Pancreatic duct stones in patients with chronic pancreatitis: surgical outcomes
2010-12-14BoNanLiuTaiPingZhangYuPeiZhaoQuanLiaoMengHuaDaiandHanXiangZhan
Bo-Nan Liu, Tai-Ping Zhang, Yu-Pei Zhao, Quan Liao, Meng-Hua Dai and Han-Xiang Zhan
Beijing, China
Pancreatic duct stones in patients with chronic pancreatitis: surgical outcomes
Bo-Nan Liu, Tai-Ping Zhang, Yu-Pei Zhao, Quan Liao, Meng-Hua Dai and Han-Xiang Zhan
Beijing, China
(Hepatobiliary Pancreat Dis Int 2010; 9: 423-427)
pancreatic duct stone;chronic pancreatitis;surgical management;modi fi ed Puestow procedure
Introduction
Pancreatic duct stone (PDS) is a common complication during the natural course of chronic pancreatitis(CP) and contributes to the pathogenesis and complications of CP. A survey showed that the prevalence of PDS in patients with CP is 8.5% (171/2008)in China.[1]Abdominal pain, one of the principal symptoms of CP, is believed to be caused by obstruction of the pancreatic duct with increasing intraductal pressure and parenchymal ischemia either by stones or stricture.[2]The standard intervention for CP with obstructing duct stones is stone retrieval and duct drainage by endoscopic, extracorporeal shockwave lithotripsy or surgery, depending upon the size and location of stone(s).[3-5]A recent randomized trial revealed a better 2-year outcome after surgery compared with endoscopic treatment to drain the obstructive pancreatic duct in patients with CP.[6]For patients with failed nonsurgical treatments, surgery is the only option to relieve symptoms. In this study we investigated the outcomes of surgical procedures to treat PDS in patients with CP.
Methods
Between January 2004 and September 2009 years, 35 patients were diagnosed with CP associated with PDS,and underwent surgery at our hospital. Patients with PDS treated by conservative therapy and those with any pancreatic neoplasm were excluded. All patients met the diagnostic criteria of CP issued by the Pancreas Study Group, the Chinese Society of Gastroenterology.[7]PDS was preoperatively diagnosed by imaging and con fi rmed operatively.
Reviewed data included demographics, symptoms and signs, results of blood tests, image fi ndings,surgical approaches, pathological results, and shortterm postoperative complications. The patients were followed by telephone interview and mail, and the data collected included patients' pain level and post-discharge medical events including PDS recurrence,pancreatic carcinogenesis, acute pancreatitis, steatorrhea and, if relevant, onset of diabetes mellitus. All patient comments were con fi rmed by clinical presentation,imaging studies, and laboratory tests.
If the stones found during surgery were removed and no sign of stone was found in the fi rst postoperative imaging examination, complete stone clearance was de fi ned; otherwise incomplete stone clearance was considered. The statistical signi fi cance of postoperative pain relief between complete and incomplete stone clearance was assessed by Fisher's exact test. A P value less than 0.05 was considered statistically signi fi cant.
ResultsClinical characteristics
The demographic data showed that there were more men than women, and nearly half of them were drank or smoked (Table 1). The most signi fi cant symptom was abdominal pain, followed by diabetes mellitus, steatorrhea,and jaundice. Two patients without abdominal pain presented with hyperglycemia and dyspepsia, for whichtenderness in the upper abdomen was the most common sign. Twenty-four patients had a history of acute pancreatitis, 11 had a prior gall stone, whereas none of the patients had a family history of CP.
