胰腺癌的不典型64排螺旋CT影像表现
2010-11-23马天顺卢明智邵成伟左长京陆建平吕桃珍郑建明
马天顺 卢明智 邵成伟 左长京 陆建平 吕桃珍 郑建明
·论著·
胰腺癌的不典型64排螺旋CT影像表现
马天顺 卢明智 邵成伟 左长京 陆建平 吕桃珍 郑建明
目的分析胰腺癌的64排螺旋CT的不典型表现,以提高对该肿瘤的CT征象的认识水平。方法回顾性分析经手术病理证实的缺乏典型CT征象的12例胰腺导管腺癌的64排螺旋CT资料。结果12例均为胰腺导管腺癌。其中,中分化导管腺癌7例,中高分化导管腺癌1例;黏液腺癌1例;腺鳞癌3例。8例导管腺癌病灶中位于胰头及(或)钩突部7例,胰颈部1例,表现为等、低密度或囊实性肿块,增强后无明显强化;5例肿瘤呈明显外生性或有外生倾向;5例肿瘤远端胰管无扩张,2例出现胆总管和肝内胆管扩张,仅1例出现肿瘤远端胰腺萎缩。1例黏液腺癌CT平扫示胰头部5 cm囊性病灶,增强后仅囊性病灶下方少许实性部分轻度强化,体尾部胰管中度扩张(7 mm),胆总管及邻近血管未受侵犯。3例腺鳞癌病灶中位于胰头2例,胰体部1例,肿块最大径3.0~4.5 cm,CT增强扫描胰腺实质期示3例病灶内均见液化坏死区,病灶远端胰管均轻度扩张(4~5 mm),胆总管和肝内胆管均未见扩张。结论胰腺癌可出现不典型的CT影像表现,要注意与易混淆疾病进行鉴别诊断。
胰腺肿瘤; 体层摄影术,X线计算机; 诊断,鉴别; 癌,非典型
近年来胰腺癌发病率在国内外均呈上升趋势[1]。胰腺癌有其典型的影像学特征,但有些胰腺癌缺乏典型影像学表现,从而影响诊断。本文收集经手术病理证实的但缺乏典型影像学表现的胰腺导管腺癌病例,结合文献分析其64排CT表现,以期提高对这类胰腺癌的认识水平。
资料与方法
一、临床资料
收集2006年3月至2008年12月期间上海长海医院经手术病理及免疫组化检查确诊、经过放射科读片会讨论一致认为缺乏典型影像学表现的胰腺癌12例,其中男7例,女5例,年龄29~77岁,平均58岁。主要临床表现:腹泻伴消瘦2例次,腰背部酸胀2例次,上腹隐痛不适5例次,反复腹痛腹胀2例次,乏力1例次。3例血CA19-9水平轻中度升高,分别为84.77 U/ml、112.3 U/ml、173.2 U/ml;1例明显升高,为590.2 U/ml;余8例在正常范围。
二、影像学检查方法
应用西门子 Sensation Cardiac 64排螺旋CT扫描机,先行腹部平扫后再行胰腺三期增强扫描。增强扫描采用高压注射器经肘前静脉注射非离子型对比剂碘海醇(300 mg I/ml) 90~100 ml,注射流率为3~4 ml/s,扫描延迟时间自动触发,动脉期约为23~25 s,胰腺实质期45~50 s,门脉期60~70 s,扫描层厚0.6 mm,螺距1.2,重建层厚3 mm。
