急性外侧踝扭伤保守治疗的研究进展
2023-06-26邹庆芳邵宏斌许杰男董晨辉马东洋
邹庆芳 邵宏斌 许杰男 董晨辉 马东洋
【摘要】 急性外侧踝扭伤(LAS)是生活中的常见损伤,多见于运动量大的青壮年,常因行走或运动过程中,踝关节突然发生内翻暴力所致,若早期不重视将导致慢性踝关节疼痛及不稳的概率较大,给人们的身体健康、社会生产生活带来了极大的负面影响;目前LAS主要采取保守治疗,而对于合并严重的骨折及其他严重并发症的患者多采用手术治疗。本文通过查阅国内外最新文献,对急性LAS的诊断、保守治疗、康复及预防进行了详细论述,以期提高LAS的早期诊断,减少晚期并发症的发生。
【关键词】 踝关节外侧副韧带 急性损伤 保守治疗
[Abstract] Acute lateral ankle sprain (LAS), as a common injury, is common in young and middle-aged people with heavy physical activity. It is often caused by ankle pronation during walking or sports. If not taken seriously in the early stage, it will lead to a higher probability of chronic ankle pain and instability, which has a great negative impact on people's physical health and social production and life; at present, LAS is mainly treated conservatively, and surgical treatment is often used for patients with severe fractures and other serious complications. By reviewing the latest literature at home and abroad, the diagnosis, conservative treatment, rehabilitation and prevention of acute LAS are discussed in detail to improve the early diagnosis and reduce the occurrence of late complications.
[Key words] Lateral collateral ligament of ankle joint Acute injury Conservative treatment
First-author's address: First Clinic Medical School, Gansu University of Chinese Medicine, Lanzhou 730000, China
doi:10.3969/j.issn.1674-4985.2023.15.043
