Total laparoscopic hysterectomy after liver transplantation
2010-12-14HaiBingZhuYueJinShaoTingXuYaXianXiaandLiPingXie
Hai-Bing Zhu, Yue Jin, Shao-Ting Xu, Ya-Xian Xia and Li-Ping Xie
Hangzhou, China
Total laparoscopic hysterectomy after liver transplantation
Hai-Bing Zhu, Yue Jin, Shao-Ting Xu, Ya-Xian Xia and Li-Ping Xie
Hangzhou, China
(Hepatobiliary Pancreat Dis Int 2010; 9: 438-440)
total laparoscopic hysterectomy;liver transplantation;immunosuppression
Introduction
With improvements in surgical techniques and immunosuppression, a growing number of female patients have undergone liver transplantation (LT) for end-stage hepatic disease.Hermann et al[1]reviewed the gender-speci fi c differences associated with living donor LT and found that 41% of the organs were distributed to female recipients. These patients may also suffer from gynecologic diseases for which a hysterectomy may be performed.[2]
Laparoscopic surgery has been widely used for its advantages such as postoperative pain relief and rapid recovery, which promote its application in treating diseases following organ transplantation.[3]Laparoscopic hysterectomy in patients after kidney transplantation has been reported,[4]but laparoscopic hysterectomy after LT has not been reported. We treated two cases of laparoscopic hysterectomy after LT and found that they were bene fi ted from this intervention.
Case reportsCase 1
A 48-year-old woman (gravida 4, para 2) having prior LT and Cesarean was admitted to the hospital because of dysmenorrhea for fi ve years. The patient underwent LT using the piggyback technique due to HCV-related cirrhosis 14 months ago. An episode of cholangitis treated with antibiotics occurred during the postoperative period. Peroral tacrolimus,mycophenolate mofetil, and prednisone were used as immunosuppressants. Upon admission, ultrasonography showed that the posterior uterine wall was enlarged to 6 cm in diameter. After adenomyosis was diagnosed,total laparoscopic hysterectomy (TLH) was performed on May 29, 2006. The patient was positioned for laparoscopy in the dorsal lithotomy position while prophylactic antibiotic injection was given. A 1-cm trocar was inserted through the umbilicus to hold the optic camera. Two 0.5-cm trocars were separatelyinserted into the lower abdomen. The whole uterus resembled that of 3-month gestation, and mild pelvic adhesion was found between the uterus and bilateral ovaries. The ligaments around the uterus were transected with endoscopic scissors after electrocoagulation using bipolar electrocautery. The bilateral uterine arteries were ligated by suture and intracorporeal ties. The uterus was removed through the vagina before suturing of the vaginal cuff. The extirpated uterine weight was 520 g.The operation time was 95 minutes and the blood loss was 100 ml. The patient was conscious 1 hour later and took immunosuppressants 6 hours after the operation.On postoperative day 3, she suffered from diarrhea due to Candida albicans in the injection. Antifungal therapy based on fl uconazole injection (200 mg/day for 2 days)was added and she recovered soon. She was discharged on the 6th day postoperatively.
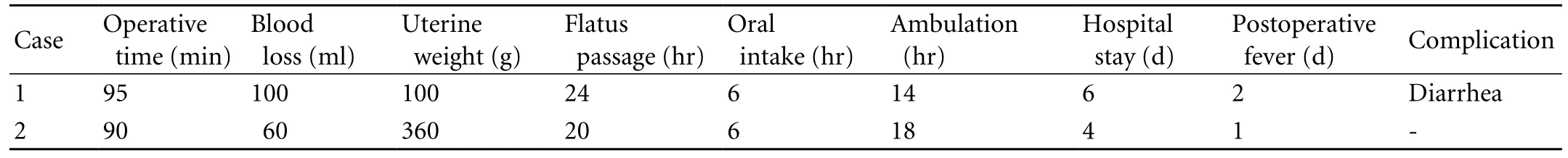
Table. Clinical outcomes and complications in patients receiving TLH after liver transplantation
Case 2
A 48-year-old woman (gravida 4, para 1) was admitted to the hospital due to menorrhagia for two years. Nineteen months ago she underwent LT using the piggyback technique because of alcoholic cirrhosis. Posttransplantation immunosuppression was prescribed with a combination of tacrolimus, mycophenolate mofetil, and prednisone. One year previously, a transcervical resection of the endometrium was made and an endometrial polyp was diagnosed. This operation failed to reduce the volume of menstrual blood. Ultrasonography revealed that several masses oppressed the line of the endometrium with the largest mass being 2.8 cm in diameter. A diagnosis of hysteromyoma and subsequent severe anemia was established. After transfusion of a pack of leukocyte-depleted blood cells, TLH was performed on June 21, 2006. No adhesion was found, and the surgical approach was similar to that used for case 1. The operative time was 90 minutes and the blood loss was 60 ml. She recovered well after the operation and was discharged on the 4th postoperative day.
