Endoscopic retrograde cholangiopancreatography outcome from a single referral center in Iran
2010-12-14AmirMohammadAlizadehEsmaeilAfzaliMirhadiMousaviYaghoubMoaddabandMohammadZali
Amir H Mohammad Alizadeh, Esmaeil S Afzali, Mirhadi Mousavi,Yaghoub Moaddab and Mohammad R Zali
Tehran, Iran
Endoscopic retrograde cholangiopancreatography outcome from a single referral center in Iran
Amir H Mohammad Alizadeh, Esmaeil S Afzali, Mirhadi Mousavi,Yaghoub Moaddab and Mohammad R Zali
Tehran, Iran
(Hepatobiliary Pancreat Dis Int 2010; 9: 428-432)
endoscopy;outcome;diagnosis;complication;pancreatitis
Introduction
Patients with suspected pancreaticobiliary disorders require diagnostic evaluation of the pancreaticobiliary tree to establish the correct diagnosis. This assessment frequently includes imaging to fi nd the presence of dilation or narrowing of the ducts and to determine the probable etiologies of such morphological changes.[1]Endoscopic retrograde cholangiopancreatography (ERCP) is an accurate diagnostic tool for assessing these changes. The available evidence suggests that ERCP is the fi rst choice for diagnostic evaluation of the pancreatic and biliary tree that can be accompanied by a high diagnostic sensitivity and a low therapeutic outcome.[2]ERCP is helpful in diagnosing and treating choledocholithiasis, benign and malignant biliary strictures,operative and traumatic ductal injuries, and sphincter of Oddi dysfunction. However, this diagnostic techniquemay lead to potential complications, even post-ERCP mortality, which should be reduced by avoidance of its unnecessary use.[3,4]ERCP-related complications can be broadly divided into short-term (within 3 days of the procedure) and long-term. Short-term complications are generally sedation- and/or endoscopy-related, and include bleeding, infection, perforation, and cardiopulmonary events, whereas long-term complications mainly include infections associated with indwelling stents and in fl ammatory changes secondary to ductal manipulation.[5,6]
Reported ERCP outcomes of populations from developed and developing countries have been widely different, mainly depending on the complexity of the procedure, the underlying diagnosis, and patient comorbidities. To determine the success rate and outcome of ERCP, comparative studies of ERCP diagnostic approaches in each population are required. In the current study, we described the indications, fi ndings,and technical success of ERCP in a population of Iranians admitted to our referral center.
Methods
In a retrospective review database-based study, 780 patients (393 males and 387 females; mean age 57.5 years, range 15-99 years) who had undergone diagnostic and therapeutic ERCP with a primary diagnosis of hepatobiliary disorders between 2006 and 2008 at Taleghani Hospital in Tehran were reviewed. In patients with invasive cancers including pancreatic ductal adenocarcinoma, biliary carcinoma, metastastic tumor with biliary obstruction, hepatocellular carcinoma, and ampullary carcinoma, 105 procedures (13.5%) were performed, whereas in patients with benign in fl ammatory diseases, 313 procedures (40.1%) were done to con fi rm bile duct stones. The patients excluded from this study were those with a history of biliary sphincterotomy, a history of pre-cut sphincterotomy, pre-procedure active pancreatitis, pregnancy, mental disability, and refusal to participate in. The patients who had a history of previous BillrothⅡ gastrectomy were also excluded.[7]
The major data of the enrolled patients were demographic characteristics, clinical information, laboratory parameters, and post-ERCP complications. The demographic characteristics, clinical information, and technical details and fi ndings from an ERCP performed in these patients were prospectively recorded in a special database. The initial liver function tests during emergency admission were used as the screening tests for ERCP.Laboratory parameters were measured on admission.Serum amylase was measured 30 minutes before and 3 hours after ERCP. Cannulation was attempted by using a sphincterotomy. Complications including post-ERCP pancreatitis, gastrointestinal perforation, and bleeding seen during or after the procedure were recorded.
