Letters to the Editor
2010-12-14
Letters to the Editor
The Editor welcomes submissions for possible publication in the Letters to the Editor section.
Letters commenting on an article published in the Journal or other interesting pieces will be considered if they are received within 6 weeks of the time the article was published. Authors of the article being commented on will be given an opportunity to offer a timely response to the letter. Authors of letters will be notified that the letter has been received. Unpublished letters cannot be returned.
Primary pancreatic hydatid disease associated with acute pancreatitis
To the Editor:
Hydatid disease is still endemic in the Middle East as well as in Turkey. Although the liver and lungs are the most frequently involved, other organs may also be affected.[1-3]Isolated involvement of the pancreas is unusual, and acute pancreatitis secondary to hydatid cyst has rarely been reported. To our knowledge, 4 cases have been reported in the literature.[4]Here we report a new case of acute pancreatitis due to primary pancreatic hydatid disease.
An 18-year-old man was admitted to our clinic with complaints of abdominal and back pain, nausea, vomiting, and fever for 15 days. His past medical history was unremarkable. On physical examination, vital signs were normal other than a temperature of 38.5 ℃. He had tenderness in the right abdominal quadrant while examination of other systems was normal. Laboratory analyses were as follows: white blood count 24 500/mm3; hemoglobin 13.8 g/dl; platelets 159 000/mm3; amylase 1540 U/L (17-115); alanine aminotransferase (ALT) 221 U/L (0-40); aspartate transaminase (AST) 63 U/L (0-40); alkaline phosphatase (ALP) 280 U/L (38-155); gammaglutamyl transpeptidase (GGT) 217 U/L (15-60); total bilirubin 0.45 mg/dl (0.1-2.0); direct bilirubin 0.3 mg/dl (0.1-0.8); albumin 3.6 g/dl; C-reactive protein 9.1 mg/L (0-5); and erythrocyte sedimentation rate 40 mm/h. Serological tests for Entamoeba (hemagglutination test), HBsAg, anti-HBc IgM, anti-HCV, and anti-HIV were negative. Lung radiography and hepatic ultrasound were normal. Abdominal computed tomography and magnetic resonance imaging revealed a multi-loculated 45×70 mm cystic lesion in the corpus of the pancreas, a dilated pancreatic duct behind the cyst, and an enlargement of the body of the pancreas (Fig.). Nothing was detected in the liver or in any other organs. After albendazole 800 mg/day was initiated, the patient underwent surgery for primary pancreatic hydatid disease. Cystectomy and distal pancreatectomy were performed. Sixty milliliter of cystic fluid was removed by a injector and a scolytic agent was injected into the cyst. The scolex membrane was aspirated and a drainage catheter was inserted. Histopathological examination revealed a hydatid cyst in the corpus of the pancreas. Twenty days later, localized fluid was observed in the region of operation by abdominal ultrasonography. An ultrasonography-guided external drainage catheter was used to drain 600-700 ml liquid with a high amylase level. With suspicion of pancreatic duct injury, endoscopic retrograde cholangiopancreatography (ERCP) was performed and a pancreatic stent was placed. Shortly after ERCP, drainage from the external catheter ended and the drain was disconnected a week later. Four months later in the follow-up period the patient was doing well and was advised to return for a stent exchange.
Cystic echinococcosis is a widespread chronic endemic helminthic disease caused by metacestodes of the tapeworm Echinococcus granulosus. The vast majority of patients have single-organ involvement, and more than two thirds have only one cyst. Isolated pancreatic disease is rare and it is estimated to have a prevalence of 0.14% to 2%.[2]The mode of infestation is hematogenous, via the pancreatic or bile duct as well as the lymphatic pathway. The cyst in the pancreas is localized in the head (57%), corpus (24%) or tail (19%) of the pancreas. Clinical presentation varies according to the anatomic location of the cyst. Abdominal pain, abdominal discomfort, and vomiting are the most common clinical symptoms. The patient may present with obstructive jaundice, weight loss, an epigastric mass, and/or recurrent acute pancreatitis which may resemble a pancreatic cystic neoplasm.[3,4]Although cystotomy and drainage are the preferred treatment methods, total cystectomy is another choice if the localization of the cyst in the pancreas is appropriate for surgery. In the literature, there are cases successfully treated with distal pancreatectomy in which hydatid cysts were localized in the tail of the pancreas.[5]The longterm outcome is variable and many patients remainasymptomatic. However, percutaneous drainage may also be the choice for selected cases. Surgical or endoscopic stent replacement into the pancreatic channel is necessary if there is a connection between the cyst and the pancreatic duct. To date, there are 4 reported cases of acute pancreatitis secondary to hydatid cyst.[4,6-8]Ours was a rare case of hydatid disease causing acute pancreatitis which was localized in the pancreas and successfully treated with the combination of surgery and endoscopy.

