Gallbladder cancer with tumor thrombus in the superior vena cava
2010-12-14SandeepBatraDineshChandraDovalUllasBatraPandalanghatSureshAmitDhimanandVineetTalwar
Sandeep Batra, Dinesh Chandra Doval, Ullas Batra, Pandalanghat Suresh,Amit Dhiman and Vineet Talwar
New Delhi, India
Gallbladder cancer with tumor thrombus in the superior vena cava
Sandeep Batra, Dinesh Chandra Doval, Ullas Batra, Pandalanghat Suresh,Amit Dhiman and Vineet Talwar
New Delhi, India
(Hepatobiliary Pancreat Dis Int 2010; 9: 325-328)
gallbladder carcinoma;superior vena cava;tumor thrombus;epidermal growth factor receptor
Introduction
Gallbladder cancer (GBC) is one of the most common gastrointestinal malignancies.[1]The incidence in Northern India, mainly along the Gangetic plains, is 4.5 cases per 100 000 population in men and 10.1 per 100 000 in women, comparable to data from Chile, which has the highest GBC incidence in the world (7.5 cases per 100 000 people). The tumor is almost always detected at a late stage. Moreover, a large number of patients who are operated upon are found to have an unresectable growth. GBC patients with advanced disease may present with hepatomegaly,a palpable mass, ascites, paraneoplastic syndromes,obstructive jaundice, and/or duodenal obstruction.Very rarely, the splenic vein,[2]portal vein,[3]adrenals,[4]distant lymph nodes[5]or intrahepatic inferior vena cava were involved by the tumor, or thrombosis due to pressure effects may lead to the development of portal vein thrombosis and/or inferior vena cava thrombosis.GBC causing superior vena cava (SVC) thrombosis,especially a metabolically active thrombus containing tumor cells, has not been reported until now.
Case report
A 60-year-old woman underwent laparoscopic cholecystectomy in 2006 with a presumptive diagnosis of cholelithiasis. Histopathology revealed a focus of adenocarcinoma in the mucosa along with cholelithiasis.No further treatment was given. She presented in mid-2008 with complaints of abdominal pain along with a lump in the right hypochondrium. Investigations including contrast-enhanced CT of the abdomenrevealed an ill-de fi ned mass in the subhepatic region in the liver along with in fi ltration into the recti abdominis,the port site of the previous laparoscopic procedure.Fine needle aspiration of the mass was positive for adenocarcinoma cells suggestive of recurrence of gallbladder carcinoma with anterior abdominal wall involvement. She was started on palliative chemotherapy with oxaliplatin, leucovorin, and 5- fl uorouracil(FOLFOX Ⅳ). After 3 cycles of chemotherapy, disease evaluation with PET-CT scan was suggestive of stable disease. In view of her poor tolerance to chemotherapy she was put on maintenance ge fi tinib-based anti-EGFR therapy along with monthly follow-up. During the 4th month of ge fi tinib therapy she presented with clinical signs and symptoms suggestive of SVC thrombosis (Fig. 1).
