中医药影响新型冠状病毒肺炎密接者转阳率的研究:一项大样本队列研究
2023-01-31王晓骁窦莉邹冲吴拥军王威赵晶晶于茜沈照峰倪平敏章雯陆亚文奚肇庆方祝元
王晓骁, 窦莉, 邹冲, 吴拥军, 王威, 赵晶晶, 于茜, 沈照峰, 倪平敏, 章雯, 陆亚文, 奚肇庆,方祝元
(南京中医药大学附属医院,江苏 南京 210023)
The severe acute respiratory syndrome corona-virus 2 (SARS-CoV-2) is a rapidly emerging virus causing corona-virus disease 2019 (COVID-19) and the global pandemic since the outbreak in Wuhan, China in late 2019[1-2]. Current strategies to protect oneself include getting vaccines, ensuring personal hygiene, using face masks, and practicing social distancing[1]. With constant mutations of the virus, multiple variants of concern (VOC) continue to emerge. The Delta variant (also referred to as B.1.617.2) appears to spread more easily than other variants. It is characterized by increased transmissible, shorter incubation period, stronger pathogenic, faster progression, and higher risks to cause severe illness[3]. It was once the predominant variant of the virus worldwide, which was already predicted by the WHO in July that the Delta variant was expected to be the main strain in the world in the upcoming months[3]. Due to its high infectivity, a rebound in cases has occurred in multiple countries and territories in the past year.
The outbreak in Nanjing, China since July 2021, which spread to Yangzhou, was caused by Delta variant. Since then, a large number of local residents were under quarantine in centralized medical quarantine sites since the standard of care is to observe and quarantine for 14 days as the incubation period[4]. However, there were no specific interventions carried out onto these population. In order to implement national and provincial requirements trying to prevent people from getting sick and treat the disease and to maximize the effect of Chinese medicine based on previous experiences to control the spread in Guangdong, China, Chinese medicine is encouraged to use for its effectiveness in the treatment of COVID-19[5-7].
TCM is a treasure of ancient Chinese medicine with a history of more than 2 000 years and rich experience. Evidence from clinical trials showed that TCM can effectively treat several chronic diseases, such as cerebral infarction and chronic kidney disease. TCM is beneficial for immunity, antivirus, anti-inflammatory and relieved side effects. During last two years, the advantages of TCM for the treatment of COVID-19 have been found, including delay the disease progression from mild and moderate to severe. Some mild symptoms like cough or dizziness could be treated with TCM. In addition, WHO expert meeting confirmed Chinese medicine (TCM) in the treatment of COVID-19. In China, TCM could shorten the time of nucleic acid turning negative and reduce the possibility of disease exacerbation. Importantly, fewer adverse events related to TCM were founded. Lianhua Qingwen capsule has been recommended to treat COVID-19 patients with mild symptoms, which could reduce the fever time. Studies shown TCM could improve immune function and hypoxia resistance, protect pulmonary micro-vascular endothelial cells, and inhibit pulmonary fibrosis, which is suitable for the pathological changes of lung tissue injury.
1 METHODS
1.1 Participants
An estimate of at least 5 000 residents who had a recent history of close-contact exposure to a case patient of COVID-19 under centralized quarantine in Jiangsu Province were included based on tripartite database. Participants were excluded if they were confirmed cases of COVID-19, while pregnant or breastfeeding, had complications of severe primary heart, lung, kidney, blood, or other diseases affecting survival, or with psychiatric, cognitive impairment, or legally disabled. Statisticians and main researchers shall determine whether the participants should be eliminated who did not meet inclusion criteria but met exclusion criteria before statistical analysis started.
1.2 Study Design and Oversight
This was an retrospective cohort study, and data of close contacts in centralized medical quarantine sites in Yangzhou, China from August 4 to September 5, 2020 was collected. Study candidates were screened using tripartite database (pharmaceutical database, Yangzhou on-site database, and provincial CDC database) to explore the efficacy of TCM in prevention of COVID-19. Tripartite database first underwent matching, cleaning, and desensitizing (removing identifiable personal information), and was later performed on mining and analysis.
A query list was provided in case of any question. The researchers shall answer the questions in the query list and review each copy of electronic document. The database would be locked once the data verification report was completed. Any documents related to quality control need to be filed, such as data consistency verification, original records of numerical range and logical check, original records of blind audit, and query records of communication between researchers.