Fig. Computed tomography showing a hydatid cyst of the pancreas.
In conclusion, pancreatic hydatidosis should be considered in the differential diagnosis of pancreatic cystic lesions associated with acute pancreatitis. Surgical, percutaneous, or endoscopic approaches alone or in combination are the therapeutic options. Medical treatment with albendazole may be preferred as chemoprophylaxis before and after drainage.
KarakaşE
Department of Radiology
Şanlıurfa Education and Research Hospital
Şanlıurfa, Turkey
Tuna Y
Department of Gastroenterology
Akdeniz University Faculty of Medicine
Antalya, Turkey
Başar Ö
Department of Gastroenterology
DışkapıEducation and Research Hospital
Ankara, Turkey
Köklü S
Department of Gastroenterology
Ankara Education and Research Hospital
Ankara, Turkey
(Email: gskoklu@yahoo.com)
1 Ozekinci S, Bakir S, Mizrak B. Evaluation of cystic echinococcosis cases given a histopathologic diagnosis from 2002 to 2007 in Diyarbakir. Turkiye Parazitol Derg 2009;33:232-235.
2 Ibis C, Albayrak D, Altan A. Primary hydatid disease of pancreas mimicking cystic neoplasm. South Med J 2009;102: 529-530.
3 Safioleas MC, Moulakakis KG, Manti C, Kostakis A. Clinical considerations of primary hydatid disease of the pancreas. Pancreatology 2005;5:457-461.
4 Ozmen MM, Moran M, Karakahya M, Coskun F. Recurrent acute pancreatitis due to a hydatid cyst of the pancreatic head: a case report and review of the literature. JOP 2005;6:354-358.
5 Moosavi SR, Kermany HK. Epigastric mass due to a hydatid cyst of the pancreas. A case report and review of the literature. JOP 2007;8:232-234.
6 Sebbag H, Partensky C, Roche J, Ponchon T, Martins A. Recurrent acute pancreatitis from the rupture of a solitary pancreatic hydatid cyst into Wirsung's canal. Gastroenterol Clin Biol 1999;23:793-794.
7 Augustin N, Gamstatter G, Neher M, Schreyer T, Storkel S. Echinococcus cysticus of the pancreas in the clinical picture of acute pancreatitis. Chirurg 1984;55:661-664.
8 Katkhouda N, Legoff D, Tricarico A, Castillo L, Bertrandy M, Mouiel J. Hydatid cyst of the pancreas responsible for chronic recurrent pancreatitis. Presse Med 1988;17:2021-2023.
Sitagliptin in treatment of diabetes complicated by chronic hepatitis C
To the Editor:
A high prevalence of glucose intolerance in patients with chronic hepatitis C has been reported,[1]and there is a significant association of chronic hepatitis C with diabetes mellitus (DM).[2]But DM has been suggested to be associated with the onset of hepatocellular carcinoma and poor prognosis of liver transplantation.[3,4]In patients with liver diseases, the management of DM is an important factor relating to prognosis. Few studies have evaluated what is the most efficacious and safe therapy for DM in chronic hepatitis patients. We treated effectively with dipeptidyl peptidase-4 (DPP-4) inhibitor, sitagliptin a 56-year-old woman with DM complicated with chronic hepatitis C.
The patient was diagnosed as having chronic hepatitis C and DM in 2008, but was not treated then. In March 2010, she was found to have a remarkably elevated plasma glucose level (712 mg/dl), and was referred subsequently to our hospital. Her height, weight, and body mass index were 150.4 cm, 42.9 kg and 19.0 kg/m2respectively. Her hemoglobin A1c level increased to 11.4% (normal range 4.3%-5.8%). The levels of serum aspartate transaminase (AST 75 IU/L, normal range 10-35 IU/L) and alanine transaminase (ALT 64 IU/L, normal range 5-40 IU/L) were also elevated. The titer of anti-hepatis C virus (HCV) antibody was 61.1 (normal range; undetectable), and the quantity of RNA for HCV genotype 1b was 7.3 (normal range; undetectable). Ultrasound examination of the liver showed chronic active hepatitis.