急性踝扭伤(acute ankle sprain,AAS)是肌肉骨骼系统最常见的损伤之一,占所有运动相关损伤的16%~40%[1-2],而外侧踝关节扭伤(lateral ankle sprain,LAS)是最常见的踝关节扭伤类型[3-4]。因此正确治疗LAS显得极其重要,若未及时、正确的处理,可能会导致踝关节反复扭伤、不稳,最终导致慢性踝关节不稳(chronic ankle instability,CAI)[5-7],并隨着CAI患者的功能下降,从而发生创伤后骨关节病,进而影响人们的工作和生活[8]。目前,保守治疗在大多数LAS患者中取得了很好的效果。本文就急性LAS的保守治疗进行综述,为LAS的科学预防及诊疗提供参考。
1 外侧踝关节的解剖特点
踝关节的骨性结构包括胫骨、腓骨和距骨;其腱性结构主要由外侧韧带、内侧三角韧带和胫腓联合韧带组成。踝关节外侧韧带的复合体由三条韧带组成:距腓前韧带(anterior talofibular ligament,ATFL)、跟腓韧带(calcaneofibular ligament,CFL)和距腓后韧带(posterior talofibular ligament,PTFL)。ATFL的起源位于腓骨前缘,距离外踝下尖约13.8 mm,向前下延伸至距骨颈部[9];CFL起源于外踝下尖前方约5.3 mm,向后下插入跟骨外侧结节[9];PTFL的起源位于外踝内侧的外踝下尖端上约4.8 mm,其纤维扩散到距骨的后外侧[9]。
2 外侧踝关节损伤机制
ATFL、CFL和PTFL是维持外侧踝关节稳定重要结构。ATFL在跖屈时绷紧,可防止距骨前移位和跖屈过度[10],ATFL是外侧韧带复合体中最弱的韧带,也是最常受伤的韧带,通常在足底屈曲和内翻时发生,约占LAS的70%[11];在对人类踝关节韧带的生物力学研究中,与CFL(345.7 N)和PTFL(261.2 N)相比,ATFL表现出最低的失效负荷(138.9 N)[12]。CFL在背屈时绷紧,可防止距下和滑骨关节过度后旋、内翻和内旋[10];PTFL在背屈时也绷紧,有助于防止脚踝过度内旋和倒置[13],PTFL很少受到影响,通常只有在踝关节脱臼等严重损伤后才会破裂[14]。
3 诊断标准
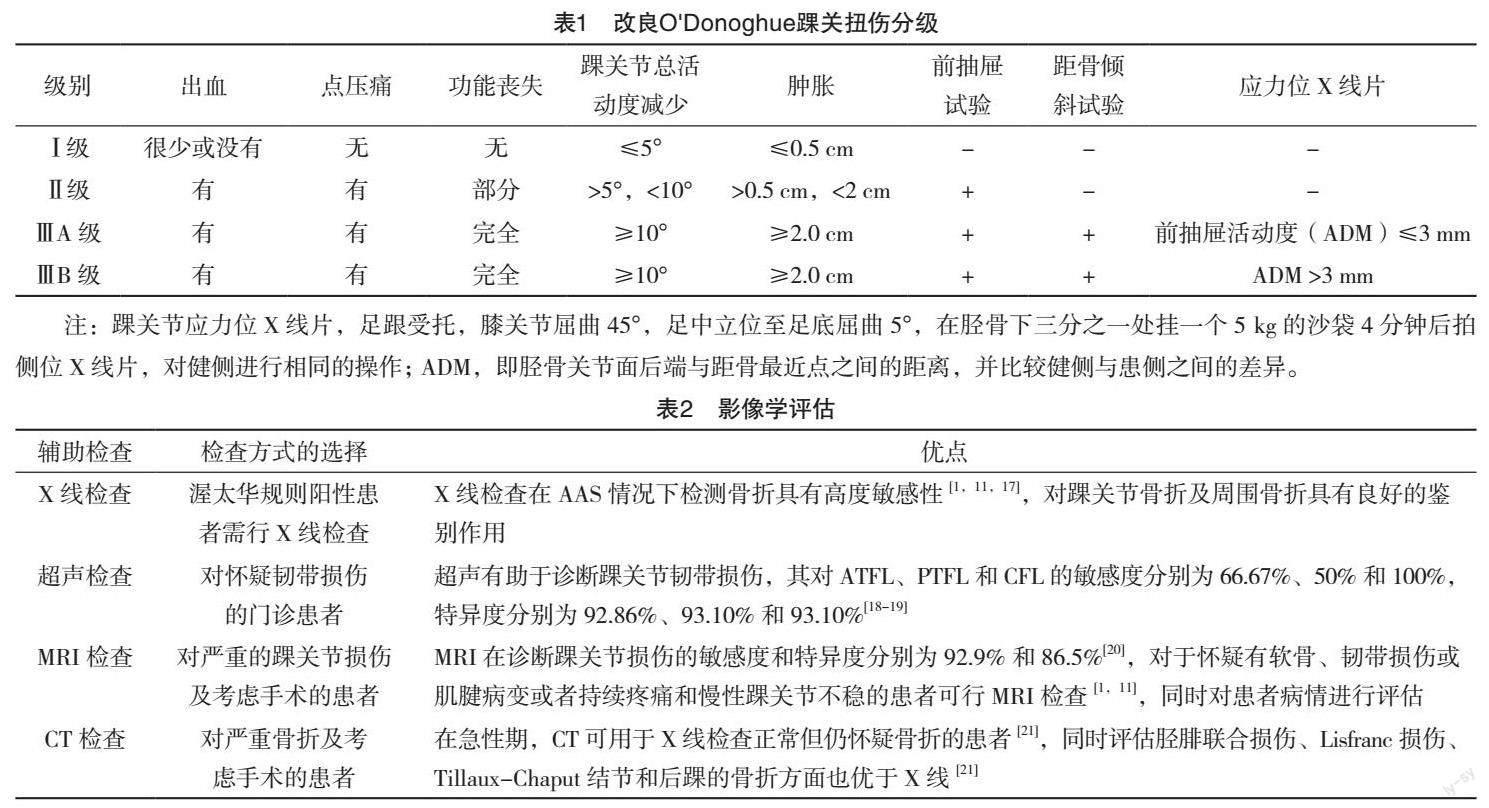
3.1 损伤分级 临床上根据O'Donoghue分类可分为Ⅰ级或轻度损伤:轻微的韧带拉伤,出血很少,没有造成松弛或不稳,踝关节完整的功能和强度得以保持。Ⅱ级或中度扭伤:韧带的不完全撕裂,轻度松弛和不稳定,功能轻微下降,力量可能下降,并可能失去本体感觉。Ⅲ级或严重扭伤:韧带完全断裂,严重不稳定和松弛,并可能丧失全部功能、力量以及本体感觉[1,11]。O'Donoghue分类主要体现在韧带的损伤程度,缺乏对踝关节的症状和体征评价,有研究通过患者的查体及影像学检查对踝关节扭伤严重程度进行改良[1,15](表1)。
3.2 症状和体征 初次扭伤的患者症状往往比较明显,出现踝关节疼痛、肿胀、点压痛、瘀斑和活动受限等[1,11]。急性损的患者因疼痛、肿胀,查体不易完成,经局部麻醉止痛后可能查出前抽屉试验、距骨倾斜试验、Kleiger外旋试验阳性等[1,11]。检查时须与对侧正常关节进行对比,防止因其他原因的关节松弛导致误判。