Statistical analysis
All the statistical analyses were performed using SPSS version 16.0 for Windows (SPSS Inc., Chicago, IL., USA).Results were expressed as the mean±standard deviation(SD) for quantitative variables and percentages for categorical variables. Categorical variables were compared using the Chi-square test or Fisher's exact test.Continuous variables were compared by independent samples t test for variables with normal distributions and the Mann-Whitney U test for variables with nonnormal distributions. P values of 0.05 or less were considered statistically signi fi cant.
Results
The current study presented a population-based report of diagnostic and therapeutic ERCP at a referral center in Iran. Baseline characteristics and medical history are shown in Table 1. Cholecystectomy was performed in about one-third of the 780 patients and 80 patients had a history of biliary stone.
A minority of the patients had hepatobiliary carcinomas, and 1 had cirrhosis. Laboratory examination showed pre-ERCP AST >250 mg/dl in 39 patients and serum ALT >250 mg/dl in 65 (Table 2). The medianAST and ALT values were 55.0 and 62.0 U/L respectively.The serum concentration of amylase was reduced in 42 patients (5.4%), whereas it was increased more than two times in 152 patients (19.5%). The most common clinical manifestations in patients undergoing diagnostic ERCP were icterus (47.3%), weight loss (31.2%), and dark urine (26.9%). Diarrhea and hepatosplenomegaly were rarely seen (Table 3).
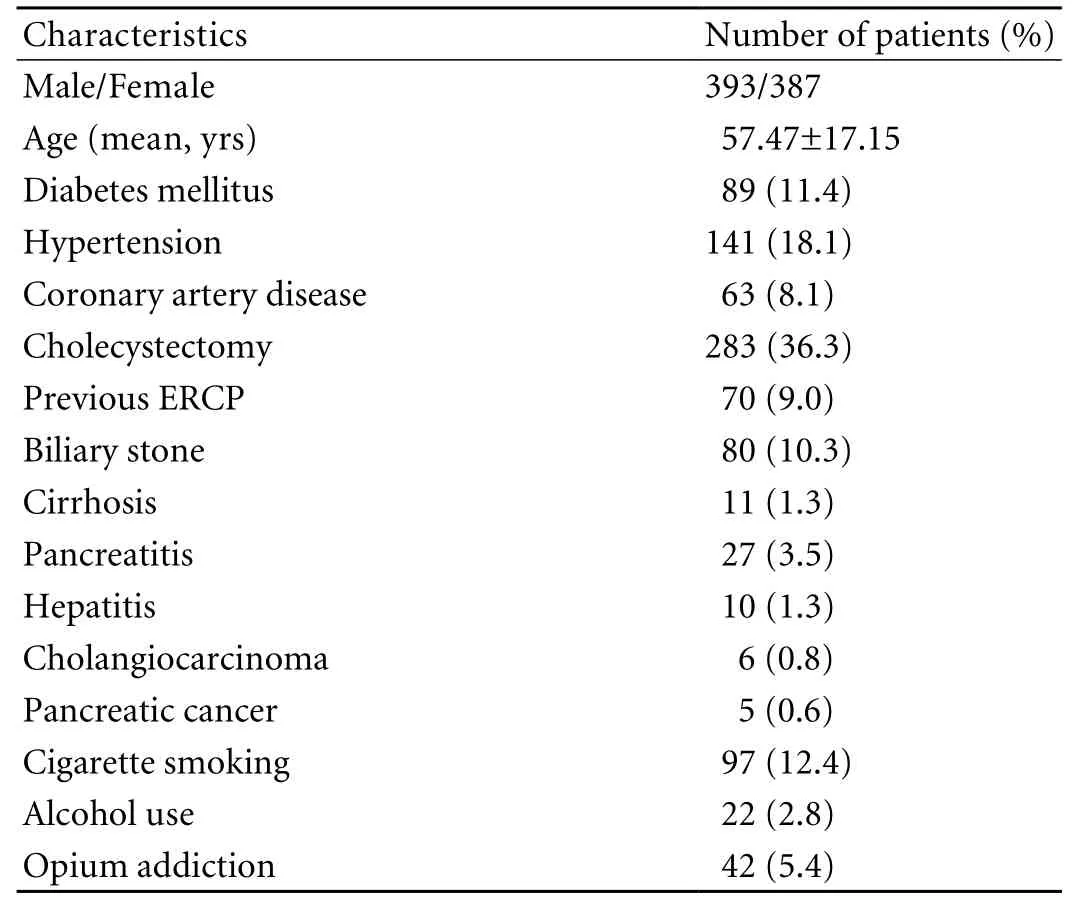
Table 1. Baseline characteristics and medical history of the 780 patients receiving diagnostic ERCP
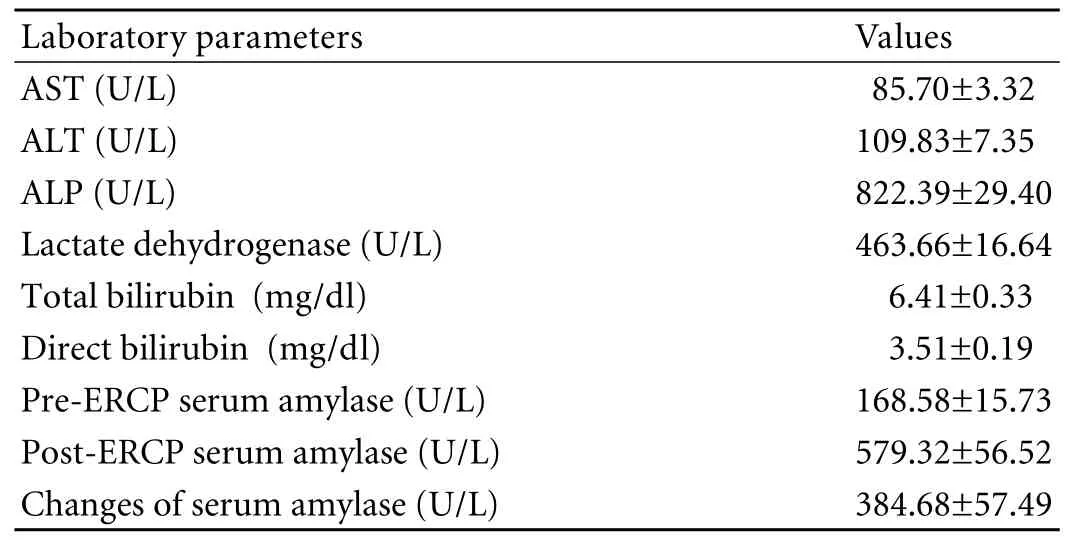
Table 2. Pre-ERCP laboratory parameters in the 780 patients undergoing ERCP
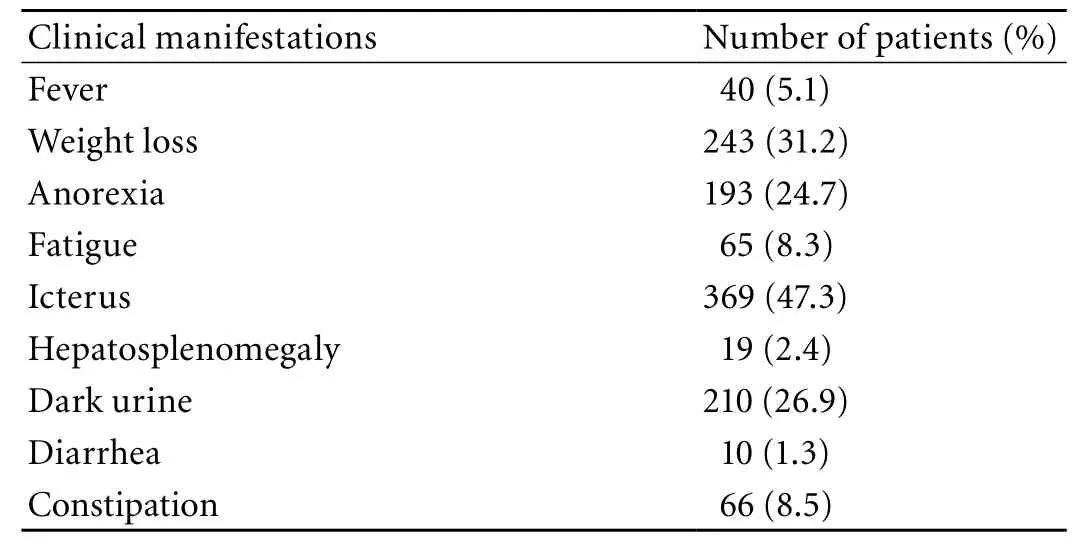
Table 3. Clinical manifestations in the 780 patients undergoing ERCP
Selective biliary cannulation was technically successful in 87.0% of all patients; however, it failed in 13.0%.The most frequent indications for diagnostic ERCP were choledocholithiasis (71.9%), suspected