A prospective study on radiofrequency ablation locally advanced pancreatic cancer
2010-12-14RiccardoCasadeiClaudioRicciRaffaelePezzilliCarlaSerraLuciaCalculliAntonioMariaMorselliLabateDonatellaSantiniandFrancescoMinni
Riccardo Casadei, Claudio Ricci, Raffaele Pezzilli, Carla Serra, Lucia Calculli,Antonio Maria Morselli-Labate, Donatella Santini and Francesco Minni
Bologna, Italy
A prospective study on radiofrequency ablation locally advanced pancreatic cancer
Riccardo Casadei, Claudio Ricci, Raffaele Pezzilli, Carla Serra, Lucia Calculli,Antonio Maria Morselli-Labate, Donatella Santini and Francesco Minni
Bologna, Italy
(Hepatobiliary Pancreat Dis Int 2010; 9: 306-311)
pancreatic neoplasms;radiofrequency ablation;survival;ef fi cacy;safety
Introduction
Adenocarcinoma of the pancreas is one of the most aggressive human cancers.[1]Surgical resection is the only potentially curative treatment for pancreatic cancer, but at the time of diagnosis radical surgery is possible in only 5%-25% of patients, with a 5-year survival rate no more than 29%in high volume centers.[2]Forty percent of patients with pancreatic adenocarcinoma have unresectable locally advanced disease with massive encasement of the major vessels (the portal and superior mesenteric vein and/or the superior mesenteric artery and/or the hepatic artery).[3]Vascular reconstruction in these patients can be carried out with acceptable morbidity and mortality without a signi fi cant survival bene fi t.[4]Chemotherapy generally confers symptomatic improvement in these patients, improves the quality of life, and prolongs survival. Chemoradiation appears to be not superior to chemotherapy.[5]The patients who have undergone surgery with the purpose of curative resection for periampullary malignancies, but have been found to have an unresectable tumor should undergo a surgical biliary bypass.[6-8]Gastrojejunostomy is better than stent placement for treatment or prevention of gastric outlet obstruction in patients with a longer survival(non-metastatic) who are found to have unresectable pancreatic head cancer at laparotomy.[9,10]
Radiofrequency ablation (RFA) is a new, local thermal therapy used for the palliative treatment of solid parenchymal tumors.[11-18]RFA appears to be an attractive option in patients with unresectable, locally advanced and non-metastatic pancreatic cancer.[19]However, onlya few cases (fewer than 100) regarding the use of RFA in pancreatic cancer have been published. No authors have conducted prospective studies and few studies have reported long-term results.[20]In this paper, we report the results of a prospective study on the ef fi cacy and safety of RFA in pancreatic head adenocarcinoma.
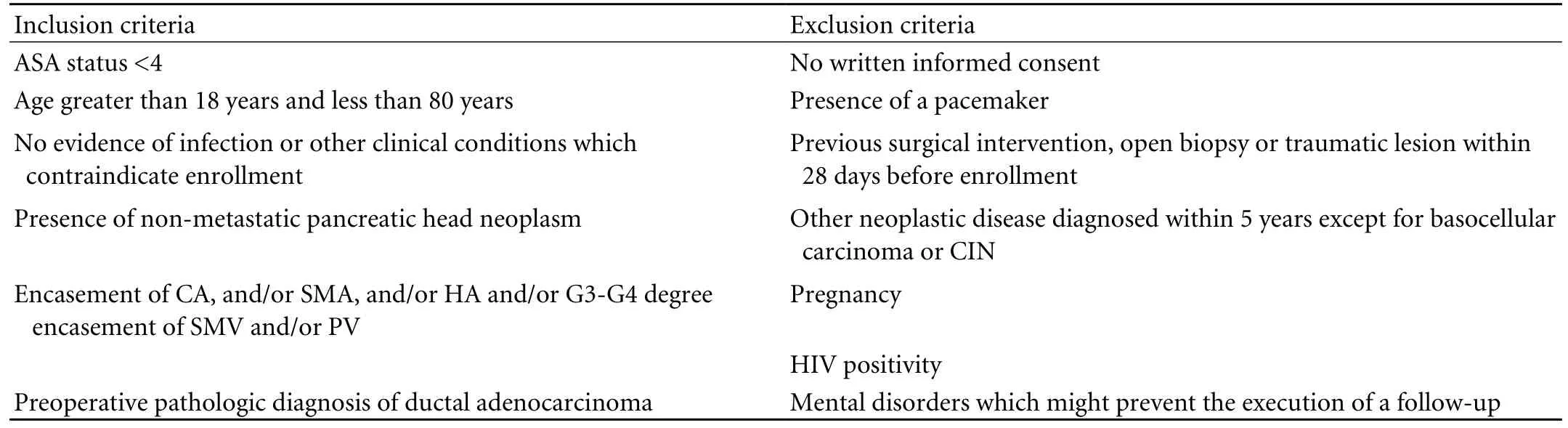
Table 1. Inclusion and exclusion criteria for eligibility for RFA
Methods
Only patients with a pancreatic head neoplasm,potentially non-metastatic and unresectable because of locally advanced disease, were recruited. This study was undertaken to evaluate the safety and effectiveness of RFA, improvement in the quality of life, and control of post-operative pain in addition to the survival bene fi t in patients who undergo RFA. Two interim analyses were planned at six and twelve months to evaluate the complication rate.