3.3 影像学评估 渥太华踝关节规则已被证明在预测踝关节损伤的患者需要X射线来排除骨折方面是准确的[16]。渥太华踝关节规则建议,应在踝部疼痛和以下任何情况下获取踝关节X光片[1]:(1)外踝末端6厘米处或末端后缘有压痛;(2)内踝末端6厘米处的后缘或末端有压痛;(3)在受伤后无法立即负重行走4步。足部系列适用于中足疼痛和以下任何一种症状的患者:(1)第五跖骨底部触痛;(2)舟骨触痛;(3)受伤后无法立即承重,并无法行走4步。这些规则部适用于注意力分散、中毒、下肢感觉障碍/减弱及头部损伤或其他导致合作困难的患者。一个典型的踝关节X线系列包括前后位、侧位和榫眼位。足部序列的标准视图包括前后位、侧位和斜位。对于LAS的患者可通过影像学评估来决定后续的诊疗措施,其对踝关节损伤的敏感度及特异度也有差异(表2),临床医师可根据患者实际情况进行选择。
4 治疗策略
LAS的治疗策略可根据踝关节扭伤分级来决定。临床医生普遍认为Ⅰ~Ⅱ级损伤通过非手术治疗恢复迅速且预后良好,Ⅲ级损伤的治疗目前具有争议,一些人更倾向于一期手术修复,另一些人则更倾向于保守治疗,但严重的Ⅲ级踝关节损伤或者保守治疗效果不佳的患者可考虑手术、制动和功能治疗[14,22-23]。主要目的是预防后遗症及快速恢复。
4.1 保守疗法
4.1.1 保护、休息、冰敷、压迫和抬高(protection,rest,ice,compression,elevation,PRICE) 对LAS的早期治疗普遍应用PRICE的原则[1,24]。然而,支持这种方法的证据是有限的。Vuurberg等[2]回顾并汇总了33项研究冷冻疗法治疗急性踝关节扭伤效果的随机对照试验的数据,发现在休息时的疼痛、功能或肿胀等症状无明显改善。Bendahou等[25]进行的一项多中心随机对照试验比较了弹力袜与非加压安慰剂袜的使用,发现在疼痛、镇痛剂消耗或双踝或中足周长未观察到显著差异。目前还没有单独的对照试验检验休息或抬高法治疗急性踝关节扭伤的疗效。尽管如此,在踝关节扭伤急性期使用PRICE治疗仍是一种合理且常用的干预措施[2,11]。
4.1.2 镇痛 口服和外用非甾体抗炎药(nonsteroidal anti-inflammatory drugs,NSAID)可减轻急性期疼痛。NSAID通过抑制环加氧酶、减少前列腺素和血栓烷下游产物起作用,从而达到抗炎和止痛效果[26]。尽管NSAID通常被认为是安全,但由于NSAID抑制组织损伤的正常炎症反应而延迟组织愈合[1,11],在LAS后的前14 d,对乙酰氨基酚是一种同样有效的减轻疼痛的替代药物[2,11]。
4.1.3 固定 根据目前的证据,早期活动和功能性踝关节支持优于刚性制动,特别是对于Ⅰ级和Ⅱ级损伤[2,27],一项随机对照试验表明,使用功能性支持治疗的运动员比使用石膏固定的运动员更早地恢复体育活动,并且他们在受伤后3~6个月发生的不适症状更少[28]。然而,一些证据表明,短期内(少于10 d)使用石膏或刚性支具固定对Ⅲ级踝关节扭伤可减轻疼痛、肿胀和改善功能[11,29]。目前没有试验证明内侧踝扭伤的早期制动的疗效;然而,由于担心早期活动范围可能会导致二次伤害,大多数专家建议制动和保护负重时间不超过2周[30]。
4.1.4 手法治疗 在LAS的康复计划中加入手法治疗可能有助于减轻疼痛和功能恢复。Loudon等[31]回顾了八项利用手法治疗的对照试验,并得出结论:在踝关节扭伤损伤的急性期应用手法治疗可减轻疼痛并增加踝背屈活动度。Cleland等[32]的另一项随机对照试验发现,在物理治疗方案中增加手法治疗方案,通过在急性LAS患者长达6个月的随访中发现,踝关节功能测量、下肢功能量表评分和疼痛评分得到更大改善。基于这些发现,我们建议将手法治疗纳入踝关节扭伤康复计划中。