结 果
一、病理学诊断
12例均为胰腺导管腺癌。其中,中分化导管腺癌7例,中高分化导管腺癌1例,黏液腺癌1例,腺鳞癌3例。
胰腺导管腺癌肿块呈灰白、灰黄色,直径2.0~6.0 cm,瘤体常为实性,边界不清,质硬。镜下见肿瘤细胞呈腺管、腺样结构排列,细胞异型不明显,核分裂象相对较少,增殖细胞活性为中、低度。
黏液腺癌的瘤体呈实性,浸润性生长。镜下见肿瘤细胞呈立方、柱状及多边形,部分排列成不规则腺管状,部分胞质内含黏液,可有大量黏液池形成。
腺鳞癌肿块呈灰白色,部分有坏死。镜下见腺癌细胞群中混有不同数量的鳞癌细胞。肿瘤细胞圆形、卵圆形、多边形,核深染,排列成巢团状,部分呈不规则腺管样,浸润性生长。
二、中、高分化导管腺癌CT影像表现
CT平扫:7例病灶位于胰头或钩突部,1例位于胰颈部。7例表现为明显等低密度肿块,1例表现为胰头钩突等密度局部膨隆。2例肿块呈明显外生性生长(图1),3例有轻微外生性生长(图2)。肿瘤最大径2.0~6.0 cm。所有病例均未见钙化。
增强扫描:动脉期示4例病灶呈等密度,4例病灶呈相对低密度,其中2例见腹腔干或肠系膜上动脉被肿块包绕(图3)。胰腺实质期示1例病灶呈等密度,5例病灶呈低密度,2例病灶呈低密度伴结节或环形强化;5例胰体尾部胰管无扩张,2例胰体尾部胰管轻度扩张(4~5 mm),1例胰体尾部胰管中度扩张(6~7 mm);1例肝门见肿大淋巴结,1例下腔静脉后见肿大淋巴结,1例出现肿瘤远端胰腺萎缩,4例胰周脂肪间隙显模糊,2例出现胆总管和肝内胆管扩张。门脉期示1例病灶呈等密度,3例病灶呈等低密度,4例病灶呈低密度(其中2例仍伴结节或环形强化)。
三、黏液腺癌CT影像表现
黏液腺癌1例,病灶位于胰头,肿块最大径5 cm。CT平扫病灶呈囊性;增强扫描:动脉期示囊性病灶下方少许实性部分强化;实质期示病灶囊性部分不强化,实性部分轻中度强化,但低于正常胰腺实质,体尾部胰管中度扩张(7 mm),十二指肠降段受压;门脉期示病灶实性部分密度略低。胆管未见扩张,未见邻近血管受侵犯,亦未见肿大淋巴结(图4、5)。
四、腺鳞癌CT影像表现
3例腺鳞癌中,2例病灶位于胰头,1例位于胰体部,肿块最大径3.0~4.5 cm。CT平扫1例病灶呈等密度,2例呈等低密度。增强扫描:动脉期示1例病灶呈等密度,2例呈等低密度;胰腺实质期示1例病灶呈混杂略低密度,2例呈低密度,内见更低液化坏死密度(图6)。3例胰体尾部胰管均轻度扩张(4~5 mm),1例体尾部胰腺萎缩,1例十二指肠降段受压;胆总管和肝内胆管均未见扩张。