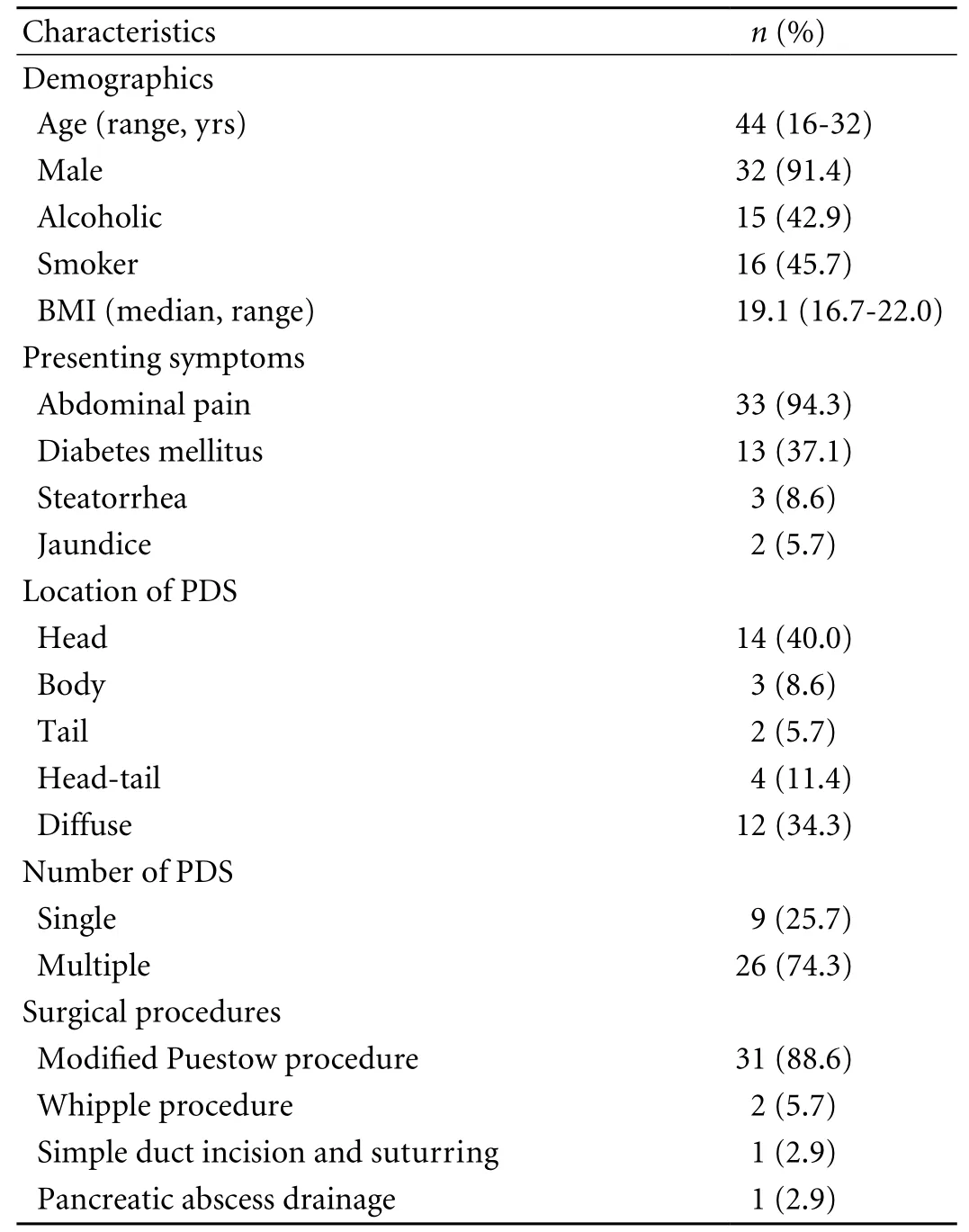
Table 1. Patient characteristics
Preoperative diagnosis
The diagnosis of PDS associated with CP was made by evaluating preoperative images including transabdominal ultrasonography (TAUS), computed tomography (CT),endoscopic retrograde cholangiopancreatography (ERCP),or magnetic resonance cholangiopancreatography (MRCP).Similar to other reports,[8,9]30 (85.7%) of the 35 patients in our study were con fi rmed with a diagnosis of PDS associated with CP either by TAUS, CT, or both.
Characteristics of pancreatic stones
PDSs were present throughout the pancreas. 40.0%were totally con fi ned at the head of the pancreas, and 45.7% were at but not limited to pancreatic head in head-tail or diffuse pattern (Table 1). The stones were round in shape and usually appeared lemon-yellow in color (Fig.).