4.1.5 伤后神经肌肉训练 神经肌肉和本体感觉训练计划是对踝关节康复计划的安全有效的补充,在受伤后应尽快实施。踝关节损伤后神经肌肉激活模式的改变会导致功能不稳定、步态改变和复发性损伤风险增加[33]。与传统的PRICE疗法相比,在损伤后越早实施神经肌肉训练能够提高总体活动水平,而不增加疼痛、肿胀或再损伤率[34]。Postle等[35]的系统综述和荟萃分析发现本体感觉练习能够显著改善踝关节功能评分,神经肌肉训练同时还能降低了复发性损伤和功能不稳定的发生率。因此,建议踝扭伤的运动员进行早期神经肌肉训练。
4.2 传统医学 传统医学中主要以消肿止痛、化瘀止血为原则,通常包括内服、外敷及针灸推拿等方式治疗。一项随机对照试验研究发现,肿痛消汤能有效缓解LAS患者的症状和体征[36]。有研究利用伤科接骨片联合石氏伤科熏洗剂治疗踝关节外侧副韧带损伤,发现采用中医药熏洗结合伤科接骨片内服,能够温经通络,活血、健骨养筋,同时还能促进组织修复,有效缓解踝关节的肿痛,从而促进患者进行主动及被动的功能训练[37]。常立仁[38]通过五步正踝法治疗急性踝关节外侧副韧带损伤临床效果观察后认为,五步正踝法可以消除踝关节肿痛,促进踝关节外侧副韧带的修复,改善患者的生活质量。
5 预防脚踝扭伤和复发性损伤
5.1 支撑和保护 使用支具或踝套都是预防首次和复发性踝关节扭伤的有效方法[2,39]。这些干预措施将再次扭伤的风险降低50%~70%[40-41]。一项大型随机对照试验证明:在使用系带式踝關节支具可降低男性和女性高中篮球运动员首次和复发性踝关节扭伤的发生率[42],脚踝扭伤后一年内佩戴脚踝支具或踝套,可有效防止再次受伤[11]。因此,我们建议在脚踝扭伤后一年内佩戴支具或踝套,以防止再次受伤。
5.2 神經肌肉训练计划 神经肌肉训练计划通常包括平衡感和本体感觉,在锻炼过程中反复进行有意或无意的不稳定练习。这些项目改善了踝关节位置感、肌肉反应时间和功能结果评分[43]。它们可以降低急性踝关节扭伤后12个月内踝关节扭伤的复发率,并且应该在所有遭受踝关节扭伤的患者伤后尽快开始锻炼[2]。尽管对预防复发性扭伤有效,但通过神经肌肉训练项目降低首次踝关节扭伤率的证据并不充分,Foss等[44]进行了一项前瞻性随机对照研究,在初中和高中年龄的运动员中实施神经肌肉训练计划,并发现总体损伤率降低,但在个体踝关节损伤方面没有显著差异。
6 缺点和不足
本文主要对急性踝关节韧带损伤的诊断、治疗及预防措施进行了详细论述,但对于合并骨折的LAS并未做详细的论述,后期应完善相关的论述。
7 总结与建议
结合最新文献,本文对LAS的早期诊断、保守治疗及预防措施进行了详细论述。对于LAS我们对比归纳了现有的几种治疗方案后,建议在急性踝关节早期应用石膏/支具固定10 d,同时联合PRICE治疗,之后更换踝套并行功能锻炼,踝套连续佩戴1年,对于急性Ⅲ级损伤的运动员或合并骨折的患者可以考虑手术治疗。
参考文献
[1] HALABCHI F,HASSABI M.Acute ankle sprain in athletes: clinical aspects and algorithmic approach[J].World Journal of Orthopedics,2020,11(12):534.
[2] VUURBERG G,HOORNTJE A,WINK L M,et al.Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline[J].British Journal of Sports Medicine,2018,52(15):956.
