Budd-Chiari syndrome secondary to caval recurrence of renal cell carcinoma
2010-12-14GabrieleMarangoniAdrianSullivanAmirAliWalidFarajandNigelHeaton
Gabriele Marangoni, Adrian O'Sullivan, Amir Ali, Walid Faraj and Nigel Heaton
London, UK
Budd-Chiari syndrome secondary to caval recurrence of renal cell carcinoma
Gabriele Marangoni, Adrian O'Sullivan, Amir Ali, Walid Faraj and Nigel Heaton
London, UK
(Hepatobiliary Pancreat Dis Int 2010; 9: 321-324)
inferior vena cava;renal cell carcinoma;recurrence;Budd-Chiari syndrome
Introduction
Tumor thrombus involving the inferior vena cava(IVC) is present in 4%-10% of patients with renal cell carcinoma (RCC).[1]The role of radical surgery in these patients is well established and 5-year survival can be achieved in 32%-64%.[2,3]
In more advanced cases, the thrombus may progress upwards to involve the ori fi ces of the hepatic veins causing Budd-Chiari syndrome (BCS), although only a small number of cases have been reported.[1,4]Surgery is currently the only treatment that can prevent progression to liver failure and death (Table).
Approximately one third of patients with RCC develop recurrent disease after surgery[5]and metastases are most common in the lungs, bones, liver, contralateral kidney, adrenals and brain. Other less common sites include the gastric wall, breast and pancreas and it seems that virtually all organs can potentially harbor metastatic renal cancer cells. We report surgical treatment of a case of RCC IVC recurrence presenting with BCS 7 years after radical nephrectomy.
Case report
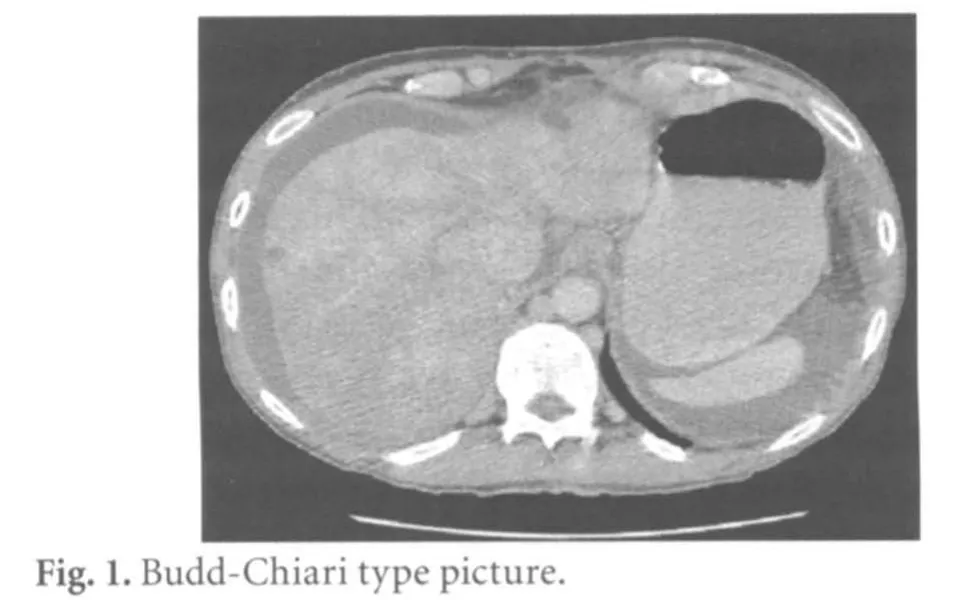
A 58-year-old man underwent a radical right nephrectomy for a locally advanced RCC in 2001. Six years later a CT scan showed a thrombosed infrahepatic IVC with extensive venous collaterals and an expanded retrohepatic IVC containing low attenuation material. A PET scan was normal and laparoscopy did not identify recurrence. A surveillance CT scan performed 8 months later con fi rmed a mass within the IVC which had grown and was now extending into the hepatic veins and the right atrium. Ascites was present with evidence of hepatic venous out fl ow obstruction, porto-caval shunting and patchy liver parenchyma enhancement compatible with a Budd-Chiari appearance. In addition,there were emboli in the pulmonary arteries (Fig. 1).Liver function tests were not grossly abnormal with bilirubin 16 μmol/l, ALP 145 U/L, AST 28 U/L, GGT116 U/L, albumin 42 g/dl, and INR 1.2. Child-Pugh score was A 6.
