Endoscopic management of postcholecystectomy biliary leakage
2010-12-14VirendraSinghGurpreetSinghGangaVermaandRajeshGupta
Virendra Singh, Gurpreet Singh, Ganga R Verma and Rajesh Gupta
Chandigarh, India
Endoscopic management of postcholecystectomy biliary leakage
Virendra Singh, Gurpreet Singh, Ganga R Verma and Rajesh Gupta
Chandigarh, India
(Hepatobiliary Pancreat Dis Int 2010; 9: 409-413)
biliary fi stulae;endoscopic retrograde cholangiopancreatography;sphincterotomy;biliary stent;nasobiliary drain;biliary strictures
Introduction
Biliary injuries continue to be a signi fi cant problem following open or laparoscopic cholecystectomy,[1,2]liver transplant,[3]trauma[4]or infection.[5,6]Traditionally, surgery has been the gold standard for the management of biliary injuries. Recently, various endoscopic methods have been used as the preferred modalities of these patients.[4,7-12]Various classi fi cations have been proposed to help manage the injuries of these patients.[8,13]However, optimal endoscopic intervention is not well established. We retrospectively evaluated the effect of endoscopic methods in the management of postcholecystectomy biliary leaks and suggested an algorithm for the management of the injuries.
Methods
We retrospectively evaluated 85 patients with postcholecystectomy biliary leaks between July 2000 to March 2009. Various parameters including clinical features, type of cholecystectomy, interventions and outcome were recorded. Diagnosis of biliary leak was based on bilious abdominal drain or endoscopic retrograde cholangiopancreatography (ERCP). All patients were given antibiotics before ERCP until 5 days after the procedure. ERCP was done to identify the leak site and therapeutic interventions were done suchas sphincterotomy, biliary stenting, and nasobiliary drainage (NBD). The stents were removed after 6-8 weeks. NBD was removed after closure of the leak on cholangiography.
Statistical analysis was performed using Student's t test and the Chi-square test. A P value of less than 0.05 was considered statistically signi fi cant.
Results
Eighty- fi ve patients with postcholecystectomy biliary leaks were treated from July 2000 to March 2009. The mean age of these patients was 42.47±11.48 years(range 20 to 80 years) and there were 65 females and 20 males. Fifty-two (61%) patients had undergone open,whereas the remaining 33 (39%) had had laparoscopic cholecystectomy. The various symptoms and signs are listed in Table 1. The mean time to presentation following cholecystectomy was 17.28±16.21 days (range 1 to 90 days). Presenting symptoms included abdominal pain in 46 patients (54.1%), fever in 23 (27.1%), abdominal distension in 42 (49.4%) and jaundice in 23 (27.1%).Bilious abdominal drain was present in 67 (78.8%)patients. ERCP detected a leak from the cystic duct in 45 patients (Fig. 1A), stricture with a middle-common bile duct (CBD) leak in 4, leak from the right hepatic duct in 3,and ligated CBD in 32 (Fig. 1B, Table 2). Twelve patients also had bile duct stones. One had a broken T-tube with a leak at the site with stones (Fig. 1C).