[3] ROOS K G,KERR Z Y,MAUNTEL T C,et al.The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports[J].The American Journal of Sports Medicine,2017,45(1):201-209.
[4] MAUNTEL T C,WIKSTROM E A,ROOS K G,et al.The epidemiology of high ankle sprains in National Collegiate Athletic Association sports[J]. The American Journal of Sports Medicine,2017,45(9):2156-2163.
[5] WANG D Y,JIAO C,AO Y F,et al.Risk factors for osteochondral lesions and osteophytes in chronic lateral ankle instability: a case series of 1169 patients[J].Orthop J Sports Med,2020,8(5):2325967120922821.
[6] AICALE R,MAFFULLI N.Chronic lateral ankle instability: topical review[J].Foot & Ankle International,2020,41(12):1571-1581.
[7]王玺,冯康虎,申建军.踝关节外侧副韧带急性损伤的治疗现状[J].甘肃医药,2017,36(12):1014-1017,1023.
[8] DONOVAN L,HETZEL S,LAUFENBERG C R,et al.Prevalence and impact of chronic ankle instability in adolescent athletes[J].Orthopaedic Journal of Sports Medicine,2020,8(2):2325967119900962.
[9] CLANTON T O,CAMPBELL K J,WILSON K J,et al.Qualitative and quantitative anatomic investigation of the lateral ankle ligaments for surgical reconstruction procedures[J/OL]. Journal of Bone and Joint Surgery,2014,96(12):e98. https://pubmed.ncbi.nlm.nih.gov/24951749/.
[10] GOLANO P,VEGA J,DELEEUW P A,et al.Anatomy of the ankle ligaments: a pictorial essay[J].Knee Surgery, Sports Traumatology, Arthroscopy,2010,18(5):557-569.