sphincter of Oddi dysfunction (14.7%), and different types of hepatobiliary malignancy (12.6%). The most frequent fi nal diagnosis of ERCP was common bile duct stone that was detected in 313 (40.1%) patients, and 16 had synchronous gallbladder stones. Common bile duct stricture and primary sclerosing cholangitis occurred in 52 (6.7%) and 27 patients (3.5%), respectively. However,the ERCP results in 11.0% of our patients were normal.Normal ERCP results were encountered more frequently in women than in men (13.7% versus 8.4%, P<0.05).Normal ERCP results were observed more often in patients below 70 years than in the older ones (13.4%versus 5.0%, P<0.05).
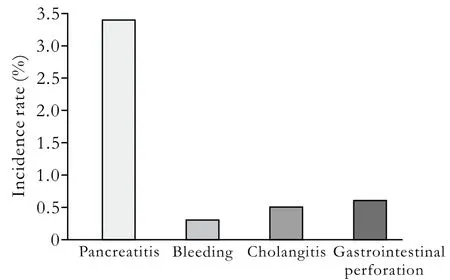
Fig. 1. The incidence rate of post-ERCP complications in all patients.
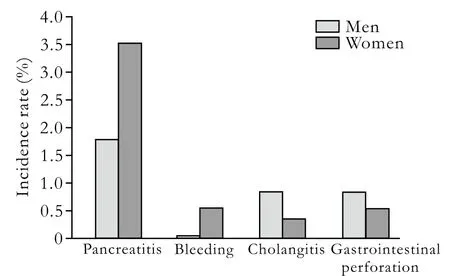
Fig. 2. The incidence rate of post-ERCP complications in men and women.
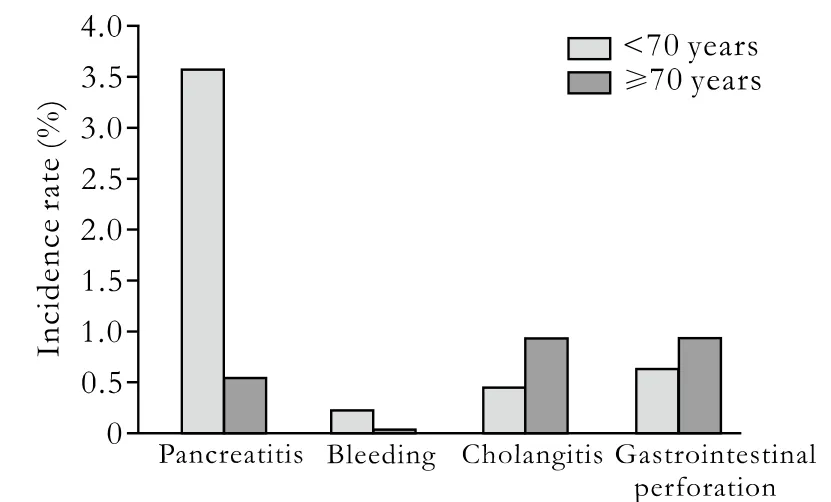
Fig. 3. The incidence rate of post-ERCP complications in patients less than 70 years old and the elderly.