Surgical considerations
All patients underwent surgery (Table 1). In 3 patients ERCP was done but failed to extract PDS before surgery, and in 2 patients a pancreatic stent was placed.A modi fi ed Puestow procedure was performed to form an arti fi cial passage connecting the pancreas to the jejunum. Pancreaticojejunostomy was performed by a Roux-en-Y loop procdure posterior to the transverse colon. Before incising the main pancreatic duct,the surgeon felt for calculi and a dilated duct, and recon fi rmed the dilated pancreatic duct using a syringe.A full-length incision was then made to complete the side-to-side pancreaticojejunostomy. Two patients could not be excluded from the involvement of pancreatic head neoplasm and underwent a Whipple procedure. One of them underwent simple stone extraction via a simple duct incision and suturing and the other underwent an external drainage of pancreatic abscess. Dilation of the main pancreatic duct was seen in 33 patients at surgery (mean duct diameter 9.3 mm). A pancreatic stent was placed in 5 patients during surgery, and in one patient the stent was positioned out of the abdominal cavity through the small intestine. The overall operative time ranged from 3 to 14 hours (mean 4.6 hours); the operative time for the modi fi ed Puestow procedure ranged from 3 to 6 hours (mean 4.3 hours).

Fig. Multiple PDSs obtained from a 23-year-old male patient.
The rate of incomplete stone clearance after the modi fi ed Puestow procedure (31 patients) was 37.5%(3/8) in patients with a single stone and 56.5% (13/23)in patients with multiple stones. The three single stones that were incompletely extracted during surgery were all con fi ned in the pancreatic head. The multiple stones of incomplete extraction in 13 patients were mostly associated with the pancreatic head, whereas some were also in the pancreatic tail (3 patients) or in the whole pancreas (7). In the remaining 4 patients, incomplete stone clearance occurred in one patient with multiple stones who received external drainage for a pancreatic abscess because the stone was inaccessible.
The mean postoperative hospital stay for all 35 patients was 14.3 days (8-83 days), and 12.3 days for those surgically treated by the modi fi ed Puestow procedure. Somatostatin was administered to suppress pancreatic juice secretion in 30 of the 35 patients.There were no postoperative deaths, and the overall postoperative morbidity rate was 5.7% (2/35). Of the two patients with complications, one had a pancreatic fi stula and the other, who had undergone Whipple procedure, had abdominal bleeding 36 hours after surgery and abdominal infection on postoperative day 12. The 31 patients who had received the modi fi ed Puestow procedure showed no postoperative pancreatic fi stula, bleeding, acute pancreatitis, or hyperglycemia.
Long-term follow-up
Twenty-eight of the 35 patients were followed up for 4-67 months (median 37 months); among them 27 underwent the modi fi ed Puestow procedure
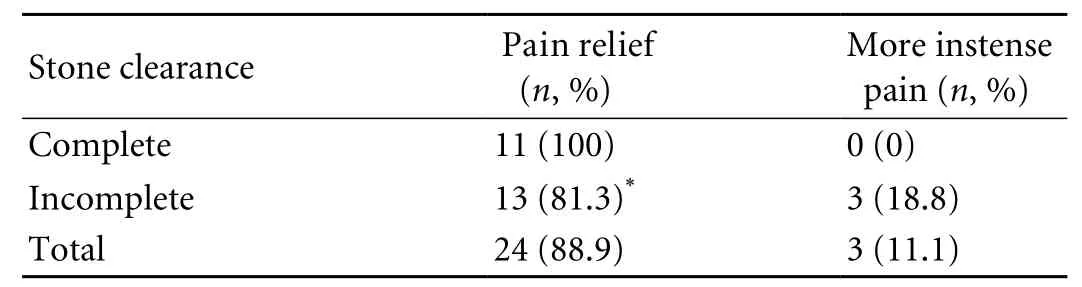
Table 2. Pain after modi fi ed Puestow procedure (n=27)
Discussion
PDS, fi rst reported in 1667,[10]is a common pathologic event in cases of CP. In western countries, the incidence of PDS associated with CP may be as high as 50%-90%,[11]whereas in China, it is 8.5%.[1]
Passing a pancreatic stone spontaneously is rare.[12]ERCP and extracorporeal shockwave lithotripsy are effective and safe in clearing stones from the pancreatic duct and in relieving pain, with an overall complication rate of 0-43%.[4,13,14]The outcomes of endoscopic treatment were reported to be equivalent to those of surgery; in the present study the indications for endoscopic treatment were ≤3 stones, stones con fi ned in the head and body of the pancreas, absence of restricted pancreatic duct, PDS diameter ≤10 mm, and noncompacted stone(s).[15]Additional and larger stones were retrieved successfully using a modi fi ed metallic stent.[16]For patients who need treatment but do not meet the aforementioned indications, or for whom conservative therapy fails, surgery is extremely necessary.