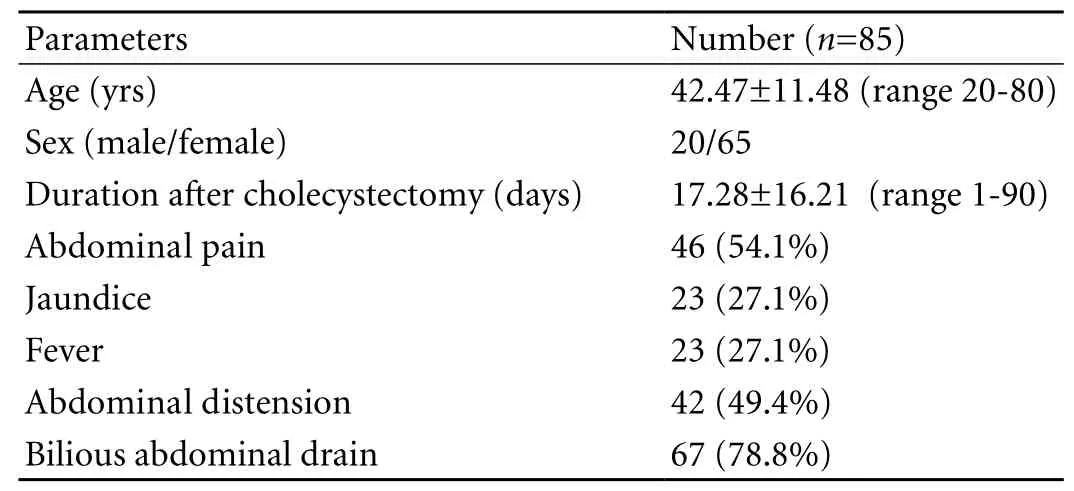
Table 1. Clinical fi ndings of 85 patients with biliary leaks
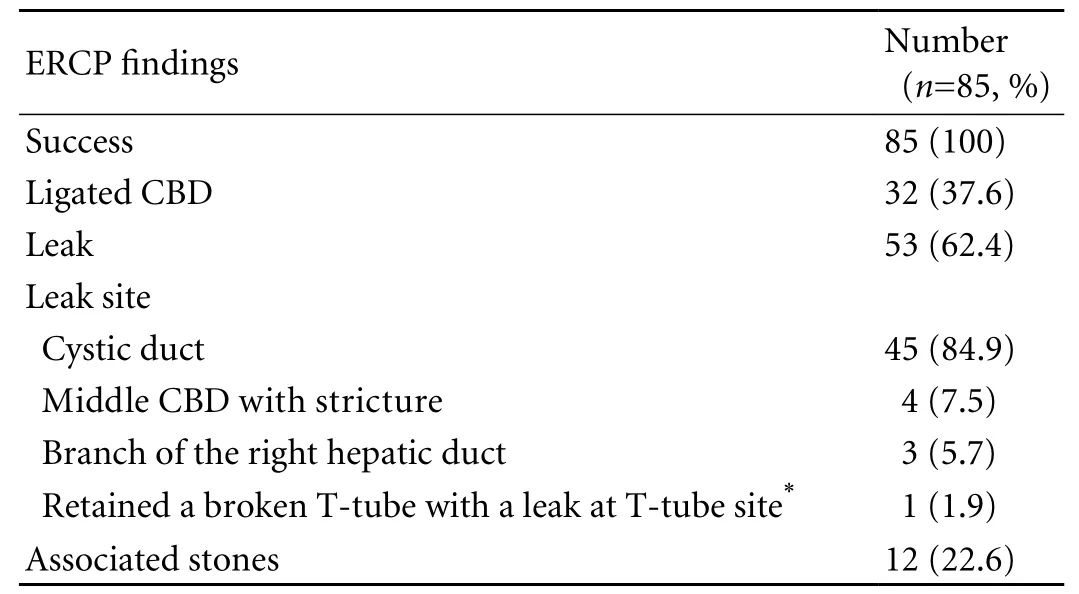
Table 2. ERCP fi ndings in patients with biliary leaks (%)
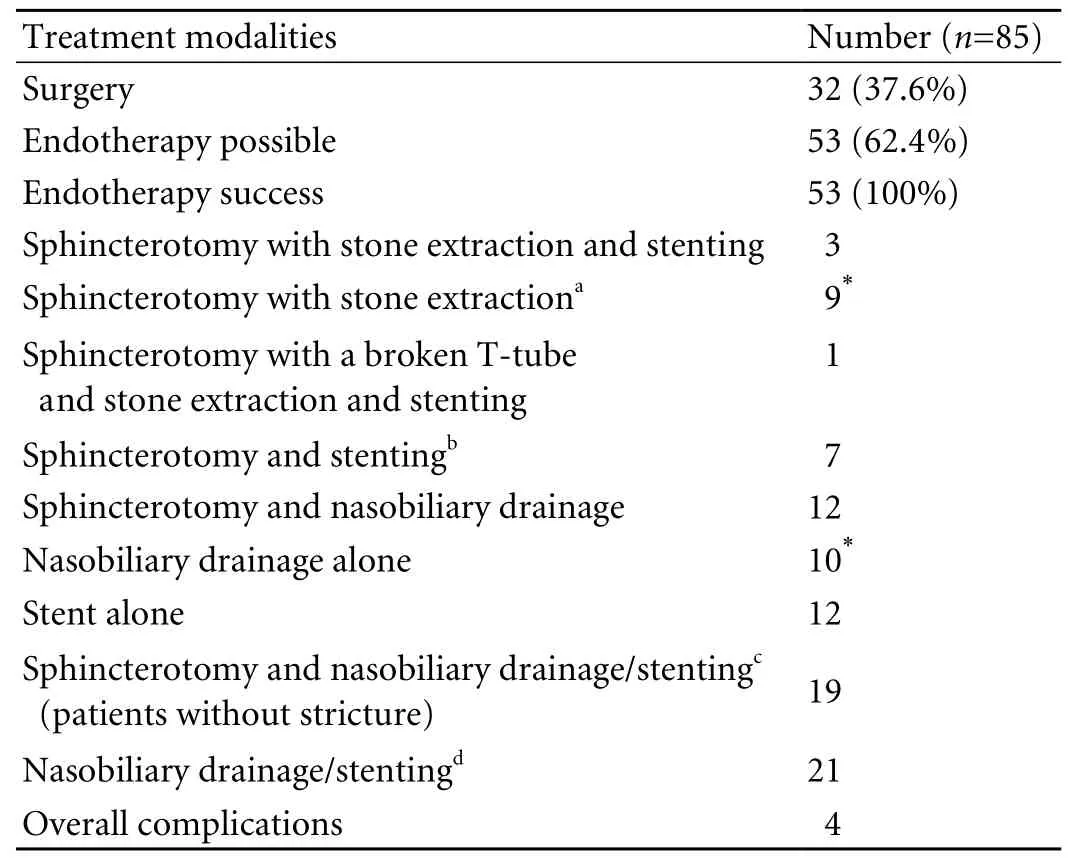
Table 3. Treatment modalities in patients with biliary leaks
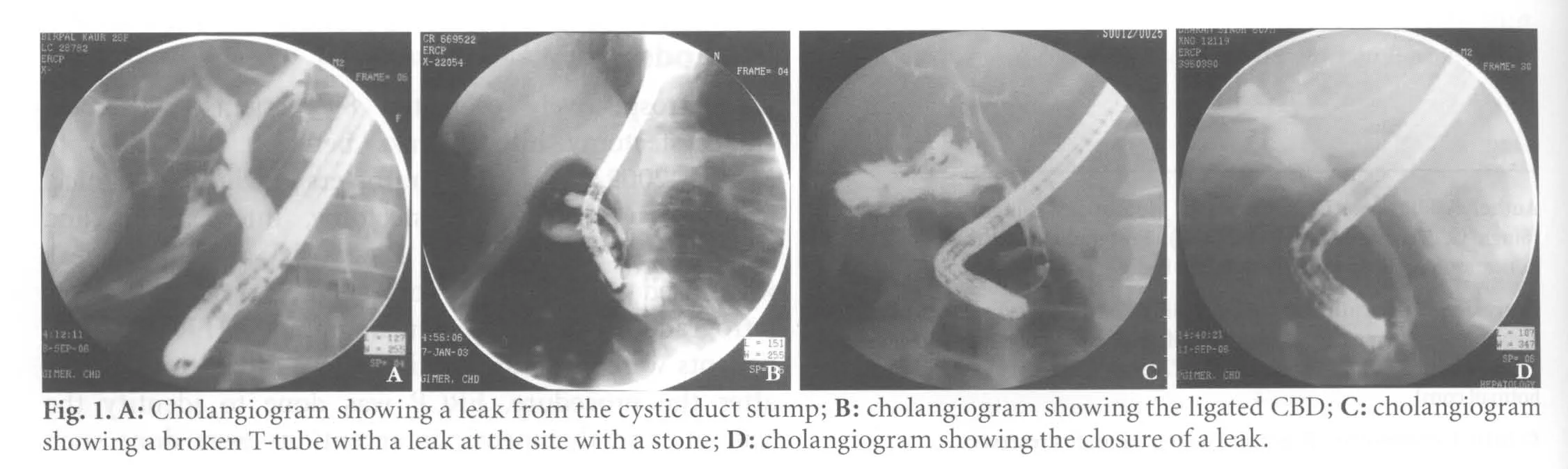
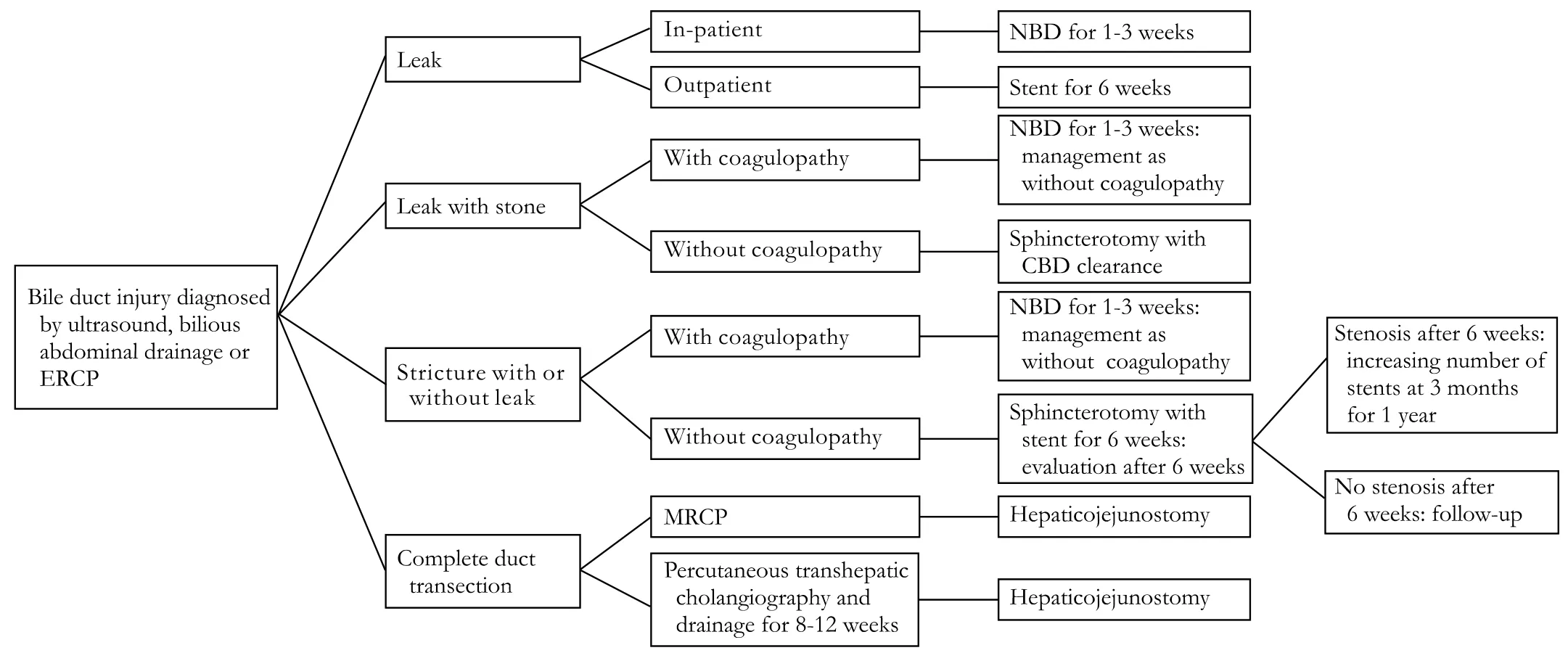
Fig. 2. Algorithm for the management of postcholecystectomy biliary injuries.
Endotherapy was possible in 53 patients, and 32 patients with ligated CBD underwent surgery (Table 3).Three patients with stones, one with a broken T-tube with stones, and four with stricture of the CBD with a leak were managed with sphincterotomy and stenting. Eight patients with a cystic duct stump leak with stone were managed with sphincterotomy and stone extraction. Three out-patients with a cystic duct stump leak were managed with sphincterotomy and stenting. Twelve patients with a cystic duct stump leak admitted to hospital were managed with sphincterotomy and NBD. Five patients with a cystic duct stump leak were managed with a stent. Sixteen had coagulopathy, hence sphincterotomy could not be done and they were managed with NBD only (9) or stenting (7). One patient with a cystic duct stump leak with stone and coagulopathy was initially managed with NBD for 2 weeks for the biliary leak and underwent sphincterotomy and stone extraction later. Leak closure were achieved in 100% patients (Fig. 1D). Stent/NBD with or without sphincterotomy was equally effective in the management of postcholecystectomy biliary leaks(Table 3). Mild pancreatitis occurred in 4 patients who were managed conservatively.