The inclusion and exclusion criteria for eligibility to RFA are listed in Table 1. In brief, the inclusion and exclusion criteria were based on past and present medical history, clinical examination, HIV-ab determination,and β-HCG serum levels to avoid pregnancy. Thoracoabdominal spiral multidetector computed tomography was carried out to assess the presence of a tumor in the pancreatic head, vascular encasement, and the absence of distant metastases. The degree of vascular involvement was assessed as reported by Calculli and colleagues.[21]Contrast-enhanced ultrasonography was carried out to exclude the presence of liver metastases. Endoscopic ultrasonography, magnetic resonance and diagnostic laparoscopy were conducted only in those patients in whom previous staging imaging did not exclude distant metastases or resectable disease. Subsequently, an ultrasonography-guided core biopsy was performed to obtain a pre-operative pathologic diagnosis. Finally, arestaging was also made at laparotomy.
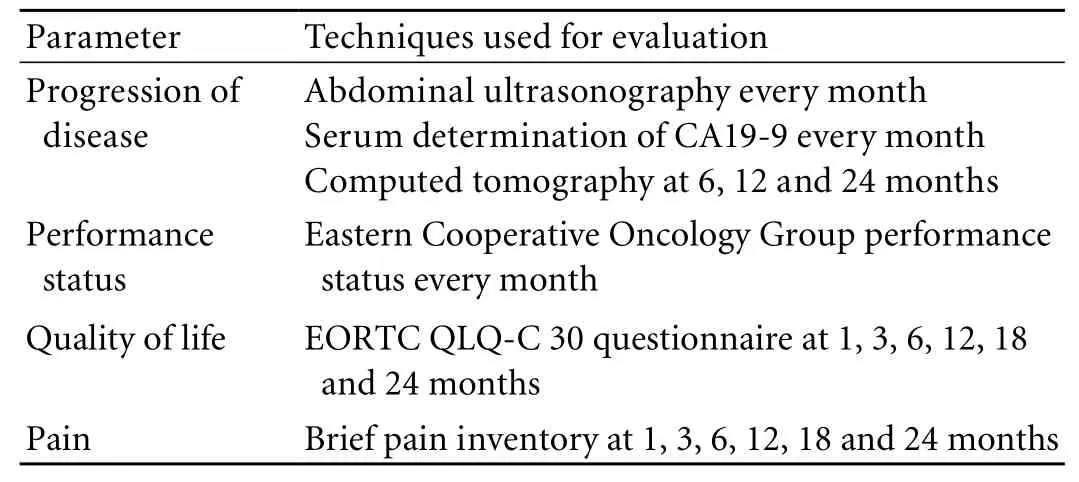
Table 2. Clinical and imaging parameters evaluated for follow-up assessment
The surgical technique was standardized as follows:the fi rst step was to mobilize the head of the pancreas;RFA was subsequently performed, usually with 2 or more passes of the probe at 90 ℃ for 5 minutes each.[22]RFA was carried out using the Cool-tipTMablation system (RadionicsTM). And fi nally, a double surgical bypass (hepaticojejunostomy "end to side" using a Roux loop and gastrojejunostomy) was performed to prevent the occurrence of biliary fi stula and duodenal occlusion.