In 1883 the fi rst case of surgical removal of PDS was reported.[10]A randomized controlled trial indicated that during a 2-year follow-up, surgery is superior to endotherapy for pain relief (75% vs. 32%) in patients with painful obstructive CP,[6]a fi nding similar to the result of another trial.[17]Fang et al[8]reported a symptom remission rate of 65%-94%, a mortality of 0-5%, and a morbidity of 20%-40%, based on their studies. In our study, 88.9% patients reported pain relief after the modi fi ed Puestow procedure with complete or incomplete stone clearance (Table 2).
Selection of surgical approach should be guided by the size, number, and type of PDS. Depending on the location of stones, four types of PDS have been established: type Ⅰ in the head of the pancreas, typeⅡ in the body, type Ⅲ in the tail, and type Ⅳ in the whole pancreas.[18]Drainage by pancreatic ductotomy is generally applicable for patients with a dilated pancreatic duct (≥6 mm); the drainage includes the Puestow,modi fi ed Puestow, and Frey procedures.[19]The Berger procedure, in which the pancreatic head is removed but the duodenum is preserved, and the Whipple procedure are suitable for type Ⅰ stones, however distal pancreatectomy is suitable for type Ⅲ stones. For patients with type Ⅱ stones, the modi fi ed Puestow procedure or segmental resection of the pancreas is suitable. For patients with type Ⅳ stones, an alternative to drainage is a subtotal pancreatectomy, which allows 95% removal of the pancreas, preserving only a thin layer of pancreatic tissue attached to the duodenum.
Side-to-side pancreaticojejunostomy is effective for most PDSs. At our institution, 88.6% of the 35 patients underwent the modi fi ed Puestow procedure, greater than the percentage of other case series because in all 31 patients the main pancreatic duct diameter was ≥6 mm, indicating a drainage procedure rather than resection. The modi fi ed Puestow procedure was found to be safe and suitable for unobstructed pancreatic juice drainage.[20]In the 14 patients with stones only in the head of the pancreas, 12 underwent pancreatic ductotomy for stone removal and decompression. In these patients, a full-length and wide incision throughout the dilated duct was necessary and,if necessary, the anterior wall of the pancreatic head was partially resected to expose enough area for adequate drainage. Although the mortality due to the Whipple procedure is below 5% in large pancreatic centers,[21]the procedure is complex and time-consuming, and carries the risk of additional postoperative complications,thus limiting its wide application. In our study, one patient experienced abdominal bleeding and infection after the Whipple operation, necessitating an 83-day postoperative hospital stay. The Whipple procedure is not always necessary for pancreatic head stones if they can be removed and the interductal pressure decreases after pancreaticojejunostomy, but the procedure is required when a pancreatic head tumor is suspected.
The incompletely removed stones were either within or partly within the pancreatic head, and they showed dot-like calci fi cation or were compacted into the pancreatic parenchyma. Sometimes it is dif fi cult to widely unroof the pancreatic duct within the pancreatic head and uncinate to clear dot-like calculi due to the vessel complexes. In addition, forced removal of the compacted stones may lead to massive postoperative bleeding and pancreatic leakage. Furthermore, the size of the pancreatic tail usually decreases in cases of CP,and the duct within the tail is sometimes not dilated for pancreaticojejunostomy, especially when it is adjacent to the spleen. Therefore, stones or fragments are deliberately left at the site where removal is dif fi cult. In our patients, although some stones were not completely removed, we adequately decompressed the pancreatic duct by opening the dilated duct as much as possible.
Studies on obstructive CP showed that after ERCP and extracorporeal shockwave lithotripsy, pain recurs more frequently in patients with incomplete stone removal than in those with complete removal.[22]Additional stenting for the main pacreatic duct after extracting pancreatic stones may reduce the risk of recurrence of pancreatic symptoms.[23]In our study, there was no difference in pain relief between the patients with complete and incomplete stone removal after the modi fi ed Puestow procedure. This demonstrates that good decompression rather than complete clearance of all stones is the decisive factor for postoperative outcome.Decompression promotes longitudinal anastomosis that ensures drainage over the full length of the pancreas and also opens the pancreatic capsule to alleviate interstitial pressure.[6]In our study, 2 of 3 patients who experienced more intense pain after the modi fi ed Puestow procedure were treated with plastic stents before surgery, but the stents were removed during surgery. It is uncertain that there is any correlation between preoperative stenting and postoperative pain relief, however, Sasahira et al[23]suggested that endoscopic stenting may worsen pancreatic duct morphologic abnormalities and lead to the risk of less pain relief.
