.
5 Strong RW,Lynch SV,Ong TH,Matsunami H,Koido Y,Balderson GA.Successful liver transplantation from a living donor to her son.N Engl J Med 1990;322:1505-1507.
6 Habib S,Berk B,Chang CC,Demetris AJ,Fontes P,Dvorchik I,et al.MELD and prediction of post-liver transplantation survival.Liver Transpl 2006;12:440-447.
7 Brandao A,Fuchs SC,Gleisner AL,Marroni C,Zanotelli ML,Cantisani G; et al.MELD and other predictors of survival after liver transplantation.Clin Transplant 2009;23:220-227.
8 Moore DE,Feurer ID,Speroff T,Gorden DL,Wright JK,Chari RS,et al.Impact of donor,technical,and recipient risk factors on survival and quality of life after liver transplantation.Arch Surg 2005;140:273-277.
9 Kamath PS,Kim WR; Advanced Liver Disease Study Group.The model for end-stage liver disease (MELD).Hepatology 2007;45:797-805.
10 de Boer MT,Christensen MC,Asmussen M,van der Hilst CS,Hendriks HG,Slooff MJ,et al.The impact of intraoperative transfusion of platelets and red blood cells on survival after liver transplantation.Anesth Analg 2008;106:32-44.
11 Lebrón Gallardo M,Herrera Gutierrez ME,Seller Pérez G,Curiel Balsera E,Fernández Ortega JF,Quesada García G.Risk factors for renal dysfunction in the postoperative course of liver transplant.Liver Transpl 2004;10:1379-1385.
12 Choo V.WHO reassesses appropriate body-mass index for Asian populations.Lancet 2002;360:235.
13 Ran S,Wen TF,Yan LN,Li B,Zeng Y,Chen ZY,et al.Risks faced by donors of right lobe for living donor liver transplantation.Hepatobiliary Pancreat Dis Int 2009;8:581-585.
14 Li C,Wen TF,Yan LN,Li B,Yang JY,Wang WT,et al.Outcome of hepatocellular carcinoma treated by liver transplantation:comparison of living donor and deceased donor transplantation.Hepatobiliary Pancreat Dis Int 2010;9:366-369.
15 Li J,Yan LN,Yang J,Chen ZY,Li B,Zeng Y,et al.Indicators of prognosis after liver transplantation in Chinese hepatocellular carcinoma patients.World J Gastroenterol 2009;15:4170-4176.
16 Brown RS Jr,Kumar KS,Russo MW,Kinkhabwala M,Rudow DL,Harren P,et al.Model for end-stage liver disease and Child-Turcotte-Pugh score as predictors of pretransplantation disease severity,posttransplantation outcome,and resource utilization in United Network for Organ Sharing status 2A patients.Liver Transpl 2002;8:278-284.
17 Guo Z,He X,Wu L,Ju W,Hu A,Tai Q,et al.Model for endstage liver disease versus the Child-Pugh score in predicting the post-transplant 3-month and 1-year mortality in a cohort of Chinese recipients.Surg Today 2010;40:38-45.
18 Li C,Wen T,Yan L,Li B,Wang W,Xu M,et al.Does model for end-stage liver disease score predict the short-term outcome of living donor liver transplantation? Transplant Proc 2010;42:3620-3623.
19 Jacob M,Copley LP,Lewsey JD,Gimson A,Toogood GJ,Rela M,et al.Pretransplant MELD score and post liver transplantation survival in the UK and Ireland.Liver Transpl 2004;10:903-907.
20 Jacob M,Lewsey JD,Sharpin C,Gimson A,Rela M,van der Meulen JH.Systematic review and validation of prognostic models in liver transplantation.Liver Transpl 2005;11:814-825.
21 Singh N,Gayowski T,Wagener MM.Posttransplantation dialysis-associated infections:morbidity and impact on outcome in liver transplant recipients.Liver Transpl 2001;7:100-105.
22 Lafayette RA,Paré G,Schmid CH,King AJ,Rohrer RJ,Nasraway SA.Pretransplant renal dysfunction predicts poorer outcome in liver transplantation.Clin Nephrol 1997;48:159-164.