The postoperative mortality rate included all deaths within 30 days after surgery. The postoperative morbidity rate included all complications following surgery until the day of discharge. A pancreatic fi stula was de fi ned as a drain output of any measurable volume of fl uid on or after postoperative day 3 with an amylase content greater than 3 times the serum amylase activity. Three different grades (A, B, C) were de fi ned according to the clinical impact on the patient’s hospital course.[23]The length of the postoperative period was de fi ned as the interval from the day of surgery to discharge. Chemotherapy was eventually performed in all patients with progression of the disease. The patients were followed up every month (Table 2). In brief, the progression of the disease was evaluated by abdominal ultrasonography, serum determination of CA19-9 every month, computed tomography at 6, 12 and 24 months, the performance status using the Eastern Cooperative Oncology Group (ECOG) Performance Status every month,[24]and the quality of life using the EORTC QLQ-C30 questionnaire[25]at 1, 3, 6, 12, 18, and 24 months; the pain was assessed using the brief pain inventory[26]at 1, 3, 6, 12, 18, and 24 months.
Sample size
According to the data reported,[27]the expected survival at 24 months was 35%. To differentiate this survival from the 3% value in an internal reference database named NeoPan[28]with a control-to-case ratio of 3:1, at a signi fi cance level of 0.05, and a power of 0.80,the estimated size of sample was 16 patients.[29]
Ethical approval
The study was carried out according to the principles of the Helsinki Declaration for human studies. It was approved on 17 July 2007 (code number 69/2007/O/Sper) by the Ethics Committee of Sant Orsola-Malpighi Hospital and written informed consent was given by each participant.
Statistical analysis
The mean, median, range, and frequency of the data of the patients were described statistically.
Results
From October 2007 to April 2008, 7 patients were enrolled in this study (Table 3). Their mean age was 66.1 years (range 47-80 years); 3 patients were male and 4 were female. Pre-operative staging revealed that only 4 patients were eligible for the RFA procedure (Table 4),2 were excluded because of the presence of a metastatic disease, and 1 was considered to have a resectable tumor. Hence RFA was carried out in 3 patients because a total pancreatectomy performed in one patient for a resectable tumor at laparotomy.
The mean size of the lesion undergoing RFA was 46.7 mm. In all patients the neoplastic lesions were completely ablated. Finally, biliary bypass and gastrojejunostomy were performed in all patients. No major intra-operative complications were registered,but extrasystolic arrhythmia was observed during radiofrequency ablation in one patient. In this series, the postoperative mortality rate was 0%, and the morbidity rate was 100%. All patients developed non-neoplasticself-limiting ascites, with normal fl uid amylase after 8.6 days on average (range 7-9 days) after RFA. A major complication occurred in a patient who developed a biliary fi stula 7 days after the procedure. The mean hospital stay was 21 days (range 10-43 days).
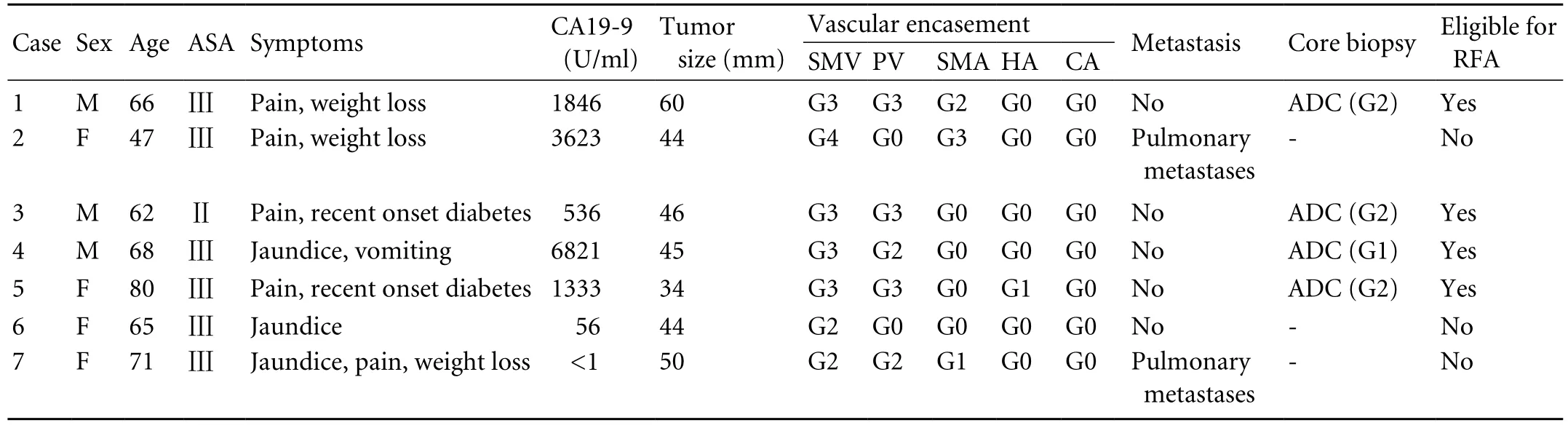
Table 3. Clinical, biochemical and radiological characteristics of patients enrolled in our study

Table 4. Outcome of patients eligible for RFA procedure
In the three patients CA19-9 serum levels reduced.Their preoperative values were higher than those at the fi rst month after surgical approach (from 1846, 536,and 1333 to 578, 108, and 418 U/ml respectively; upper reference value: 37 U/ml; Tables 3 and 4). Data on pain control and quality of life assessment were not available because of the poor clinical conditions of the patients.The median ECOG score of performance status was 3, 4 and 5 respectively at 1, 3 and 5 months after RFA.