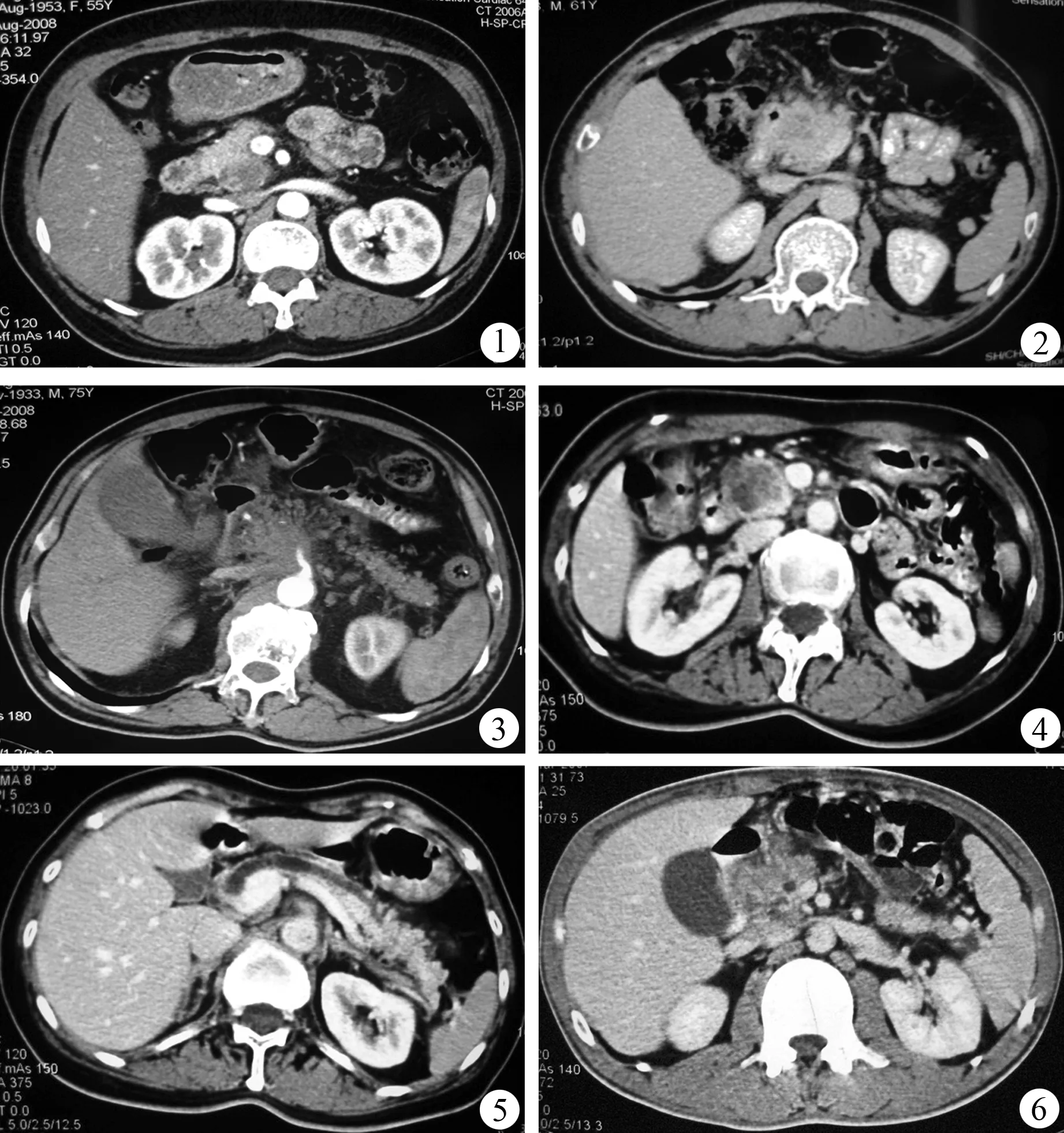
图1胰头钩突内后方外生型肿块,轻度不均匀强化,病灶边界清图2胰头轻微外生型低密度肿块,与十二指肠降部分界不清图3胰头颈后方低密度肿块,包裹肠系膜上动脉图4胰头混杂密度肿块,实性成分有强化图5病灶远端胰管全程扩张图6胰头低密度为主混杂密度肿块,内见灶性坏死区
讨 论
典型胰腺导管腺癌的CT影像学直接征象为胰腺实质性肿块,呈等密度或略低密度,肿块较大时内部可出现液化坏死的低密度;增强扫描表现为强化不明显的低密度灶,肿瘤远端胰腺萎缩,远端胰管扩张。间接征象:(1)胰头部肿块导致胰胆管梗阻形成的“双管征”;(2)胰周尤其是胰后脂肪间隙模糊,腹膜后淋巴结肿大;(3)邻近血管、神经受累。
近年来随着影像学检查手段的发展,典型胰腺导管腺癌诊断一般不难。但对于一些不典型的胰腺癌影像学表现,则容易误诊。本文报道的12例不典型胰腺导管腺癌CT征象主要有:(1)胰腺癌呈外生性或具有外生性倾向,围管浸润特性不明显,远端胰管不扩张或轻度扩张,胆总管多不受影响。但有2例胰头肿块侵犯十二指肠降部,2例侵犯肠系膜上动脉根部,仍然表现出恶性肿瘤的生物学特性,在鉴别诊断上具有较大的价值。而且75%~90%的胰腺
导管腺癌在CT增强扫描中呈低密度影[2-4]。胰腺实质期,呈相对低密度,有利于清晰地发现病灶。(2)黏液腺癌可呈囊性,而实性成分极少。CT增强扫描表现为不强化囊性密度,容易误诊为囊腺瘤或者胰腺导管内乳头状黏液性肿瘤(IPMT)[5]。(3)腺鳞癌表现为肿瘤体积较小,边界一般清晰,病灶内出现液化坏死低密度区。这是其较特征性的影像表现。(4)肿块强化与胰腺实质强化对比不明显。CT平扫,肿瘤呈现等密度或夹杂灶性低密度;延迟增强扫描,肿瘤强化,与胰腺实质强化对比不明显,故仅表现为胰腺局部轮廓膨大,容易漏诊[6]。需要与胰腺导管腺癌鉴别的有:(1)肿块型胰腺炎。肿块型胰腺炎多数有慢性胰腺炎病史,胰头增大、饱满,胰周纤维素样索条及肾周筋膜增厚,增强扫描胰腺实质期至延迟期密度趋向一致,有“慢进慢出”的特点,有时可见微小钙化或胰管穿过并狭窄。(2)IPMT。分支胰管型IPMT表现为胰头葡萄串样囊性病灶与扩张主胰管相通,病灶以囊性为主,实性成分较少或者仅可见囊性成分。主胰管型IPMT可见主胰管明显扩张(>1 cm),无明显胰腺实质萎缩、胰腺钙化或胰管结石。ERCP结合超声内镜穿刺活检有助于病变的定性。(3)胰腺囊性肿瘤。胰腺囊腺瘤(或癌)多体积较大,内有分隔和壁结节可强化,典型者出现轮辐状钙化。除了囊腺癌外,远端胰管几乎无扩张。
[1] 李兆申,潘雪.胰腺癌的流行病学、病因学和发病机制.胃肠病学,2004,9:101-103.