[11] CHEN E T,MCINNIS K C,BORG-STEIN J.Ankle sprains: evaluation, rehabilitation, and prevention[J].Current Sports Medicine Reports,2019,18(6):217-223.
[12] ATTARIAN D E,MCCRACKIN H J,DEVIT D P,et al.A biomechanical study of human lateral ankle ligaments and autogenous reconstructive grafts[J].The American Journal of Sports Medicine, 1985,13(6):377-381.
[13] HERTEL J.Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability[J]. Journal of Athletic Training,2002,37(4):364.
[14] POLZER H,KANZ K G,PRALL W C,et al.Diagnosis and treatment of acute ankle injuries: development of an evidence-based algorithm [J/OL].Orthopedic Reviews,2012,4(1):e5.https://pubmed.ncbi.nlm.nih.gov/22577506/.
[15] MALLIAROPOULOS N,PAPACOSTAS E,PAPALADA A,et al.Acute lateral ankle sprains in track and field athletes: an expanded classification[J].Foot and Ankle Clinics,2006,11(3):497-507.
[16] KERKHOFFS G M,ROWE B H,ASSENDELFT W J,et al.Immobilisation and functional treatment for acute lateral ankle ligament injuries in adults[J].Cochrane Database of Systematic Reviews,2002,3(3):CD003762.
[17] BECKENKAMP P R,LIN C-W C,MACASKILL P,et al.Diagnostic accuracy of the Ottawa Ankle and Midfoot Rules: a systematic review with meta-analysis [J]. British Journal of Sports Medicine,2017,51(6):504-510.
[18] ESMAILIAN M,ATAIE M,AHMADI O,et al.Sensitivity and specificity of ultrasound in the diagnosis of traumatic ankle injury[J].Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences,2021,26(1):14.
[19] BALTES T,ARNAIZ J,GEERTSEMA L,et al.Diagnostic value of ultrasonography in acute lateral and syndesmotic ligamentous ankle injuries[J].European Radiology,2021,31(4):2610-2620.
[20] CHUN D I,CHO J H,MIN T H,et al.Diagnostic accuracy of radiologic methods for ankle syndesmosis injury: a systematic review and meta-analysis[J].Journal of Clinical Medicine,2019,8(7):968.
[21] VAN D,BEKEROM M P J.Diagnosing syndesmotic instability in ankle fractures[J].World Journal of Orthopedics,2011,2(7):51.
[22] LYNCH S A,RENSTROM P A.Treatment of acute lateral ankle ligament rupture in the athlete[J].Sports Medicine,1999,27(1):61-71.
[23] D'HOOGHE P,ALKHELAIFI K,ABDELATIF N,et al.From "low" to "high" athletic ankle sprains: a comprehensive review[J].Operative Techniques in Orthopaedics,2018,28(2):54-60.
[24] TRAN K,MCCORMACK S.Exercise for the treatment of ankle sprain: a review of clinical effectiveness and guidelines[J/OL]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health 2020 Apr 3. https://pubmed.ncbi.nlm.nih.gov/33074633/.
[25] BENDAHOU M,KHIAMI F,SAIDI K,et al.Compression stockings in ankle sprain: a multicenter randomized study[J].The American Journal of Emergency Medicine,2014,32(9):1005-1010.
[26] STRUIJS P A,KERKHOFFS G M.Ankle sprain: the effects of non-steroidal anti-inflammatory drugs[J].BMJ Clinical Evidence,2015,2015:1115.
[27] NAEEM M,RAHIMNAJJAD M K,RAHIMNAJJAD N A,et al.Assessment of functional treatment versus plaster of Paris in the treatment of grade 1 and 2 lateral ankle sprains[J].Journal of Orthopaedics and Traumatology,2015,16(1):41-46.