The three patients died at 3, 4 and 5 months after treatment, two had no evidence of progression of disease, and one developed liver metastasis and portal thrombosis after 2 months. At the fi rst interim analysis the study was stopped.
Discussion
This is the fi rst prospective study evaluating RFA in clinical practice. In fact, a recent review of the literature[20]indicated that there are few studies reporting the RFA approach in human pancreatic cancer and that none of them were carried out in a prospective manner. The following critical points can be considered in RFA for unresectable, non-metastatic pancreatic head cancer:feasibility, safety, effectiveness, and long-term results.
Studies demonstrated that RFA is feasible in human pancreatic cancer,[20]but thermal injury of the intrapancreatic common bile duct should be taken into account as a complication of the ablation of lesions localized in the pancreatic head.[22]Also, RFA may cause inadvertent thermal necrosis of the portal vein,duodenum, or common intrapancreatic bile duct.These complications require surgical resection even in the presence of an unresectable tumor. Similarly, a late complication of RFA is duodenal occlusion as a result of fi brosis after ablation of the pancreatic tissue.Thus, ablation of pancreatic lesions, particularly in the pancreatic head, always require a laparotomy and a double surgical bypass.[19,30]
In our study, patients with unresectable and nonmetastatic disease who were con fi rmed at laparotomy underwent RFA. One patient was upstaged because of the objective limits of imaging techniques.[31]Thus, it is necessary to restage the tumor at laparotomy when a RFA approach is planned. In all patients, complete necrosis of the lesion was con fi rmed by intraoperative and postoperative ultrasonography. At least two passes of the probe were necessary to obtain a complete ablation of the lesion (mean size 46.7 mm). In our patients optimal thermal kinetic characteristics were produced by a target temperature of 90 ℃ for 5 minutes. Thermal injury of the portal vein or other major intra-operative complications were not observed except extra-systoles in one patient during the RFA procedure. The relationship between the ablation procedure and this cardiac event has not been conclusively clari fi ed.
The safety of RFA for pancreatic cancer is still under debate. The reported major post-operative complications include septic shock, massive gastrointestinal bleeding,[32]pancreatic fi stulas[33]and severe acute pancreatitis.[34]Elias et al[34]reported their experience with two patients with diffuse pancreatic metastases of renal cancer.Both patients developed severe acute pancreatitis after RFA and died. The result was probably due to multiple ablations, to the high temperature used (>90 ℃), and to the lack of adequate instrumentation. In our experience,however, we did not observe severe acute pancreatitis.
Tang et al[33]reported a frequency of 16.7% for pancreatic fi stulas and a postoperative mortality of 22.2% in 18 patients with unresectable pancreatic tumors who underwent RFA. They concluded that the standard use of cool-tip RFA is dangerous for patients with pancreatic head carcinoma but safe for those with tumors in the body and tail of the pancreas. We did not fi nd any pancreatic fi stulas. In one patient, there was a major biliary fi stula caused by surgical procedure. The data of our study were consistent with those of Koninger and colleagues[35]who reported a complication rate of 29% to 40% related to biliary surgical bypass in unresectable peri-ampullary cancer.