Discussion
Endoscopic interventions have essentially replaced surgery as fi rst-line treatment for most of the biliary injuries following cholecystectomy. Bile duct injury has been classi fi ed into 4 types: type A, cystic duct leaks or leakage from aberrant or peripheral hepatic radicles; type B, major bile duct leaks with or without concomitant biliary strictures; type C, bile duct strictures without bile leakage; and type D, complete transection of the bile duct with or without excision of some portion of the biliary tree.[8]Another group proposed classifying leaks into low grade and high grade, depending on when the leak was identi fi ed during contrast injection.[13]Bile leaks seen only after opaci fi cation of intrahepatic biliary branches were considered low grade, while those seen prior to intrahepatic duct opaci fi cation were de fi ned as high grade. This grading system was used as an objective re fl ection of leak severity and to guide therapy.
Various methods such as long or short stents and NBD with or without sphincterotomy have been used to facilitate biliary drainage and leak closure in patients with postcholecystectomy biliary leaks[7,10,14]at a median interval of 3 days (range 3-16 days) after endoscopic intervention.[15]These methods decrease or eliminate the pressure gradient between the bile duct and duodenum,[10]allowing preferential fl ow of bile from the duct into the duodenum instead of extravasation via the leak, and allowing the defect to heal. Endoscopic sphincterotomy is an established procedure but carries a risk of early or late complications. Foutch et al[7]treated 23 patients with biliary leak with sphincterotomy alone, sphincterotomy with stenting, stenting alone, and sphincterotomy with NBD. All patients improved and stents were removed at an average of 8 weeks. Endoscopic biliary sphincterotomy alone was described to effectively treat 22 of 25 patients(88%) with postoperative leaks in one report.[16]Marks et al[17]reported early fi stula closure in dogs with stent alone compared with sphincterotomy alone. We treated 20 patients with traumatic hepatobiliary injuries and biliary leaks with sphincterotomy with NBD (13) or NBD alone (7) and showed that NBD alone is as effective as NBD with sphincterotomy in managing these leaks.[4]Recently, Kaffes et al[11]treated endoscopically 96 of 100 patients with biliary leak. The endoscopic procedures included stenting alone (40), sphincterotomy alone (18)and combination of stenting and sphincterotomy (31),and advocated temporary insertion of a biliary stent without sphincterotomy as the optimal endoscopic intervention for patients with postcholecystectomy biliary leak.[11]
NBD and plastic biliary stents effectively treat leaks in more than 85% of cases.[10,18-21]NBD has the potential advantages of maintaining access for repeat cholangiography to con fi rm leak closure and not requiring a second endoscopic procedure for their removal. However, the presence of nasobiliary catheters can be irritating to patients, alterations of patient position may lead to accidental dislodgment from the biliary tree, and they deprive the patients of a signi fi cant proportion of their bile. Biliary stenting seems to be the preferred method of endoscopic treatment at many centers.[10,19,20]Some studies advocate the use of "leak-bridging" stents, when possible, to traverse the site of the defect.[20]However, shorter stents that just traverse the papilla and improve transpapillary bile fl ow appear equally effective for most leaks.[10]Biliary stenting requires repeat endoscopy for removal, and this is usually performed 4 to 8 weeks after initial placement. Stenting has the advantages of technical simplicity and preservation of the biliary sphincter. In addition, stenting is safe in patients with coagulopathy and is an effective therapy for those with concomitant postoperative bile duct strictures. Sandha et al[13]treated low-grade leaks with sphincterotomy alone (91%success), and high-grade leaks with stenting with or without sphincterotomy (100% success). In our study,the addition of sphincterotomy to stenting/NBD did not provide any extra bene fi t, and the complications of sphincterotomy could be avoided. In the present study, one patient had a broken T-tube with a leak at the site with stone. Breakage of a T-tube during its removal is rarely seen.[22]We have only come across a few case reports about a fractured T-tube retained in bile ducts.[22,23]Our patient underwent sphincterotomy,stone extraction, T-tube removal and stenting.
Biliary stricture also is a severe complication of cholecystectomy. This complication occurred in 4 patients (7.5%) in our series. Kaffes et al[11]reported biliary stricture in only 4 patients (4%) in their series.The strictures in 3 of their patients were of mild severity and resolved with a short period of stenting, and one patient with a severe high-grade stricture had to be managed by endoscopic insertion of serial stents.Costamagna et al[24]successfully managed postoperative bile duct strictures with an increasing number of stents.The strictures in the present study resolved in response to a short period of stent placement.