To reduce glucotoxicity and treat hyperglycemia, intensive insulins therapy was used with rapid-acting insulin analogue, insulin glulisine, and insulins glargine as basal insulins. Her blood glucose level was rapidly decreased, and oral anti-diabetic drugs, sulfonylurea (glimepiride, 1 mg/day) and biguanides (metformin, 750 mg/day), were prescribed. These drugs were effective in lowering the blood glucose level (Fig. A), but liverfunction deteriorated (Fig. B). At last we stopped the use of these drugs, on day 23 instead we used the DPP-4 inhibitor, sitagliptin (50 mg/day). The hypoglycemic activity of sitagliptin was comparable to that of the combination of sulfonylurea and biguanides (Fig. A), and sitagliptin did not impair liver function (Fig. B). The blood glucose level of the patient ameliorated 6 days after the use of sitagliptin.
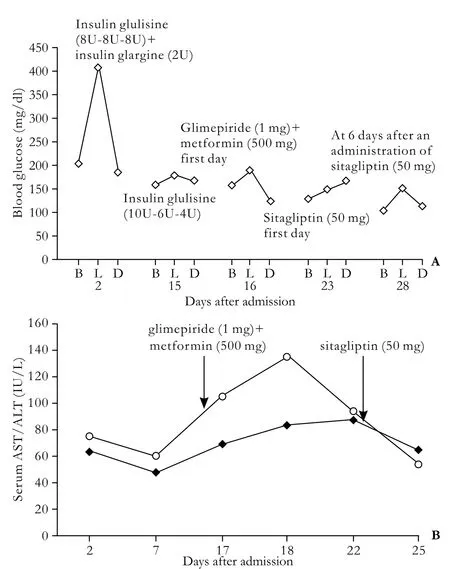
Fig. A: Changes of blood glucose levels. B, L, and D mean before breakfast (7:30), before lunch (11:30), and before dinner (18:00). B: Changes of serum AST (open circles) and ALT (black squares).
DM complicated with chronic hepatitis is difficult to treat. First, most of the oral hypoglycemic agents (sulfonylurea, biguanides, and thiazolidines) are metabolized in the liver. Second, patients with chronic hepatitis often have episodes of hypoglycemia. Inhibition by DPP-4 prevents the inactivation of glucagon-like peptide-1 (GLP-1), which increases active GLP-1, stimulates insulin secretion, and inhibits glucagon secretion.[5]These actions improve both fasting and postprandial glucose levels. Sitagliptin is highly tolerable, and there is minimal risk of hypoglycemia.[6]Further, since sitagliptin is minimally metabolized and over 80% of it is excreted in the urine, hepatic insufficiency seems not to alter its pharmacokinetics.[7]
In conclusion, DPP-4 inhibitors may be useful and safe for the treatment of DM complicated with chronic hepatitis.
Yanai H
Department of Internal Medicine
Kohnodai Hospital
National Center for Global Health and Medicine
Chiba 272-8516, Japan
Tel: +81-47-373-3501
Fax: +81-47-372-1858
Email: dyanai@hospk.ncgm.go.jp
References
1 Chen LK, Hwang SJ, Tsai ST, Luo JC, Lee SD, Chang FY. Glucose intolerance in Chinese patients with chronic hepatitis C. World J Gastroenterol 2003;9:505-508.
2 Rouabhia S, Malek R, Bounecer H. Association of hepatitis C virus infection and diabetes. World J Gastroenterol 2009;15:5114-5115.
3 Gao C, Yao SK. Diabetes mellitus: a "true" independent risk factor for hepatocellular carcinoma? Hepatobiliary Pancreat Dis Int 2009;8:465-473.
4 Xu X, Ling Q, He ZL, Gao F, Zheng SS. Post-transplant diabetes mellitus in liver transplantation: Hangzhou experience. Hepatobiliary Pancreat Dis Int 2008;7:465-470.