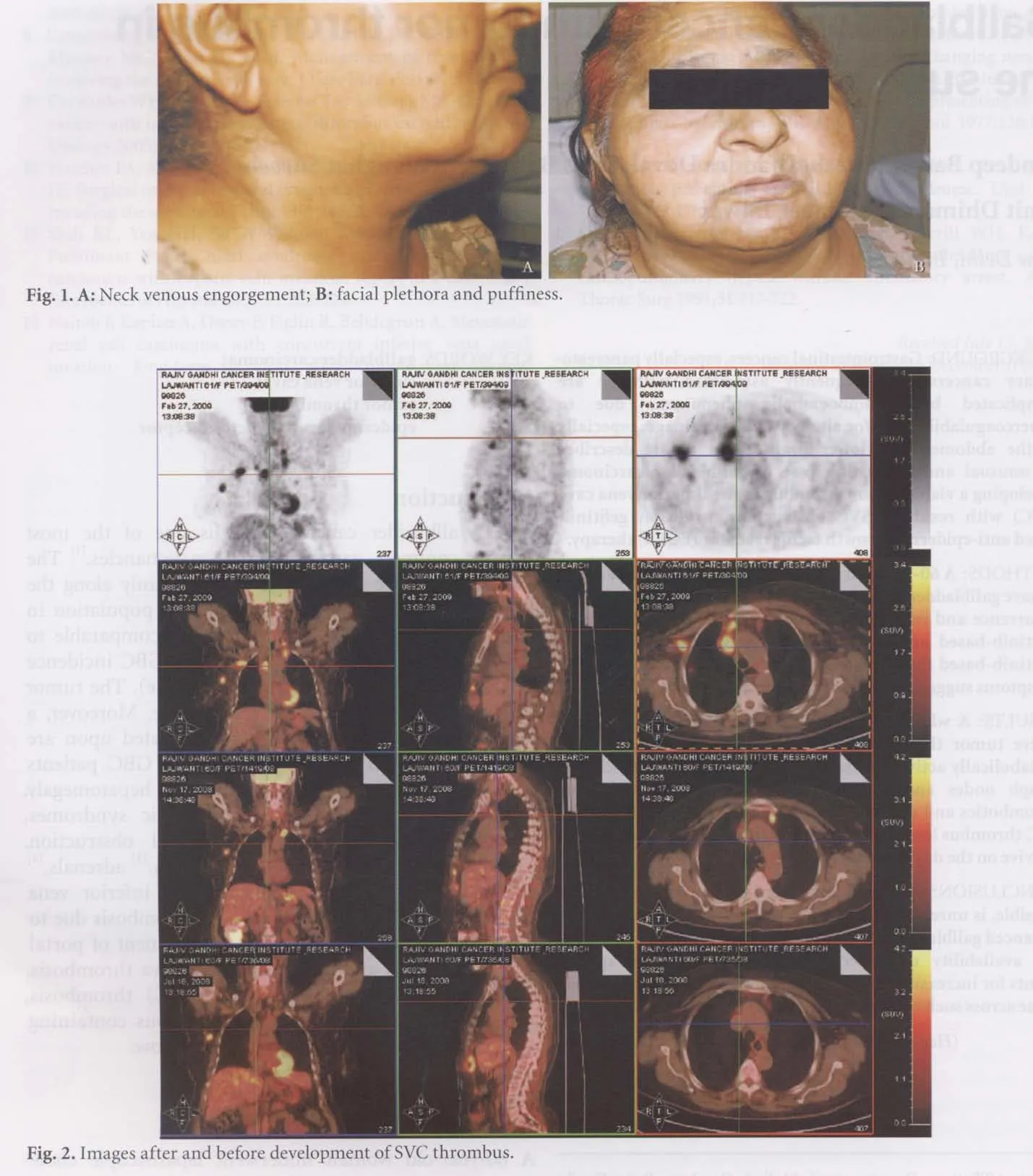
A whole body PET scan revealed an ill-de fi ned soft tissue lesion in the epigastric region with increased tracer uptake. A few small soft tissue nodules with increased tracer uptake were also seen in the xiphisternal region and along the right rectus abdominis muscle. Both lungs showed multiple variable-sized subpleural and parenchymal hypermetabolic nodules. Increased tracer uptake was also noted in enlarged supraclavicular, right axillary and right prevascular lymph nodes.
A metabolically active tumor thrombus in the SVC (Fig. 2) besides other sites of metabolically active disease inclusive of lung parenchyma, lymph nodes and abdomen was a new development when compared with prior PET-CT scans.
Therapeutical methods and symptoms after treatment
Discussion
Cancer per se is a hypercoagulable state with well recognized complications of deep vein thrombosis of the lower limbs and inferior vena cava.[3]Central venous catheter-induced thrombosis of the upper limb venous system is a well known complication in cancer patients.[6]A case has been reported of a patient with extensive paraneoplastic thrombosis of the sigmoid sinus and the internal jugular, brachiocephalic and subclavian veins on the left side developing one year prior to documentation of GBC.[7]
Cases of GBC associated with or developing the portal venous, inferior vena cava, and iliofemoral thrombosis are well known. However, never has it been reported that these thrombi were metabolically active on positron emission tomography, suggestive of harboring viable tumor cells.
Ge fi tinib use has been suggested to accelerate thromboembolic disease by TX/PG imbalance and platelet activation in acute myocardial infarction in a patient with lung cancer on ge fi tinib-based therapy.[8]
SVC thrombosis associated with GBC and/or associated with ge fi tinib use has not been reported in the English literature to our knowledge. To further add to the rarity, this is a tumor thrombus causing SVC obstruction. The route of entry of tumor cells in this case may have been through the venous/lymphatic drainage of the tumor in fi ltrating the upper anterior abdominal wall. This, along with the probable thrombogenicity of ge fi tinib, may have caused SVC thrombosis.
Our patient was started on radiotherapy for palliation of symptoms of SVC syndrome and she continues to survive on the date of writing this report.
Funding: None.
Ethical approval: Not needed.
Contributors: BS wrote the fi rst draft of this commentary. All authors contributed to the intellectual context and approved the fi nal version. BS is the guarantor.
Competing interest: No bene fi ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Batra Y, Pal S, Dutta U, Desai P, Garg PK, Makharia G, et al.Gallbladder cancer in India: a dismal picture. J Gastroenterol Hepatol 2005;20:309-314.