Successful stenting was performed in 43 (15.2%) of our patients. Stent was placed more frequently in men than in women (21.5% versus 8.2%, P<0.001). It was placed in patients of 70 years old more than in younger ones (18.8% versus 13.4%, P=0.056). In post-ERCP complications, pancreatitis was predominant with an incidence rate of 3.3% (Fig. 1). Other complications including local bleeding, cholangitis and gastrointestinal perforation, rarely occurred. The incidence rate of post-ERCP pancreatitis was 1.8% in men and 3.6% in women(Fig. 2). Although the incidence of pancreatitis was numerically higher in women, this difference was not statistically signi fi cant (P=0.120). The incidence rate of other post-ERCP complications were also comparable in both genders. In different age subgroups (Fig. 3),the incidence of pancreatitis was higher in younger patients than in the older ones (3.6% versus 0.5%;OR: 8.216, P=0.015). However, the incidences of other complications were similar in the two age subgroups.
Discussion
In the current study we investigated diagnostic ERCP approaches used in Iranians with a fi nal diagnosis of hepatobiliary disease at a referral center in Iran.In this study clinical disorders were comparable in both genders. Bile duct cannulation was successfully performed in the patients except 13% of them. In the patients with cholelithiasis revealed by ERCP, 2.6% had malignancies. Pancreatitis was the most common post-ERCP complication and other complications were rarely seen. The overall prevalence of post-ERCP pancreatitis in our study was less than 6.0%, which was within the range of other similar studies (4.0%-10.0%).[8-16]Also,according to the reported rate of successful cannulation(63% to 94%), the rate in our study was acceptable.Although we did not observe any post-ERCP early mortality, but the early mortality in other studies was to incidence of pancreatitis was similar in men and women.Age as a patient-related predictor was found to be signi fi cant in some studies.[21,22]Besides, female gender and young age have been identi fi ed as risk factors for the development of post-ERCP pancreatitis.[18]In two different studies, nearly all of the patients who developed severe or fatal pancreatitis were young to middle-aged women with recurrent abdominal pain, normal serum bilirubin level, and no biliary obstructive pathology.[23]Therefore, it is recommended that in younger women,diagnostic ERCP should be avoided in routine practice and magnetic resonance cholangiopancreatography or detailed CT imaging should be used instead.
In conclusion, ERCP indications, fi nal diagnosis,and related complications are comparatively consistent with those reported in other countries. Pancreatitis is the most common post-ERCP complication, and young age is a potential determinant of post-ERCP pancreatitis.1.6%.[10, 13-16]
Pancreatitis is the most common event after ERCP,which has been con fi rmed by other studies.[14-16]Patients with this complication usually present with mild symptoms and signs. The reported incidences of pancreatitis vary widely from 1% to 40%, which are potentially in fl uenced by different diagnostic criteria of pancreatitis, methods of data collection, and patient populations. The severity of pancreatitis ranges from a minor inconvenience with one or two days of hospitalization with full recovery to a devastating illness with pancreatic necrosis, multiorgan failure, permanent disability, and even death. Most episodes of post-ERCP pancreatitis are mild and approximately 10% of patients may develop moderate or severe pancreatitis.[17-19]Thus post-ERCP pancreatitis should be suspected in any patient who develops pain within 6 hours after the procedure since it is much less likely to develop after 12 hours. Post-ERCP pain with marked elevation of serum amylase and/or lipase levels, especially when the values are greater than 1000 IU/L, is strongly suggestive of pancreatitis. In case of diagnostic doubt, especially when severe pancreatitis is predicted, radiological imaging should con fi rm the diagnosis.[20]
Apart from pancreatitis that was more prevalent in the younger patients, other complications were comparable between the two age groups in our study. However, the
Funding: None.