[2] 胡先贵,邵成浩,胡志浩,等.胰腺腺鳞癌9例临床分析.胰腺病学,2001,1:15-17.
[3] Lu DS,Vedantham S,Krasny RM,et al.Two-phase helical CT for pancreatic tumors:pancreatic versus hepatic phase enhancement for tumor,pancreas,and vascular structures.Radiology,1996,199:697-701.
[4] Boland GW,O′Malley ME,Saez M,et al.Pancreatic-phase versus portal vein-phase helical CT of the pancreas:optimal temporal window for evaluation of pancreatic adenocarcinoma.AJR Am J Roentgenol,1999,172:605-608.
[5] 席鹏程,胡先贵,刘瑞,等.胰腺黏液性非囊性癌12例诊治经验.中华外科杂志,2004,42:504-506.
[6] 许相丰,杨津毅,张增利,等.等密度胰腺癌的多层螺旋CT诊断.中国临床医学影像杂志,2007,18:468-470.
2010-02-22)
(本文编辑:屠振兴)
Atypical64slicespiralCTimagingfindingsofpancreaticcancer
MATian-shun,LUMing-zhi,SHAOCheng-wei,ZUOChang-jing,LUJian-ping,LVTao-zhen,ZHENGJian-ming.
DepartmentofRadiology,HospitalofZhongzhouAluminumFactory,Xinxiang453834,China
Correspondingauthor:SHAOCheng-wei,Email:cwshao@sina.com
ObjectiveTo analyze atypical 64-slice spiral CT imaging findings of pancreatic cancer and to improve the ability to identify CT manifestations of pancreatic cancer.MethodsA retrospective analysis was performed on the atypical 64-slice spiral CT imaging findings of 12 cases of pancreatic cancer confirmed by pathology after surgery.ResultsAll the twelve cases were pancreatic ductal adenocarcinoma. Among them, 7 cases were moderately differentiated ductal adenocarcinoma, 1 case was well-differentiated ductal adenocarcinoma, 1 case was mucinous adenocarcinoma, 3 cases were adenosquamous carcinoma. Among 8 cases with ductal adenocarcinoma, the lesions were located in the pancreatic head and (or) uncinate process in 7 cases, and in the pancreatic neck of 1 case. Tumors were expressed as isodense or low-density or cystic-solid lesions, the masses showed no enhancement in the enhanced scanning phase. Tumors were clearly exogenous or exogenous tendencies in 5 cases. Five cases had no distal pancreatic duct dilation, 2 patients had common bile duct and intrahepatic biliary dilation, and only 1 patient had atrophy of distal pancreas. There was one case of mucinous carcinoma, plain CT scan showed a cystic lesion in head of pancreas about 5cm in diameter, the solid part below the cystic lesion was slightly enhanced in the enhanced scanning phase and the body and tail pancreatic duct was moderately dilated (7 mm). There was no common bile duct and adjacent blood vessels invasion. Among 3 cases of adenosquamous carcinoma, lesions were located in the pancreatic head of 2 cases and in pancreatic body of 1 case. The maximal diameter of mass ranged 3.0 cm~4.5 cm. Cystic necrotic area was observed within the lesions in 3 cases in enhanced pancreatic parenchymal phase of CT scan. Distal pancreatic duct were mildly dilated (4~ 5 mm) in 3 cases. There was no common bile duct and intrahepatic bile duct dilation.ConclusionsPancreatic cancer may show atypical CT imaging findings and great cautions are needed for differential diagnosis.
Pancreatic neoplasms; Tomography, X-ray computed; Diagnosis,differential; Cancer, atypical
10.3760/cma.j.issn.1674-1935.2010.03.009
453834 新乡,河南省新乡市中州铝厂医院放射科(马天顺,原长海医院放射科进修生);长海医院放射科(邵成伟、陆建平、吕桃珍),放疗科(卢明智),核医学科(左长京),病理科(郑建明)
邵成伟,Email:cwshao@sina.com