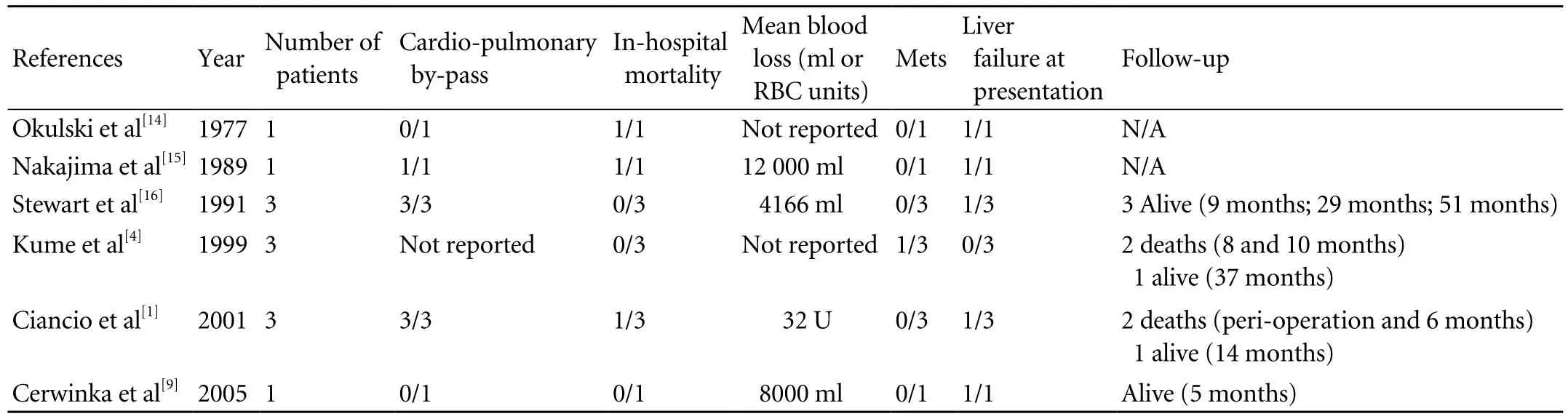
Table. Surgery for Budd-Chiari syndrome due to RCC
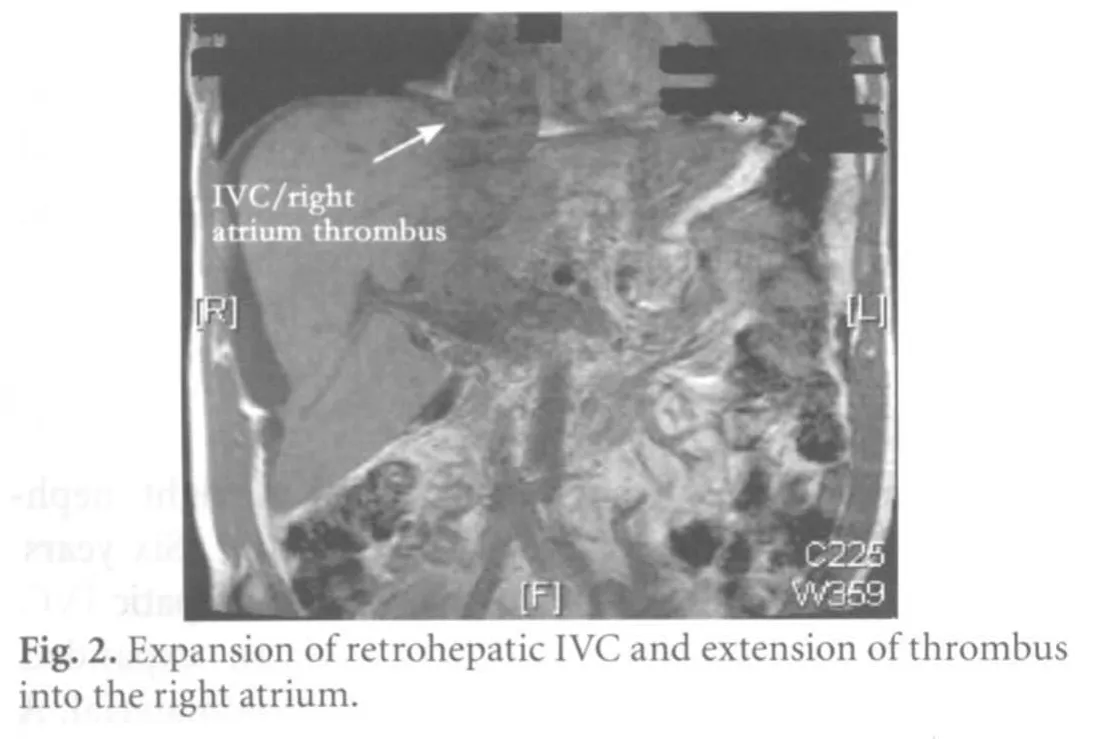
The patient was referred to our center for consideration of surgery. Pre-operative evaluation with transthoracic echocardiogram and liver magnetic resonance showed that the large mass in the right atrium seemed to involve the tricuspid valve (Fig. 2).
At surgery, access was gained with a Mercedes abdominal incision and a median sternotomy. There was ascites and clear features of venous out fl ow obstruction, more pronounced in the right lobe with extensive retroperitoneal collaterals. The IVC was completely occluded from the iliac veins to the right atrium. The right hepatic vein ori fi ce was completely occluded and the suprahepatic cava was also blocked by tumor thrombus. The distal cava was mobilized and the left renal vein was divided at a level free of tumor and anastomosed with the left gonadal vein. The right liver was mobilized with division of the coronary and triangular ligaments and the IVC was dissected off the liver with ligation and suture of the accessory hepatic veins.
Cardiopulmonary by-pass with cardioplegia was performed. Venous fl ow from the right femoral and inferior mesenteric veins was returned to the heart and the liver in fl ow controlled with the Pringle maneuver for a total of 50 minutes. The atrium was opened vertically and the tumor dissected free. The retrohepatic IVC and