Steatorrhea and diabetes mellitus are indications for pancreatic exocrine and endocrine dysfunction.Postoperative dysfunction in exocrine and endocrine glands was seen in 21.4% and 7.1% of the 28 patients we followed up respectively, indicating that surgical drainage could not have prevented pancreatic damage over the long-term follow-up. In this study, no pancreatic carcinogenesis was observed after surgery, but longer follow-up was necessary.
In conclusion, the modi fi ed Puestow procedure has fewer complications than other procedures and is the most widely used procedure for PDS in patients with CP at our institution. Good decompression rather than complete clearance of all stones is the most important factor for postoperative outcome, after which abdominal pain is reduced in most of patients during a long-term follow-up.
Funding: None.
Ethical approval: Not needed.
Contributors: LBN and ZTP made equal contributions to the study. ZTP and ZYP proposed the study. LBN wrote the fi rst draft.LBN and ZTP analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. ZYP is the guarantor.
Competing interest: No bene fi ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Wang LW, Li ZS, Li SD, Jin ZD, Zou DW, Chen F. Prevalence and clinical features of chronic pancreatitis in China: a retrospective multicenter analysis over 10 years. Pancreas 2009;38:248-254.
2 Di Sebastiano P, di Mola FF, Buchler MW, Friess H.Pathogenesis of pain in chronic pancreatitis. Dig Dis 2004;22:267-272.
3 Li L, Zhang SN. Management of pancreatic duct stone.Hepatobiliary Pancreat Dis Int 2008;7:9-10.
4 Howell DA. Pancreatic stones: treat or ignore? Can J Gastroenterol 1999;13:461-465.
5 Devière J, Delhaye M, Cremer M. Pancreatic duct stones management. Gastrointest Endosc Clin N Am 1998;8:163-179.
6 Cahen DL, Gouma DJ, Nio Y, Rauws EA, Boermeester MA,Busch OR, et al. Endoscopic versus surgical drainage of the pancreatic duct in chronic pancreatitis. N Engl J Med 2007;356:676-684.
7 Pancreas Study Group, Chinese Society of Gastroenterology.Guidelines for the diagnosis and treatment of chronic pancreatitis (Nanjing, 2005). Chin J Dig Dis 2005;6:198-201.
8 Fang WL, Shyr YM, Su CH, Chen TH, Wu CW, Lui WY. Longterm follow-up study of surgical treatment for pancreatic stones. Hepatogastroenterology 2007;54:246-249.
9 Li JS, Zhang ZD, Tang Y, Jiang R. Retrospective analysis of 88 patients with pancreatic duct stone. Hepatobiliary Pancreat Dis Int 2007;6:208-212.
10 Haggard WD, Kirtley JA. Pancreatic calculi: A review of sixtyfi ve operative and one hundred thirty-nine non-operative cases.Ann Surg 1939;109:809-826.
11 Ammann RW, Muench R, Otto R, Buehler H, Freiburghaus AU, Siegenthaler W. Evolution and regression of pancreatic calci fi cation in chronic pancreatitis. A prospective long-term study of 107 patients. Gastroenterology 1988;95:1018-1028.
12 Rhee J, Scheiman J, Inadomi J. "Spontaneous" passage of a pancreatic duct stone. Gastrointest Endosc 2003;57:278-280.
13 Farnbacher MJ, Schoen C, Rabenstein T, Benninger J,Hahn EG, Schneider HT. Pancreatic duct stones in chronic pancreatitis: criteria for treatment intensity and success.Gastrointest Endosc 2002;56:501-506.
14 Guda NM, Partington S, Freeman ML. Extracorporeal shock wave lithotripsy in the management of chronic calci fi c pancreatitis: a meta-analysis. JOP 2005;6:6-12.