5 Drucker DJ, Nauck MA. The incretin system: glucagonlike peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet 2006;368:1696-1705.
6 Nauck MA, Meininger G, Sheng D, Terranella L, Stein PP; Sitagliptin Study 024 Group. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, compared with the sulfonylurea, glipizide, in patients with type 2 diabetes inadequately controlled on metformin alone: a randomized, double-blind, non-inferiority trial. Diabetes Obes Metab 2007;9:194-205.
7 Vincent SH, Reed JR, Bergman AJ, Elmore CS, Zhu B, Xu S, et al. Metabolism and excretion of the dipeptidyl peptidase 4 inhibitor [14C]sitagliptin in humans. Drug Metab Dispos 2007;35:533-538.
Liver injury associated with Malva grandifolia To the Editor:

Fig. Malva grandifolia.
Dietary supplements and herbal products are an increasingly common source of drug-induced liver injury. An increasing number of case reports have suggested causative supplement-associated liver toxicity.[1]Malva grandifoliais a plant which is frequently found in flower and vegetable gardens (Fig.). Mallow products are used as herbal medicines for gastritis as well as for ulcers of the stomach and intestines. We encountered a case of liver toxicity due toMalva grandifoliajuice, i.e. a 59-yearold woman with a medical history of hypertension. She presented to the Department of Gastroenterology with dyspepsia. She noted that she had drunkMalva grandifoliajuice (250 ml per day) for 4 weeks to control dyspeptic complaints. She took an antihypertensive drug for a long time. She denied using alcohol and the risk factors for chronic viral hepatitis were absent. Physical examination showed nothing abnormal. Her laboratory profile at admission was notable for liver injury with aspartate aminotransferase 234 IU/ml (normal <40 IU/ml), alanine aminotransferase 269 IU/ml (normal <40 IU/ml), alkaline phosphatase 335 IU/ml (normal <240 IU/ml), and gamma-glutamyl transpeptidase 66 IU/ml (normal <38 IU/ml). Albumin, bilirubin, and prothrombin time were normal. Serological markers for acute viral hepatitis were negative for anti-hepatitis A IgM, anti-hepatitis B core immunoglobulin-M, cytomegalovirus, epstein-Barr virus, herpes simplex viruses, and hepatitis B surface antigen. Hepatitis C and human immunodeficiency virus antibodies were negative. Liver ultrasound was normal. Autoimmune hepatitis markers including antinuclear antibody and smooth muscle antibody were negative with normal levels of serum immunoglobulin. These findings suspect the liver toxicity ofMalva grandifoliajuice. After giving up drinking the juice, liver enzymes normalized rapidly and were within normal limits 10 days after the first admission. Liver biopsy was not performed because the results of liver function tests were normal.
Liver toxicity due to herbal products is a rare, but well-known adverse event. An estimated 80% of the world population uses herbal medicines.[2]To our knowledge, this is the first report of hepatotoxicity caused byMalva grandifoliajuice. In conclusion, physicians should ask specifically about the use of herbal supplements, and warn patients about the potential consequences of their use. Thus patients with abnormal liver tests should also be queried in terms of herbal use.
Ekiz F, Yükselİ, BaşarÖ,ÇobanŞand Yüksel O
Department of Gastroenterology
Diskapi Yildirim Beyazit Educational and Research Hospital
Ankara, Turkey
Teber MA
Department of Radiology
Ankara Etlik Ihtisas Educational and Research Hospital
Ankara, Turkey
Tel: +903125621086
Fax: +903123186690
Email: dr_ekiz@yahoo.com
References
1 Stickel F, Patsenker E, Schuppan D. Herbal hepatotoxicity. J Hepatol 2005;43:901-910.
2 Farnsworth NR, Akerele O, Bingel AS, Soejarto DD, Guo Z. Medicinal plants in therapy. Bull World Health Organ 1985; 63:965-981.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Total laparoscopic hysterectomy after liver transplantation
- Pancreatic duct stones in patients with chronic pancreatitis: surgical outcomes
- Outcomes and mechanisms of ischemic preconditioning in liver transplantation
- Percutaneous injection of hemostatic agents for active liver hemorrhage
- Giant cell tumor of the pancreas: a pathological diagnosis with poor prognosis
- Application of a medical image processing system in liver transplantation