the extrahepatic right hepatic vein were resected, leaving a cuff of the hepatic veins free of the tumor. Vascular continuity was restored using a cuff of the cadaveric iliac vein sutured onto the hepatic veins and subsequently onto the right atrium.
Reperfusion was associated with signi fi cant bleeding from the chest requiring prolonged hemostasis with tissue sealants and blood products: overall blood loss was 33 600 ml and 32 units of packed red blood cells, 28 units of fresh frozen plasma, 5 pools of platelets, and 4 units of cryoprecipitate were infused. The abdomen was packed, the skin closed and the patient transferred to the Intensive Care Unit. The operative time was 11 hours. On post-operative day 2 the packs were removed and the abdomen was closed.
The immediate post-operative course was characterized by slow respiratory and vasopressor weaning.Three more units of red blood cells were transfused in the post-operative period. Atrial fi brillation was treated with amiodarone, and renal replacement therapy(hemo fi ltration) was required for 16 days. The patient was discharged to the surgical ward on post-operative day 17 and subsequently discharged home 38 days after surgery. At a 15-month follow-up the patient is alive with no evidence of recurrence.
Histology con fi rmed luminal occlusion of the IVC by clear cell renal carcinoma with focal but not transmural in fi ltration of the vein wall and resection margins free of tumor.