2 Legnani P, Weiss A. Early gallbladder cancer associated with idiopathic splenomegaly, splenic vein thrombosis and gastroesophageal varices. Am J Gastroenterol 2000;95: 2585-2586.
3 Iyomasa S, Matsuzaki Y, Hiel K, Kawai M, Matsunaga H,Yamaguchi Y. Adenosquamous carcinoma of the gallbladder with tumor thrombus in left portal trunk. J Hep Bil Pancr Surg 1997;4:332-336.
4 Rawat NS, Negi A, Sangwan S, Sharma U, Thukral BB, Saxena NC. Aggressive adenocarcinoma of gallbladder with distant metastasis and venous thrombosis at initial presentation.Indian J Radioline Imag 2006;16:499-501.
5 Shukla PJ, Barreto SG, Shrikhande SV, Mohandas KM,Purandare N, Rangarajan V. Detection of gallbladder cancer metastases in rare sites by PET scan. Indian J Gastroenterol 2007;26:303-304.
6 Sallah S, Wan JY, Nguyen NP. Venous thrombosis in patients with solid tumors: determination of frequency and characteristics. Thromb Haemost 2002;87:575-579.
7 Wirowski D, Treckmann J, Böhner H. Paraneoplastic thrombosis of the internal jugular and subclavian veins as fi rst manifestation of gall bladder cancer. Dtsch Med Wochenschr 2008;133:2562-2564.
8 Yamaguchi K, Kanazawa S, Kinoshita Y, Muramatsu M,Nomura S. Acute myocardial infarction with lung cancer during treatment with ge fi tinib: the possibility of ge fi tinibinduced thrombosis. Pathophysiol Haemost Thromb 2005;34:48-50.
BACKGROUND: Gastrointestinal cancers, especially pancreatobiliary cancers, are frequently associated with or are complicated by thromboembolic phenomena due to hypercoagulability and/or altered venous drainage, especially of the abdomen and lower limbs. This report describes an unusual and interesting case of gallbladder carcinoma developing a viable tumor thrombus in the superior vena cava(SVC) with resultant SVC obstruction, while on ge fi tinibbased anti-epidermal growth factor receptor (EGFR) therapy.METHODS: A 60-year-old woman was incidentally diagnosed to have gallbladder cancer on cholecystectomy. She had disease recurrence and
systemic chemotherapy followed by ge fi tinib-based anti-EGFR therapy. Subsequently, while on ge fi tinib-based therapy, she presented with clinical signs and symptoms suggestive of SVC thrombosis.
RESULTS: A whole body PET scan revealed a metabolically active tumor thrombus in the SVC, besides other sites of metabolically active disease inclusive of the lung parenchyma,lymph nodes and abdomen. She was treated with antithrombotics and external beam radiotherapy directed to the SVC thrombus leading to symptomatic relief. She continues to survive on the day of writing this report.
CONCLUSIONS: This rare complication, though theoretically possible, is unreported because of the short overall survival of advanced gallbladder cancer patients. This highlights that with the availability of better chemotherapeutic/biotherapeutic agents for increasing in the lifespan of cancer patients, we may come across such cases more frequently in the future.
Author Af fi liations: Department of Medical Oncology, Rajiv Gandhi Cancer Hospital, Sector 5, Rohini, New Delhi, 110085, India (Batra S, Doval DC, Batra U, Suresh P, Dhiman A and Talwar V)
Sandeep Batra, MD, Department of Medical Oncology, Rajiv Gandhi Cancer Hospital, Sector 5, Rohini, New Delhi,110085, India (Tel: 91-011-47022428; Fax: 91-011-27051037; Email:sandeepriya2000@yahoo.com)
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
palliative external beam RT to the chest and anterior abdominal wall ( in view of persistant pain at the scar site). The patient was put on low molecular weight heparin and was later overlapped and started on tab acitrom. One month later the patient complained of pain in right shoulder and back. MRI of spine revealed marrow lesion in multiple cervicodorsal spine and vertebrae C5 C6 C7 including their posterior elements and on the left side at C7 level and lesion involving D1 D2 and D3 vertebrae which was suggestive of metastatic involvement of nerve root canal. For severe pain she was started on palliative RT to right scapula and cervical spine. The patient continued waxing and waining mode of disease with overall progression of disease. Finally the patient died approximately 6 months after development of superion obstruction of the superior vana cava.
Received March 16, 2009
Accepted after revision December 25, 2009
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Budd-Chiari syndrome secondary to caval recurrence of renal cell carcinoma
- A prospective study on radiofrequency ablation locally advanced pancreatic cancer
- Liver graft vascular variant with 3 extra-hepatic arteries
- An effective model for predicting acute kidney injury after liver transplantation
- Pancreas transplantation in the mouse
- Integrity of the pancreatic duct-acinar system in the pathogenesis of acute pancreatitis