The clinical outcomes and complications of the two patients are listed in the Table. The changes of plasma concentration of tacrolimus are listed in Fig. The preoperative and postoperative liver function indices including alanine aminotransferase and aspartate aminotransferase were within the normal limits in both cases. Both patients were followed up to the present and routine gynecologic examinations were performed twice a year with negative disclosure.
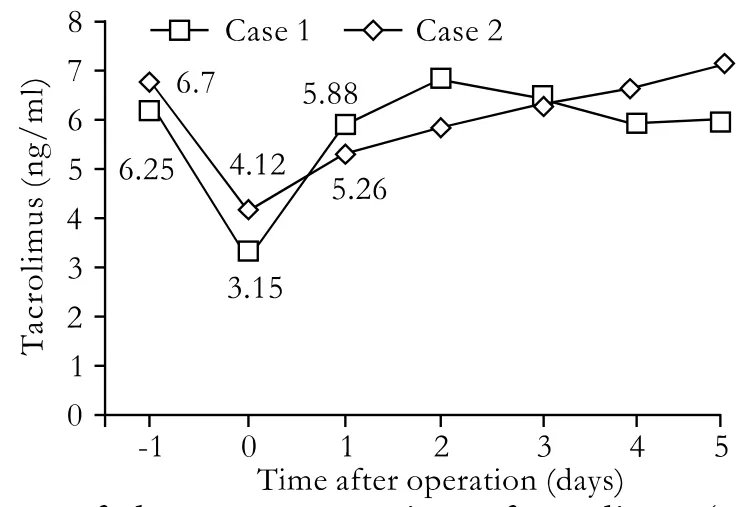
Fig. Changes of plasma concentrations of tacrolimus (ng/ml) in 2 patients.
Discussion
The number of women who undergo LT is growing every year. In the United States, there are more than 3000 LT recipients of childbearing age.[5]Females in this category may encounter complications or other diseases originating from the reproductive organs. The reported cases include lymphoproliferative disorder of the cervix,[6]endometrial adenocarcinoma[2]and acute vaginal bleeding.[7]Laparohysterectomy is usually selected when surgical therapy is unavoidable.However, hysterectomy can also be accomplished by laparoscopy with prominent bene fi ts of better cosmesis,decreased length of hospitalization, and quicker recovery compared with laparohysterectomy.[8]As far as we know, the present report is the fi rst one on laparoscopic hysterectomy in patients who have received LT.
Laparoscopic technology has been widely used in these patients. The operation includes ventral hernia repair, splenectomy, and right adrenalectomy.[9-11]Laparoscopic operation in the lower abdomen also includes appendectomy[12]and total proctocolectomy[13]after LT. These operations, especially those in the pelvic cavity, indicate that laparoscopic technology is feasible in cases of hysterectomy after LT.
Before TLH, three issues must be considered. First,whether there is adhesion between the viscera and abdominal wall because previous abdominal surgery or peritonitis. This adhesion may affect puncturing by the Veress needle and thus add dif fi culty to the operation.Second, whether pneumoperitoneum will harm the transplanted liver. And third, whether this operative method is superior to laparotomy. In our practice, the site for puncturing of the Veress needle was the umbilical skinfold. Laparoscopy con fi rmed there was no adhesion of the viscera to the undersurface of the umbilicus. Only mild adhesion was found between the uterus and the bilateral ovaries in case 1, which may be the result of the prior Cesarean. Preoperative and postoperative liver function was within normal limits, suggesting that pneumoperitoneum has no adverse effect on the transplanted liver.
The operative times in both cases were less than 95 minutes, with blood loss less than 100 ml. The recovery of oral intake, fl atus passage, and ambulation was well within 1 day after the operation. These data are similar to those on laparoscopic hysterectomy for benign pathology.[14]No intramuscular meperidine was required and the hospital stay ranged from 4 to 6 days. In addition,the patients bene fi ted from small wounds. Since oral immunosuppressant drugs may increase wound complications.[15]The blood concentration of tacrolimus decreased immediately after the operation, but increased to the preoperative range quickly the next day due to its intake 6 hours after operation (Fig.). TLH may reduce the time of recovery of normal gastrointestinal function in comparison with conventional abdominal hysterectomy.[16]There were no major complications except mild postoperative fever accompanied by diarrhea in case 1 for two days. Tanaka et al[2]reported the same situation and considered the fever after the operation to be secondary to the immunosuppressive therapy. They reduced the volume of tacrolimus until it was completely stopped. But in case 1, we added fl uconazole injection and the outcome was satisfactory. Thus attention should be paid to the possibility of fungal infection in patients during hospitalization after LT.
In conclusion, the two cases indicate that TLH is a safe and effective treatment for adenomyosis and hysteromyoma after LT. However, the fi ndings are preliminary because of the small number of patients.
Funding: None.
Ethical approval: Not needed.
Contributors: ZHB wrote the fi rst draft of this report. All authors contributed to the intellectual context and approved the fi nal version. ZHB is the guarantor.
Competing interest: No bene fi ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Hermann HC, Klapp BF, Danzer G, Papachristou C. Genderspeci fi c differences associated with living donor liver transplantation: a review study. Liver Transpl 2010;16:375-386.