Discussion
Surgery is the only potentially curative treatment of primary and metastatic RCC. Survival does not appear to be different for RCC if the IVC or renal veins are in fi ltrated.[1]There is controversy regarding the prognostic signi fi cance of the level of thrombus in the IVC. Some studies suggest that extension of thrombus into the suprahepatic IVC is associated with reduced survival and increased risk of further metastasis.[6,7]A level IVC thrombus (extension to the right atrium)requires a combined abdominal-thoracic approach with cardio-pulmonary by-pass. This technique has a reported mortality of 8%-13%.[2,8]Cerwinka et al[9]reported a case of renal cancer invading the right atrial wall causing BCS which was resected without sternotomy. In this case the diaphragm was divided and the right atrium pulled below the diaphragm. The atrium and infrahepatic IVC were clamped and the tumor thrombus was removed. This was not possible in our case because the thrombus extended up to the tricuspid valve and open cardiac surgery with cardiopulmonary by-pass was necessary to dissect the tumor thrombus free from the right atrium. Expertise from liver transplantation and organ procurement was essential to planning and carrying out the surgery.[1,9]
To re-establish vascular continuity we used a blood group-compatible cuff of cadaveric iliac vein graft.Venous interposition cadaveric grafts were used in right lobe living donor liver transplantation to reconstruct the middle hepatic vein ori fi ce to overcome anterior segment congestion and occasionally for portal vein reconstruction in selected liver transplant recipients.IVC replacement was unnecessary as chronic venous obstruction had created spontaneous retroperitoneal collaterals.
Kume et al[4]reviewed 12 cases of BCS due to RCC thrombus and classi fi ed them into mild/silent and severe according to clinical manifestations. They concluded that in cases of mild/silent BCS, removal of the thrombus is effective and therefore surgery should be performed as a matter of urgency to avoid end-stage liver failure. Long-term survival can be achieved in these patients, although when there is severe disease, surgery is more challenging and is associated with a greater risk.[1,4,10]When surgery is not feasible, inevitably the progression is geared to fulminant liver failure.[11]
Surgery in the context of RCC with IVC tumor and widespread distant metastases has not produced good long-term survival results and is associated with high peri-operative mortality.[4]Patients with IVC involvement and an isolated pulmonary metastasis should be explored instead and a 5-year survival rate of 43% has been reported in combination with immunotherapy.[12,13]
BCS associated with extensive IVC RCC thrombus and atrium involvement should not be considered a contraindication to surgery, as long-term survival can be achieved if radical resection is possible. The surgery requires advanced liver and cardio-thoracic surgical expertise and is undoubtedly a major undertaking.Accurate pre-operative assessment and careful consideration of risk-bene fi t are therefore mandatory.
Funding: None.
Ethical approval: Not needed.
Contributors: MG wrote the fi rst draft and analyzed the data; OSA revised the draft; AA and WF collected data and literature search.HN approved the fi nal version and is the guarantor.
Competing interest: No bene fi ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Ciancio G, Soloway M. Renal cell carcinoma invading the hepatic veins. Cancer 2001;92:1836-1842.
2 Skinner DG, Pritchett TR, Lieskovsky G, Boyd SD, Stiles QR.Vena caval involvement by renal cell carcinoma. Surgical resection provides meaningful long-term survival. Ann Surg 1989;210:387-394.
3 Glazer AA, Novick AC. Long-term followup after surgical treatment for renal cell carcinoma extending into the right atrium. J Urol 1996;155:448-450.
4 Kume H, Kameyama S, Kasuya Y, Tajima A, Kawabe K.Surgical treatment of renal cell carcinoma associated with Budd-Chiari syndrome: report of four cases and review of the literature. Eur J Surg Oncol 1999;25:71-75.
5 Breda A, Konijeti R, Lam JS. Patterns of recurrence and surveillance strategies for renal cell carcinoma following surgical resection. Expert Rev Anticancer Ther 2007;7:847-862.
6 Sosa RE, Muecke EC, Vaughan ED Jr, McCarron JP Jr. Renal cell carcinoma extending into the inferior vena cava: the prognostic signi fi cance of the level of vena caval involvement. J Urol 1984;132:1097-1100.