[28] ARDEVOL J,BOLIBAR I,BELDA V,et al.Treatment of complete rupture of the lateral ligaments of the ankle: a randomized clinical trial comparing cast immobilization with functional treatment[J].Knee Surgery, Sports Traumatology, Arthroscopy, 2002,10(6):371-377.
[29] VUURBERG G,ALTINK N,RAJAI M,et al.Weight, BMI and stability are risk factors associated with lateral ankle sprains and chronic ankle instability: a meta-analysis[J].Journal of ISAKOS,2019,4(6):313-327.
[30] KNAPIK D M,TREM A,SHEEHAN J,et al.Conservative management for stable high ankle injuries in professional football players[J].Sports Health,2018,10(1):80-84.
[31] LOUDON J K,REIMAN M P,SYLVAIN J.The efficacy of manual joint mobilisation/manipulation in treatment of lateral ankle sprains: a systematic review[J].British Journal of Sports Medicine,2014,48(5):365-370.
[32] CLELAND J A,MINTKEN P,MCDEVITT A,et al.Manual physical therapy and exercise versus supervised home exercise in the management of patients with inversion ankle sprain: a multicenter randomized clinical trial[J].Journal of Orthopaedic & Sports Physical Therapy,2013,43(7):443-455.
[33] PUNT I M,ZILTENER J-L,LAIDET M,et al.Gait and physical impairments in patients with acute ankle sprains who did not receive physical therapy[J].PM&R,2015,7(1):34-41.
[34] BLEAKLEY C M,O'CONNOR S R,TULLY M A,et al.Effect of accelerated rehabilitation on function after ankle sprain: randomised controlled trial[J].BMJ,2010,340(7756):1122.
[35] POSTLE K,PAK D,SMITH T.Effectiveness of proprioceptive exercises for ankle ligament injury in adults: a systematic literature and meta-analysis[J].Manual Therapy,2012,17(4):285-291.
[36]譚小平.肿痛消汤治疗早期踝关节外侧韧带损伤90例临床观察[J].中医药导报,2011,17(1):63-65.
[37]徐震球.伤科接骨片联合石氏伤科熏洗剂治疗踝关节外侧副韧带损伤40例临床观察[J].中医药导报,2016,22(2):64-66.
[38]常立仁.五步正踝法治疗急性踝关节外侧副韧带损伤临床疗效观察[J/OL].中西医结合心血管病电子杂志,2020,8(16):137.https://kns-cnki-net-443.webvpn.gszy.edu.cn/kcms/detail/detail.aspx?FileName=ZXJH202016108&DbName=CJFQ2020.
[39] BARELDS I,VAN DEN BROEK A G,HUISSTEDE B.Ankle bracing is effective for primary and secondary prevention of acute ankle injuries in athletes: a systematic review and meta-analyses[J].Sports Medicine,2018,48(12):2775-2784.
[40] MCKEON P O,MATTACOLA C G.Interventions for the prevention of first time and recurrent ankle sprains[J].Clinics in Sports Medicine,2008,27(3):371-382.
[41] KAMINSKI T W,NEEDLE A R,DELAHUNT E.Prevention of lateral ankle sprains[J].Journal of Athletic Training,2019,54(6):650-661.
[42] MCGUINE T A,BROOKS A,HETZEL S.The effect of lace-up ankle braces on injury rates in high school basketball players[J].The American Journal of Sports Medicine,2011,39(9):1840-1848.
[43] ZECH A,HUEBSCHER M,VOGT L,et al.Neuromuscular training for rehabilitation of sports injuries: a systematic review[J].Med Sci Sports Exerc,2009,41(10):1831-1841.
[44] FOSS K D B,THOMAS S,KHOURY J C,et al.A school-based neuromuscular training program and sport-related injury incidence: a prospective randomized controlled clinical trial[J].Journal of Athletic Training,2018,53(1):20-28.
(收稿日期:2023-02-03) (本文編辑:占汇娟)