Self-limiting ascites with normal fl uid amylase occurred within 7-9 days after the procedure in all patients.Varshney et al[36]reported a similar complication. In our patients postoperative CA19-9 serum levels decreased, as previously reported[19,30,36]We hypothesized that this marker may be used as an index of tumor volume after RFA.[37]Our study assessed the effectiveness and longterm results of RFA for pancreatic cancer. Only two non-randomized retrospective studies were conducted using a cohort of comparison for long-term results.[27,32]One study evaluated 20 patients with unresectable and metastatic carcinomas of the pancreas (stage Ⅳ). No statistical differences were found in the prognosis of these patients as compared with those of the same stage who did not receive any treatment with RFA.[32]Our experience does not answer this question because we excluded patients with hepatic or pulmonary metastases.Another study was carried out on 25 consecutive patients who underwent palliative therapy for unresectable pancreatic cancer. Thirteen patients received palliative therapy alone and the other 12 received surgical palliative therapy plus RFA. The overall mean survival rate in the patients who were treated with palliative therapy was 13 months whereas those who also received RFA had a mean survival of 33 months. The differences in survival rates was statistically signi fi cant (P=0.0048). When the difference in survival rates was calculated for patients of the same stage, RFA provided survival bene fi ts especially for patients with stage Ⅲ pancreatic cancer (P=0.0032),whereas stage Ⅳ patients had survival rates similar to patients of the same stage who did not receive RFA(P=0.1095).[27]
In our study, a survival rate at 3 months was 66.7%(2/3), whereas at 6 months it was nil. In our NeoPan series, the survival rates at 3 and 6 months was 91.7% and 73.3%, respectively. The small number of patients was not suitable for a statistical analysis with historical series.
In our 3 patients data on pain control and quality of life assessment were not available because of their poor clinical conditions. The median ECOG score of performance status was 3, 4 and 5 respectively at 1, 3 and 5 months after RFA. Because of the high complication rate,the poor clinical condition of the patients, and the absence of a survival bene fi t, we decided to terminate the study.
In our opinion, RFA is a feasible procedure but we have observed a high rate of postoperative complications but non-bene fi t of survival and quality of life. Finally, we do not recommend the RFA procedure in patients with locally advanced non-metastatic adenocarcinoma at least in our experimental conditions.
Acknowledgment
The authors wish to thank Prof. R. Corinaldesi who cared for the study patients.
Funding: None.
Ethical approval: The Ethics Committee of Sant' Orsola-Malpighi Hospital approved the study on 17 July 2007 (code number 69/2007/O/Sper).
Contributors: CR, PR and MF proposed the study. PR, CR and RC wrote the fi rst draft. AMML analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. PR is the guarantor.
Competing interest: No bene fi ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Brennan MF, Kattan MW, Klimstra D, Conlon K. Prognostic nomogram for patients undergoing resection for adenocarcinoma of the pancreas. Ann Surg 2004;240:293-298.
2 Neoptolemos JP, Stocken DD, Friess H, Bassi C, Dunn JA,Hickey H, et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med 2004;350:1200-1210.
3 Verslype C, Van Cutsem E, Dicato M, Cascinu S, Cunningham D, Diaz-Rubio E, et al. The management of pancreatic cancer.Current expert opinion and recommendations derived from the 8th World Congress on Gastrointestinal Cancer, Barcelona,2006. Ann Oncol 2007;18:vii1-10.
4 Smeenk HG, Incrocci L, Kazemier G, van Dekken H, Tran KT,Jeekel J, et al. Adjuvant 5-FU-based chemoradiotherapy for patients undergoing R-1/R-2 resections for pancreatic cancer.Dig Surg 2005;22:321-328.
5 Yip D, Karapetis C, Strickland A, Steer CB, Goldstein D.Chemotherapy and radiotherapy for inoperable advanced pancreatic cancer. Cochrane Database Syst Rev 2006;3:CD002093.
6 Andersen JR, Sorensen SM, Kruse A, Rokkjaer M, Matzen P. Randomised trial of endoscopic endoprosthesis versus operative bypass in malignant obstructive jaundice. Gut 1989;30:1132-1135.
7 Shepherd HA, Royle G, Ross AP, Diba A, Arthur M, Colin-Jones D. Endoscopic biliary endoprosthesis in the palliation of malignant obstruction of the distal common bile duct: a randomized trial. Br J Surg 1988;75:1166-1168.
8 Smith AC, Dowsett JF, Russell RC, Hat fi eld AR, Cotton PB.Randomised trial of endoscopic stenting versus surgical bypass in malignant low bileduct obstruction. Lancet 1994;344:1655-1660.