Ethical approval: Not needed.
Contributors: MAAH proposed the study and wrote the fi rst draft. AES analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. ZMR is the guarantor.
Competing interest: No bene fi ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA, et al. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc 2005;62:1-8.
2 Jaik NP, Hoey BA, Stawicki SP. Evolving role of endoscopic retrograde cholangiopancreatography in management of extrahepatic hepatic ductal injuries due to blunt trauma:diagnostic and treatment algorithms. HPB Surg 2008;2008:259141.
3 Mallery JS, Baron TH, Dominitz JA, Goldstein JL, Hirota WK, Jacobson BC, et al. Complications of ERCP. Gastrointest Endosc 2003;57:633-638.
4 Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M,et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol 2001;96:417-423.
5 Kozarek RA, Ball TJ, Patterson DJ. Endoscopic approach to pancreatic duct calculi and obstructive pancreatitis. Am J Gastroenterol 1992;87:600-603.
6 Baron TH, Petersen BT, Mergener K, Chak A, Cohen J, Deal SE, et al. Quality indicators for endoscopic retrograde cholan giopancreatography. Gastrointest Endosc 2006;63:S29-34.
7 Karamanolis G, Katsikani A, Viazis N, Stefanidis G,Manolakopoulos S, Sgouros S, et al. A prospective cross-over study using a sphincterotome and a guidewire to increase the success rate of common bile duct cannulation. World J Gastroenterol 2005;11:1649-1652.
8 Laukkarinen J, Nordback I, Mikkonen J, Kärkkäinen P, Sand J. A novel biodegradable biliary stent in the endoscopic treatment of cystic-duct leakage after cholecystectomy.Gastrointest Endosc 2007;65:1063-1068.
9 Andriulli A, Loper fi do S, Napolitano G, Niro G, Valvano MR,Spirito F, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol 2007;102:1781-1788.
10 Cheng CL, Fogel EL, Sherman S, McHenry L, Watkins JL,Crof fi e JM, et al. Diagnostic and therapeutic endoscopic retrograde cholangiopancreatography in children: a large series report. J Pediatr Gastroenterol Nutr 2005;41:445-453.
11 Ciriza C, Dajil S, Jiménez C, Urquiza O, Karpman G,García L, et al. Five-year analysis of endoscopic retrograde cholangiopancreatography in the Hospital del Bierzo. Rev Esp Enferm Dig 1999;91:693-702.
12 Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc 2009;70:80-88.
13 Farrell RJ, Mahmud N, Noonan N, Kelleher D, Keeling PW.Diagnostic and therapeutic ERCP: a large single centre's experience. Ir J Med Sci 2001;170:176-180.
14 Güitrón-Cantú A, Adalid-Martínez R, Gutiérrez-Bermúdez JA, Nieves-Rentería A, Alvarez-Valdés G. Complications in diagnostic and therapeutic endoscopic cholangiopancreatogr aphy. Prospective study. Rev Gastroenterol Mex 2007;72:227-235.
15 Loper fi do S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study.Gastrointest Endosc 1998;48:1-10.
16 Ong TZ, Khor JL, Selamat DS, Yeoh KG, Ho KY.Complications of endoscopic retrograde cholangiography in the post-MRCP era: a tertiary center experience. World J Gastroenterol 2005;11:5209-5212.
17 Murray WR. Reducing the incidence and severity of post ERCP pancreatitis. Scand J Surg 2005;94:112-116.
18 Cheng CL, Sherman S, Watkins JL, Barnett J, Freeman M,Geenen J, et al. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol 2006;101:139-147.
19 Fazel A, Quadri A, Catalano MF, Meyerson SM, Geenen JE.Does a pancreatic duct stent prevent post-ERCP pancreatitis?A prospective randomized study. Gastrointest Endosc 2003;57:291-294.