2 Tanaka H, Sato H, Konishi Y, Fujimoto T, Takahashi O, Tanaka T. Endometrial adenocarcinoma after liver transplantation. J Obstet Gynaecol Res 2005;31:224-226.
3 Krajewski E, Soriano IS, Ortiz J. Laparoscopy in transplantation JSLS 2006;10:426-431.
4 Chen SY, Huang SC, Sheu BC, Chang DY, Chou LY, Hsu WC,et al. Laparoscopically assisted vaginal hysterectomy following previous kidney transplantation. Taiwan J Obstet Gynecol 2009;48:249-253.
5 Health Resources and Services Administration 2006.2006 annual report of the U.S. Organ Procurement and Transplantation Network and the Scienti fi c Registry of Transplant Recipients: transplant data 1996-2005. Available at: http://optn.transplant.hrsa.gov/data/annualReport.asp.Accessed July 8, 2010.
6 Nagarsheth NP, Kalir T, Rahaman J. Post-transplant lymphoproliferative disorder of the cervix. Gynecol Oncol 2005;97:271-275.
7 Nicholas SL, Rulin MC. Acute vaginal bleeding in women undergoing liver transplantation. Am J Obstet Gynecol 1994;170:733-736.
8 Sokol AI, Green IC. Laparoscopic hysterectomy. Clin Obstet Gynecol 2009;52:304-312.
9 Harold K, Mekeel K, Spitler J, Frisella M, Merritt M, Tessier D,et al. Outcomes analysis of laparoscopic ventral hernia repair in transplant patients. Surg Endosc 2009;23:1835-1838.
10 Kato H, Usui M, Azumi Y, Ohsawa I, Kishiwada M, Sakurai H,et al. Successful laparoscopic splenectomy after living-donor liver transplantation for thrombocytopenia caused by antiviral therapy. World J Gastroenterol 2008;14:4245-4248.
11 Gill IS, Meraney AM, Mayes JT, Bravo EL. Laparoscopic right adrenalectomy after liver transplantation. Transplantation 2001;71:1350-1351.
12 Savar A, Hiatt JR, Busuttil RW. Acute appendicitis after solid organ transplantation. Clin Transplant 2006;20:78-80.
13 Hochman DJ, Pemberton JH. Hand-assisted laparoscopic total proctocolectomy and ileal pouch-anal anastomosis after liver transplant for primary sclerosing cholangitis. Surg Laparosc Endosc Percutan Tech 2007;17:56-57.
14 Candiani M, Izzo S, Bulfoni A, Riparini J, Ronzoni S, Marconi A. Laparoscopic vs vaginal hysterectomy for benign pathology.Am J Obstet Gynecol 2009;200:368.e1-7.
15 Humar A, Ramcharan T, Denny R, Gillingham KJ, Payne WD, Matas AJ. Are wound complications after a kidney transplant more common with modern immunosuppression?Transplantation 2001;72:1920-1923.
16 Gyr T, Ghezzi F, Arslanagic S, Leidi L, Pastorelli G, Franchi M.Minimal invasive laparoscopic hysterectomy with ultrasonic scalpel. Am J Surg 2001;181:516-519.
BACKGROUND: The number of females who undergo liver transplantation is growing and sometimes gynecologic operations are needed to control gynecologic diseases after liver transplantation.
METHOD: Total laparoscopic hysterectomy was performed in 2 patients who had undergone liver transplantation, one for adenomyosis and the other for hysteromyoma.
RESULTS: It was safe to create a pneumoperitoneum through the umbilical skinfold even though mild adhesion in the pelvic cavity occurred in one patient. The operative times were 95 and 90 minutes, with blood loss of about 100 and 60 ml, respectively. Oral intake, fl atus passage, and ambulation recovered within a day, after the operation. No signi fi cant changes in liver function were observed except complication of diarrhea caused by Candida albicans in one patient.
CONCLUSIONS: The result of the two patients suggest that total laparoscopic hysterectomy is a safe and effective surgical approach for patients who have undergone liver transplantation.
Author Af fi liations: Department of Obstetrics and Gynecology (Zhu HB, Jin Y, Xu ST and Xia YX), and Department of Urology (Xie LP), First Af fi liated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, China Corresponding Author: Li-Ping Xie, PhD, Department of Urology, First Af fi liated Hospital, Zhejiang University School of Medicine, Hangzhou 310003, China (Tel: 86-571-86517305; Fax: 86-571-87072577; Email: lpxie88@yahoo.cn)
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
January 13, 2010
Accepted after revision April 26, 2010
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Giant cell tumor of the pancreas: a pathological diagnosis with poor prognosis
- Pancreatic duct stones in patients with chronic pancreatitis: surgical outcomes
- Letters to the Editor
- Outcomes and mechanisms of ischemic preconditioning in liver transplantation
- Percutaneous injection of hemostatic agents for active liver hemorrhage
- Application of a medical image processing system in liver transplantation