9 Jeurnink SM, van Eijck CH, Steyerberg EW, Kuipers EJ, Siersema PD. Stent versus gastrojejunostomy for the palliation of gastric outlet obstruction: a systematic review.BMC Gastroenterol 2007;7:18.
10 Lillemoe KD, Cameron JL, Hardacre JM, Sohn TA, Sauter PK,Coleman J, et al. Is prophylactic gastrojejunostomy indicated for unresectable periampullary cancer? A prospective randomized trial. Ann Surg 1999;230:322-330.
11 Jansen MC, van Hillegersberg R, Chamuleau RA, van Delden OM, Gouma DJ, van Gulik TM. Outcome of regional and local ablative therapies for hepatocellular carcinoma: a collective review. Eur J Surg Oncol 2005;31:331-347.
12 Simon CJ, Dupuy DE. Current role of image-guided ablative therapies in lung cancer. Expert Rev Anticancer Ther 2005;5:657-666.
13 Singletary ES. Feasibility of radiofrequency ablation for primary breast cancer. Breast Cancer 2003;10:4-9.
14 Boss A, Clasen S, Kuczyk M, Anastasiadis A, Schmidt D,Graf H, et al. Magnetic resonance-guided percutaneous radiofrequency ablation of renal cell carcinomas: a pilot clinical study. Invest Radiol 2005;40:583-590.
15 Wood BJ, Abraham J, Hvizda JL, Alexander HR, Fojo T. Radiofrequency ablation of adrenal tumors and adrenocortical carcinoma metastases. Cancer 2003;97:554-560.
16 Shariat SF, Raptidis G, Masatoschi M, Bergamaschi F, Slawin KM. Pilot study of radiofrequency interstitial tumor ablation(RITA) for the treatment of radio-recurrent prostate cancer.Prostate 2005;65:260-267.
17 Martel J, Bueno A, Ortiz E. Percutaneous radiofrequency treatment of osteoid osteoma using cool-tip electrodes. Eur J Radiol 2005;56:403-408.
18 Chiou YY, Hwang JI, Chou YH, Wang HK, Chiang JH, Chang CY. Percutaneous ultrasound-guided radiofrequency ablation of intrahepatic cholangiocarcinoma. Kaohsiung J Med Sci 2005;21:304-309.
19 Siriwardena AK. Radiofrequency ablation for locally advanced cancer of the pancreas. JOP 2006;7:1-4.
20 Pezzilli R, Ricci C, Casadei R, Serra C, Calculli L, Antonacci N, et al Radiofrequency ablation of pancreatic cancer: a new attractive approach or another unsuccessful technique for the treatment of pancreatic adenocarcinoma? Cancer Therapy 2008;6:741-744.
21 Calculli L, Casadei R, Amore B, Albini Riccioli L, Minni F, Caputo M, et al. The usefulness of spiral Computed Tomography and colour-Doppler ultrasonography to predict portal-mesenteric trunk involvement in pancreatic cancer.Radiol Med 2002;104:307-315.
22 Date RS, Biggins J, Paterson I, Denton J, McMahon RF, Siriwardena AK. Development and validation of an experimental model for the assessment of radiofrequency ablation of pancreatic parenchyma. Pancreas 2005;30:266-271.
23 Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J,et al. Postoperative pancreatic fi stula: an international study group (ISGPF) de fi nition. Surgery 2005;138:8-13.
24 Oken MM, Creech RH, Tormey DC, Horton J, Davis TE,McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982;5:649-655.
25 Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A,Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365-376.
26 Daut RL, Cleeland CS, Flanery RC. Development of the Wisconsin Brief Pain Questionnaire to assess pain in cancer and other diseases. Pain 1983;17:197-210.
27 Spiliotis JD, Datsis AC, Michalopoulos NV, Kekelos SP,Vaxevanidou A, Rogdakis AG, et al. Radiofrequency ablation combined with palliative surgery may prolong survival of patients with advanced cancer of the pancreas. Langenbecks Arch Surg 2007;392:55-60.
28 Pezzilli R, Casadei R, Calculli L, Santini D, Morselli Labate AM, on behalf of NeoPan Study Group. The Sant Orsola Algorithm for pancreatic cancer: an interim report. JOP 2006;7:546.
29 Dupont WD and Plummer WD. PS power and sample size program available for free on the Internet. Controlled Clin Trials.1997;18:274.