20 Badalov N, Tenner S, Baillie J. The Prevention, recognition and treatment of post-ERCP pancreatitis. JOP 2009;10:88-97.21 Maldonado ME, Brady PG, Mamel JJ, Robinson B. Incidence of pancreatitis in patients undergoing sphincter of Oddi manometry (SOM). Am J Gastroenterol 1999;94:387-390.
22 Mehta SN, Pavone E, Barkun JS, Bouchard S, Barkun AN.Predictors of post-ERCP complications in patients with suspected choledocholithiasis. Endoscopy 1998;30:457-463.
23 Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med 1996;335:909-918.
BACKGROUND: Endoscopic retrograde cholangiopancreatography (ERCP) is the fi rst choice for diagnostic evaluation of the pancreatic and biliary tree and can be accompanied by a high diagnostic sensitivity and a poor therapeutic outcome.In the current study, we described our experiences in the indications, fi ndings, and technical success of ERCP in a sample of the Iranian population admitted to a referral center in Iran.
METHODS: In a retrospective review database-based study,780 patients (393 males and 387 females; mean age 57.5 years)who had undergone diagnostic and therapeutic ERCP with the primary diagnosis of hepatobiliary disorder between 2006 and 2008 at Taleghani Hospital in Tehran were reviewed. The key data were demographic characteristics, clinical information,laboratory parameters, as well as post-ERCP complications.
RESULTS: A history of cholecystectomy was found in about one-third (36.3%) of participants and 80 (10.3%) out of 780 patients had a previous history of biliary stone. A minority (1.4%) of the patients suffered from hepatobiliary carcinomas, and 11 patients had cirrhosis. The most common clinical manifestations in the patients undergoing diagnostic ERCP were icterus (47.3%), weight loss (31.2%), and dark urine (26.9%). Selective biliary cannulation was technically successful in 87.0% of the patients; however, cannulation failed in 13.0%. The most frequent fi nal diagnosis of ERCP was common bile duct stone that was detected in 40.1% of the patients. The ERCP results in 11.0% of the patients were normal. Regarding appropriate treatment, successful stenting was performed in 43 patients (15.2%). Among post-ERCP complications, pancreatitis was the most adverse event with an incidence rate of 3.3%. Other complications including local bleeding, cholangitis and gastrointestinal perforation, rarely occurred. Post-ERCP pancreatitis was reported in 1.8% of men and 3.6% of women (P=0.120). Pancreatitis was more common in women below 70 years than in those who were older than 70 years (3.6% versus 0.5%; OR: 8.216, P=0.015). This might be due to the more functionally active pancreas in younger women than in the older ones. However, other complications were similar in the two age groups.
CONCLUSIONS: Based on our experience, ERCP indications,fi nal diagnosis and related complications are comparatively consistent with those reported in other countries. The most common post-ERCP complication is pancreatitis that is more often observed in younger patients.
Author Af fi liations: Shahid Beheshti University of Medical Sciences,Taleghani Hospital, Parvaneh Ave., Tabnak Str., Evin, Tehran, Iran-19857(Mohammad Alizadeh AH, Afzali ES, Mousavi M, Moaddab Y and Zali MR)Corresponding Author: Amir H Mohammad Alizadeh, Shahid Beheshti University of Medical Sciences, Taleghani Hospital, Parvaneh Ave., Tabnak Str., Evin, Tehran, Iran-19857, P.O. Box: 19835-178 (Tel: 0098-21-22432521;Fax: 0098-21-22432517; Email: ahmaliver@yahoo.com)
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
March 10, 2010
Accepted after revision June 5, 2010
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Pancreatic duct stones in patients with chronic pancreatitis: surgical outcomes
- Methylprednisolone inhibits activated CD4+ T cell survival promoted by toll-like receptor ligands
- Endoscopic management of postcholecystectomy biliary leakage
- Magnetic resonance imaging-guided percutaneous cryoablation of hepatocellular carcinoma in special regions
- Radiofrequency ablation, heat shock protein 70 and potential anti-tumor immunity in hepatic and pancreatic cancers: a minireview
- Application of a medical image processing system in liver transplantation