23 Markmann JF,Markmann JW,Markmann DA,Bacquerizo A,Singer J,Holt CD,et al.Preoperative factors associated with outcome and their impact on resource use in 1148 consecutive primary liver transplants.Transplantation 2001;72:1113-1122.
24 Nair S,Verma S,Thuluvath PJ.Pretransplant renal function predicts survival in patients undergoing orthotopic liver transplantation.Hepatology 2002;35:1179-1185.
25 González E,Rimola A,Navasa M,Andreu H,Grande L,García-Valdecasas JC,et al.Liver transplantation in patients with non-biliary cirrhosis:prognostic value of preoperative factors.J Hepatol 1998;28:320-328.
26 Dellon ES,Galanko JA,Medapalli RK,Russo MW.Impact of dialysis and older age on survival after liver transplantation.Am J Transplant 2006;6:2183-2190.
27 Xu X,Ling Q,Wei Q,Wu J,Gao F,He ZL,et al.An effective model for predicting acute kidney injury after livertransplantation.Hepatobiliary Pancreat Dis Int 2010;9:259-263.
28 Ramos E,Dalmau A,Sabate A,Lama C,Llado L,Figueras J,et al.Intraoperative red blood cell transfusion in liver transplantation:in fluence on patient outcome,prediction of requirements,and measures to reduce them.Liver Transpl 2003;9:1320-1327.
29 Shaheen FA,al Sulaiman M,Mousa D,el Din AB,Hawas F,Fallatah A,et al.Impact of donor/recipient gender,age,HLA matching,and weight on short-term graft survival following living related renal transplantation.Transplant Proc 1998;30:3655-3658.
30 Sato M,Gutierrez C,Waddell TK,Liu M,Keshavjee S.Donor-recipient gender mismatch in lung transplantation:Impact on obliterative bronchiolitis and survival.J Heart Lung Transplant 2005;24:2000-2001.
31 Rustgi VK,Marino G,Halpern MT,Johnson LB,Umana WO,Tolleris C.Role of gender and race mismatch and graft failure in patients undergoing liver transplantation.Liver Transpl 2002;8:514-518.
32 Grande L,Rull A,Rimola A,Manyalic M,Cabrer C,Garcia-Valdecasas JC,et al.Impact of donor gender on graft survival after liver transplantation.Transplant Proc 1997;29:3373-3374.
33 Al-Khaldi A,Oyer PE,Robbins RC.Outcome analysis of donor gender in heart transplantation.J Heart Lung Transplant 2006;25:461-468.
34 Alvaro D,Mancino MG,Onori P,Franchitto A,Alpini G,Francis H,et al.Estrogens and the pathophysiology of the biliary tree.World J Gastroenterol 2006;12:3537-3545.
35 Wittnich C,Belanger MP,Askin N,Boscarino C,Wallen WJ.Lower liver transplant success in females:gender differences in metabolic response to global ischemia.Transplant Proc 2004;36:1485-1488.
36 Gu Y,Dirsch O,Dahmen U,Ji Y,He Q,Chi H,et al.Impact of donor gender on male rat recipients of small-for-size liver grafts.Liver Transpl 2005;11:669-678.
37 Lehner F,Becker T,Klempnauer J,Borlak J.Genderincompatible liver transplantation is not a risk factor for patient survival.Liver Int 2009;29:196-202.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Hepatocellular carcinoma HepG2 cell apoptosis and caspase-8 and Bcl-2 expression induced by injectable seed extract of Coix lacryma-jobi
- A new scoring system for assessment of liver function after successful hepatectomy in patients with hepatocellular carcinoma
- Relationship between alcohol consumption and clinical manifestation of patients with fatty liver:a single-center study
- Oncofetal antigen glypican-3 as a promising early diagnostic marker for hepatocellular carcinoma
- Necessity and indications of invasive treatment for Budd-Chiari syndrome
- Evaluation of hepatitis B viral replication and proteomic analysis of HepG2.2.15 cell line after knockdown of HBx