30 Date RS, Siriwardena AK. Radiofrequency ablation of the pancreas. II: Intra-operative ablation of non-resectable pancreatic cancer. A description of technique and initial outcome. JOP 2005;6:588-592.
31 Mornex F, Girard N, Delpero JR, Partensky C. Radiochemotherapy in the management of pancreatic cancer--part I:neoadjuvant treatment. Semin Radiat Oncol 2005;15:226-234.
32 Matsui Y, Nakagawa A, Kamiyama Y, Yamamoto K, Kubo N, Nakase Y. Selective thermocoagulation of unresectable pancreatic cancers by using radiofrequency capacitive heating. Pancreas 2000;20:14-20.
33 Tang Z, Wu YL, Fang HQ, Xu J, Mo GQ, Chen XM, et al. Treatment of unresectable pancreatic carcinoma by radiofrequency ablation with 'cool-tip needle': report of 18 cases. Zhonghua Yi Xue Za Zhi 2008;88:391-394.
34 Elias D, Baton O, Sideris L, Lasser P, Pocard M. Necrotizing pancreatitis after radiofrequency destruction of pancreatic tumours. Eur J Surg Oncol 2004;30:85-87.
35 Koninger J, Wente MN, Müller MW, Gutt CN, Friess H,Büchler MW. Surgical palliation in patients with pancreatic cancer. Langenbecks Arch Surg 2007;392:13-21.
36 Varshney S, Sewkani A, Sharma S, Kapoor S, Naik S, Sharma A, et al. Radiofrequency ablation of unresectable pancreatic carcinoma: feasibility, ef fi cacy and safety. JOP 2006;7:74-78.
37 Nishida K, Kaneko T, Yoneda M, Nakagawa S, Ishikawa T, Yamane E, et al. Doubling time of serum CA 19-9 in the clinical course of patients with pancreatic cancer and its signi fi cant association with prognosis. J Surg Oncol 1999;71:140-146.
BACKGROUND: Radiofrequency ablation (RFA) has been suggested as a new treatment option for patients with locally advanced cancer. This study aimed to prospectively evaluate the ef fi cacy and safety of intraoperative RFA in patients with unresectable, locally advanced, non-metastatic carcinoma of the pancreatic head.
METHODS: RFA was the fi rst step of the surgical procedure and was carried out on the mobilized pancreatic head followed by biliary by-pass and gastrojejunal-anastomosis. Intra- and post-operative morbidity and mortality, performance status,pain control, quality of life, and survival at 24 months were evaluated.
RESULTS: Seven patients (3 men and 4 women; median age 66 years, range 47-80 years) were studied and 4 were eligible for treatment. The RFA procedure was carried out in 3 of the 4 patients; in one patient it was not carried out because of the upstaging of the neoplasm. In all 3 patients RFA achieved complete necrosis of the lesion. A biliary fi stula developed 7 days after the procedure in one patient; all 3 patients developed ascites 8.6 days (range 7-9 days) on average after RFA. All patients died respectively, at 3, 4, and 5 months after the treatment.
CONCLUSIONS: In our experience, RFA is a feasible procedure,but it presents a very high rate of postoperative complications.Moreover, pain control, life quality and survival rate are poor.The few data suggest no impact on survival.
Author Af fi liations: Department of Surgery (Casadei R, Ricci C and Minni F), Department of Internal Medicine and Gastroenterology (Pezzilli R,Serra C and Morselli-Labate AM), Department of Radiology (Calculli L),and Department of Pathology (Santini D), S. Orsola-Malpighi Hospital,University of Bologna, Bologna, Italy
Raffaele Pezzilli, MD, Department of Internal Medicine and Gastroenterology, S. Orsola-Malpighi Hospital, University of Bologna, Via Massarenti n.9 40138, Bologna, Italy (Tel: +3905163641488;Fax: +390516364148; Email: raffaele.pezzilli@aosp.bo.it)
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
October 28, 2009
Accepted after revision April 6, 2010
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Gallbladder cancer with tumor thrombus in the superior vena cava
- Budd-Chiari syndrome secondary to caval recurrence of renal cell carcinoma
- Liver graft vascular variant with 3 extra-hepatic arteries
- An effective model for predicting acute kidney injury after liver transplantation
- Pancreas transplantation in the mouse
- Integrity of the pancreatic duct-acinar system in the pathogenesis of acute pancreatitis