In conclusion, stenting in outpatients and NBD in inpatients with simple leaks, sphincterotomy and stone extraction in patients with a leak with stone,sphincterotomy and stenting in patients with stricture with a leak and those with ligated bile duct should undergo surgery (Fig. 2). Patients with coagulopathy and stone/stricture should be managed with NBD for 1-3 weeks and sphincterotomy and stone extraction/stenting should be done later. Endoscopic management of bile leak is safe and effective; however, a prospective randomized trial is required.
Funding: None.
Ethical approval: Not needed.
Contributors: SV proposed the study, performed ERCP and wrote the fi rst draft. All authors contributed to the design and interpretation of the study and to further drafts. SV is the guarantor.Competing interest: No bene fi ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 No authors listed. A prospective analysis of 1518 laparoscopic cholecystectomies. The Southern Surgeons Club. N Engl J Med 1991;324:1073-1078.
2 Mehta SN, Pavone E, Barkun JS, Cortas GA, Barkun AN. A review of the management of post-cholecystectomy biliary leaks during the laparoscopic era. Am J Gastroenterol 1997;92:1262-1267.
3 Thuluvath PJ, Atassi T, Lee J. An endoscopic approach to biliary complications following orthotopic liver transplantation. Liver Int 2003;23:156-162.
4 Singh V, Narasimhan KL, Verma GR, Singh G. Endoscopic management of traumatic hepatobiliary injuries. J Gastroenterol Hepatol 2007;22:1205-1209.
5 Singh V, Reddy DC, Verma GR, Singh G. Endoscopic management of intrabiliary-ruptured hepatic hydatid cyst.Liver Int 2006;26:621-624.
6 Singh V, Bhalla A, Sharma N, Mahi SK, Lal A, Singh P.Pathophysiology of jaundice in amoebic liver abscess. Am J Trop Med Hyg 2008;78:556-559.
7 Foutch PG, Harlan JR, Hoefer M. Endoscopic therapy for patients with a post-operative biliary leak. Gastrointest Endosc 1993;39:416-421.
8 Bergman JJ, van den Brink GR, Rauws EA, de Wit L, Obertop H, Huibregtse K, et al. Treatment of bile duct lesions after laparoscopic cholecystectomy. Gut 1996;38:141-147.
9 Barkun AN, Rezieg M, Mehta SN, Pavone E, Landry S, Barkun JS, et al. Postcholecystectomy biliary leaks in the laparoscopic era: risk factors, presentation, and management. McGill Gallstone Treatment Group. Gastrointest Endosc 1997;45:277-282.
10 Bjorkman DJ, Carr-Locke DL, Lichtenstein DR, Ferrari AP,Slivka A, Van Dam J, et al. Postsurgical bile leaks: endoscopic obliteration of the transpapillary pressure gradient is enough.Am J Gastroenterol 1995;90:2128-2133.
11 Kaffes AJ, Hourigan L, De Luca N, Byth K, Williams SJ, Bourke MJ. Impact of endoscopic intervention in 100 patients with suspected postcholecystectomy bile leak. Gastrointest Endosc 2005;61:269-275.
12 Khan MH, Howard TJ, Fogel EL, Sherman S, McHenry L,Watkins JL, Canal DF, et al. Frequency of biliary complications after laparoscopic cholecystectomy detected by ERCP:experience at a large tertiary referral center. Gastrointest Endosc 2007;65:247-252.
13 Sandha GS, Bourke MJ, Haber GB, Kortan PP. Endoscopic therapy for bile leak based on a new classi fi cation: results in 207 patients. Gastrointest Endosc 2004;60:567-574.
14 Chow S, Bosco JJ, Heiss FW, Shea JA, Qaseem T, Howell D. Successful treatment of post-cholecystectomy bile leaks using nasobiliary tube drainage and sphincterotomy. Am J Gastroenterol 1997;92:1839-1843.
15 Agarwal N, Sharma BC, Garg S, Kumar R, Sarin SK.Endoscopic management of postoperative bile leaks.Hepatobiliary Pancreat Dis Int 2006;5:273-277.
16 Llach J, Bordas JM, Elizalde JI, Enrico C, Ginès A, Pellisé M, et al. Sphincterotomy in the treatment of biliary leakage.Hepatogastroenterology 2002;49:1496-1498.
17 Marks JM, Ponsky JL, Shillingstad RB, Singh J. Biliary stenting is more effective than sphincterotomy in the resolution of biliary leaks. Surg Endosc 1998;12:327-330.