7 Bissada NK, Yakout HH, Babanouri A, Elsalamony T, Fahmy W,Gunham M, et al. Long-term experience with management of renal cell carcinoma involving the inferior vena cava. Urology 2003;61:89-92.
8 Langenburg SE, Blackbourne LH, Sperling JW, Buchanan SA,Mauney MC, Kron IL, et al. Management of renal tumors involving the inferior vena cava. J Vasc Surg 1994;20:385-388.
9 Cerwinka WH, Ciancio G, Salerno TA, Soloway MS. Renal cell cancer with invasive atrial tumor thrombus excised off-pump.Urology 2005;66:1319.
10 Hatcher PA, Anderson EE, Paulson DF, Carson CC, Robertson JE. Surgical management and prognosis of renal cell carcinoma invading the vena cava. J Urol 1991;145:20-24.
11 Shih KL, Yen HH, Su WW, Soon MS, Hsia CH, Lin YM.Fulminant Budd-Chiari syndrome caused by renal cell carcinoma with hepatic vein invasion: report of a case. Eur J Gastroenterol Hepatol 2009;21:222-224.
12 Naitoh J, Kaplan A, Dorey F, Figlin R, Belldegrun A. Metastatic renal cell carcinoma with concurrent inferior vena caval invasion: long-term survival after combination therapy with radical nephrectomy, vena caval thrombectomy and postoperative immunotherapy. J Urol 1999;162:46-50.
13 Pantuck AJ, Zisman A, Belldegrun AS. The changing natural history of renal cell carcinoma. J Urol 2001;166:1611-1623.
14 Okulski TA, Soulen RL. Renal cell carcinoma presenting as the Budd-Chiari Syndrome. AJR Am J Roentgenol 1977;128:140-142.
15 Nakajima Y, Baba S, Nagahama T, Tazaki H. Renal cell carcinoma presenting as Budd-Chiari syndrome. Urol Int 1989;44:173-176.
16 Stewart JR, Carey JA, McDougal WS, Merrill WH, Koch MO, Bender HW Jr. Cavoatrial tumor thrombectomy using cardiopulmonary bypass without circulatory arrest. Ann Thorac Surg 1991;51:717-722.
BACKGROUND: Renal cell carcinoma (RCC) involves the inferior vena cava (IVC) in a minority of patients. Less commonly, it presents with Budd-Chiari syndrome. If untreated,the condition progresses towards liver failure and death.
METHOD: We report a case of Budd-Chiari syndrome due to in fi ltration of the IVC and right atrium by recurrence of RCC 7 years after successful treatment by primary resection.
RESULTS: Surgery was performed with a combined abdominal and thoracic approach with cardio-pulmonary by-pass and cardioplegia. The tumor was removed and a cadaveric iliac vein graft used to re-establish venous continuity between the right atrium and hepatic veins.
CONCLUSIONS: Although it is a complex and high-risk procedure, aggressive surgery performed by an experienced team with liver transplant and cardiothoracic skills may enable resection of apparently advanced caval tumors. The case is discussed in the light of the current literature.
Author Af fi liations: Institute of Liver Studies, King's College London School of Medicine at King's College Hospital, Denmark Hill, London SE5 9RS, UK (Marangoni G, O'Sullivan A, Ali A, Faraj W and Heaton N)
Gabriele Marangoni, MD, Institute of Liver Studies,King's College Hospital, Denmark Hill, SE5 9RS, London, UK (Tel:+442032993672; Fax: +442032993575; Email: gabrielemarangoni@virgilio.it)© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
July 13, 2009
Accepted after revision December 1, 2009
Life is not merely enjoyment but also laborious work.
— Leo Nikolayevich Tolstoy
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Gallbladder cancer with tumor thrombus in the superior vena cava
- A prospective study on radiofrequency ablation locally advanced pancreatic cancer
- Liver graft vascular variant with 3 extra-hepatic arteries
- An effective model for predicting acute kidney injury after liver transplantation
- Pancreas transplantation in the mouse
- Integrity of the pancreatic duct-acinar system in the pathogenesis of acute pancreatitis