15 Sherman S, Lehman GA, Hawes RH, Ponich T, Miller LS,Cohen LB, et al. Pancreatic ductal stones: frequency of successful endoscopic removal and improvement in symptoms.Gastrointest Endosc 1991;37:511-517.
16 Yang XJ, Lin Y, Zeng X, Shi J, Chen YX, Shen JW, et al. A minimally invasive alternative for managing large pancreatic duct stones using a modi fi ed expandable metal mesh stent.Pancreatology 2009;9:111-115.
17 Díte P, Ruzicka M, Zboril V, Novotny I. A prospective,randomized trial comparing endoscopic and surgical therapy for chronic pancreatitis. Endoscopy 2003;35:553-558.
18 Chen Y, He Y, Zhao J, Liu Y, Liu YF, Cao HL, et al. The classi fi cation and management of pancreatic duct stone.Zhonghua Wai Ke Za Zhi 2004;42:417-420.
19 Mihaljevic AL, Kleeff J, Friess H, Büchler MW, Beger HG.Surgical approaches to chronic pancreatitis. Best Pract Res Clin Gastroenterol 2008;22:167-181.
20 Ceppa EP, Pappas TN. Modi fi ed puestow lateral pancreaticojejunostomy. J Gastrointest Surg 2009;13:1004-1008.
21 Ho V, Heslin MJ. Effect of hospital volume and experience on in-hospital mortality for pancreaticoduodenectomy. Ann Surg 2003;237:509-514.
22 Tadenuma H, Ishihara T, Yamaguchi T, Tsuchiya S, Kobayashi A, Nakamura K, et al. Long-term results of extracorporeal shockwave lithotripsy and endoscopic therapy for pancreatic stones. Clin Gastroenterol Hepatol 2005;3:1128-1135.
23 Sasahira N, Tada M, Isayama H, Hirano K, Nakai Y, Yamamoto N, et al. Outcomes after clearance of pancreatic stones with or without pancreatic stenting. J Gastroenterol 2007;42:63-69.
BACKGROUND: Pancreatic duct stone (PDS) is a common complication of chronic pancreatitis. Surgery is a common therapeutic option for PDS. In this study we assessed the surgical procedures for PDS in patients with chronic pancreatitis at our hospital.
METHOD: Between January 2004 and September 2009, medical records from 35 patients diagnosed with PDS associated with chronic pancreatitis were retrospectively reviewed and the patients were followed up for up to 67 months.
RESULTS: The 35 patients underwent ultrasonography,computed tomography, or both, with an overall accuracy rate of 85.7%. Of these patients, 31 underwent the modi fi ed Puestow procedure, 2 underwent the Whipple procedure, 1 underwent simple stone removal by duct incision, and 1 underwent pancreatic abscess drainage. Of the 35 patients, 28 were followed up for 4-67 months. There was no postoperative death before discharge or during follow-up. After the modi fi ed Puestow procedure, abdominal pain was reduced in patients with complete or incomplete stone clearance (P>0.05).Steatorrhea and diabetes mellitus developed in several patients during a long-term follow-up.
CONCLUSIONS: Surgery, especially the modi fi ed Puestow procedure, is effective and safe for patients with PDS associated with chronic pancreatitis. Decompression of intraductal pressure rather than complete clearance of all stones predicts postoperative outcome.
Author Af fi liations: Department of General Surgery, Peking Union Medical College Hospital, Peking Union Medical College & Chinese Academy of Medical Sciences, Beijing 100730, China (Liu BN, Zhang TP, Zhao YP, Liao Q, Dai MH and Zhan HX)
Yu-Pei Zhao, MD, Department of General Surgery,Peking Union Medical College Hospital, Peking Union Medical College& Chinese Academy of Medical Sciences, Beijing 100730, China (Tel:86-10-65296014; Email: zhao8028@263.net)
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
March 18, 2010
Accepted after revision May 21, 2010
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Methylprednisolone inhibits activated CD4+ T cell survival promoted by toll-like receptor ligands
- Endoscopic management of postcholecystectomy biliary leakage
- Magnetic resonance imaging-guided percutaneous cryoablation of hepatocellular carcinoma in special regions
- Radiofrequency ablation, heat shock protein 70 and potential anti-tumor immunity in hepatic and pancreatic cancers: a minireview
- Endoscopic retrograde cholangiopancreatography outcome from a single referral center in Iran
- Application of a medical image processing system in liver transplantation