18 Rerknimitr R, Sherman S, Fogel EL, Kalayci C, Lumeng L, Chalasani N, et al. Biliary tract complications after orthotopic liver transplantation with choledochocholedochos tomy anastomosis: endoscopic fi ndings and results of therapy.Gastrointest Endosc 2002;55:224-231.
19 Pfau PR, Kochman ML, Lewis JD, Long WB, Lucey MR,Olthoff K, et al. Endoscopic management of postoperative biliary complications in orthotopic liver transplantation.Gastrointest Endosc 2000;52:55-63.
20 Morelli J, Mulcahy HE, Willner IR, Baliga P, Chavin KD, Patel R,et al. Endoscopic treatment of post-liver transplantation biliary leaks with stent placement across the leak site. Gastrointest Endosc 2001;54:471-475.
21 Neidich R, Soper N, Edmundowicz S, Chokshi H, Aliperti G.Endoscopic management of bile duct leaks after attempted laparoscopic cholecystectomy. Surg Laparosc Endosc 1996;6:348-354.
22 Chaudhary A, Salunkhe S, Anand BS, Aranya RC. Postcholecystectomy syndrome due to a broken T-tube. Indian J Gastroenterol 1991;10:18-19.
23 Thors H, Gudjónsson H, Oddsson E, Cariglia N. Endoscopic retrieval of a biliary T-tube remnant. Gastrointest Endosc 1994;40:241-242.
24 Costamagna G, Pandol fi M, Mutignani M, Spada C, Perri V.Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents.Gastrointest Endosc 2001;54:162-168.
BACKGROUND: Biliary leak is an uncommon but signi fi cant complication following cholecystectomy. Endotherapy is an established method of treatment. However, the optimal intervention is not known.
METHOD: Eighty- fi ve patients with postcholecystectomy biliary leaks from July 2000 to March 2009 were retrospectively evaluated.
RESULTS: The study population was 20 males and 65 females with a mean age of 42.47 years. Patients presented with abdominal pain (46), jaundice (23), fever (23), abdominal distension (42), or bilious abdominal drain (67). Endoscopic retrograde cholangiopancreatography detected a leak at the cystic duct stump in 45 patients, stricture with middle common bile duct leak in 4, leak from the right hepatic duct in 3, and a ligated common bile duct in 32. Twelve also had bile duct stones. One had a broken T-tube with stones.Endotherapy was possible in 53 patients. Three patients with stones, one with a broken T-tube with stones, and 4 with stricture of the common bile duct with a leak were managed with sphincterotomy and stenting. Eight patients with a cystic duct stump leak with stones were managed with sphincterotomy and stone extraction. Three outpatients and 12 inpatients with a cystic duct stump leak were managed with sphincterotomy and stent and sphincterotomy and nasobiliary drain, respectively. Five patients with a cystic duct stump leak were managed with stenting. Sixteen with coagulopathy were managed with only nasobiliary drain(9) or stent (7). Leak closure was achieved in 100% patients.Four developed mild pancreatitis which improved with conservative treatment.
CONCLUSIONS: Endoscopic intervention is a safe and effective method of treatment of postcholecystectomy biliary leaks. However, management should be individualized based on factors such as outpatients or inpatients, presence of stone,stricture, ligature, or coagulopathy.
Author Af fi liations: Departments of Hepatology (Singh V) and Surgery(Singh G, Verma GR and Gupta R), Postgraduate Institute of Medical Education and Research, Chandigarh, India
Virendra Singh, MD, DM, Department of Hepatology, Postgraduate Institute of Medical Education and Research,Chandigarh 160 012, India (Fax: 91-172-2744401; Email: virendrasingh100@hotmail.com)
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
March 18, 2010
Accepted after revision June 29, 2010
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Pancreatic duct stones in patients with chronic pancreatitis: surgical outcomes
- Methylprednisolone inhibits activated CD4+ T cell survival promoted by toll-like receptor ligands
- Magnetic resonance imaging-guided percutaneous cryoablation of hepatocellular carcinoma in special regions
- Radiofrequency ablation, heat shock protein 70 and potential anti-tumor immunity in hepatic and pancreatic cancers: a minireview
- Endoscopic retrograde cholangiopancreatography outcome from a single referral center in Iran
- Application of a medical image processing system in liver transplantation