1.3 Exposure
The exposure (main strategies) was the use of TCM (including Qingfei Paidu Decoction and Fuzhengyiqing prescription) in the prevention of COVID-19 among close contact in various parts of Jiangsu Province, twice a day for 6 days. Close contacts without using TCM were considered control group.
Qingfei Paidu Decoction composes of 21 herbs, which are Ma huang (EphedraHerba) 9 g, Zhi gan cao 6 g, Ku xing ren (AmygdalusCommunisVas) 9 g, Sheng shi gao 15-30 g, Gui zhi (CinnamomiRamulus) 9 g, Ze xie (AlismaOrientaleJuz.) 9 g, Zhu ling (PolyporusUmbellatusFr.) 9 g, Bai zhu (AtractylodesMacrocephalaKoidz.) 9 g, Fu ling (PoriaCocosWolf.) 15 g, Bei chai hu 16 g, Huang qin (ScutellariaeRadix) 6 g, Jiang ban xia 9 g, Ginger (ZingiberOfficinaleRoscoe) 9 g, Zi wan (AsterisRadixEt Rhizoma) 9 g, Kuan dong hua (FarfaraeFlos) 9 g, She gan (BelamcandaeRhizome) 9 g, Xi xin (AsariRadixEt Rhizoma) 6 g, Shan yao (RhizomaDioscoreae) 12 g, Zhi shi (AurantiiFructusImmaturus) 6 g, Chen pi (CitrusReticulata) 6 g, Huo xiang (PogostemonCablinBenth.) 9 g[8]. Raw herbs were boiled with water and made into a 400 mL decoction, which could be taken in 2 days with 100 mL b.i.d. for the entire course of treatment for 6 days. Studies have found over 210 possible targets of Qingfei Paidu Decoction and 50 common targets with COVID-19, which are associated with major immunological pathways including T cell, B cell, tumor necrosis factor (TNF), etc, by inhibiting the invasion and replication of virus directly[8-9].
Fuzhengyiqing Prescription include Ren shen (PanaxGinsengC. A. Mey.) 5g, Huang qi (HedysarumMultijugumMaxim.) 5 g, Shan yao (RhizomaDioscoreae) 10 g, Chen pi (CitrusReticulata) 5 g, Fu ling (PoriaCocosWolf.) 15 g, Jin yin hua (LoniceraeJaponicaeFlos) 5 g, Mint (MenthaeHerba) 3 g, Sang ye (MoriFollum) 5 g, Lu gen (PhragmitisRhizoma) 15 g, Huo xiang (PogostemonCablinBenth.) 5 g, Sheng gan cao (Licorice) 3 g, Lian zi xin (NelumbinisPlumula) 3 g. Raw herbs were processed into granules and taken with water b.i.d. for the entire course of treatment for 6 days.
(1) FZ/T 82006-2018比 FZ/T 73044-2012在外观质量方面多要求考核:针距密度、整烫、色差等。规格尺寸、外观疵点、附件、缝制等方面要求更加严格。
1.4 Covariable and outcome
Age, sex, underlying disease of close contacts,Nvalue andOvalue of cases which relate to those close contacts, were considered covariables. Age was categorized as dichotomous variable:<60 years old and ≥60 years old. Underlying diseases were categorized according to whether the close contacts had underlying diseases (i.e. hypertension, diabetes, chronic bronchitis). The primary outcome was the result (Positive and Negative) of Nucleic Acid Amplification Tests (NAATs), the positive rate of NAATs was reported. The secondary outcome was theNvalue andOvalue of close contacts who turn positive subsequently.
1.5 Statistical analysis
All data of study were analyzed statistically using R software including actual number of participants, expulsion and exclusion cases, demographic and other baseline characteristics, and efficacy.
Because three data sets form site Yangzhou, EDC system and CDC include different information, the three data sets were merged by ID number to get the final analysis data set before data analysis. The analysis data set included age, sex, underlying diseases,Nvalue,Ovalue, TCM use and the testing result of NAATs.
2 RESULTS
2.1 Statistical results after data handover
A total of 7 793 subjects were collected on site Yangzhou, of which 7 314 in TCM group and 479 in control group. A total of 8 440 subjects were collected using EDC system, of which 4 995(59.18%) in TCM group and 3 445 (40.82%) in control group.
After removing duplicate cases and non-close contacts by processing with tripartite matching and cleaning according to tripartite database (on site, EDC system and CDC), a total of 1 286 subjects were collected, of which 1 016 (79.00%) in TCM group and 270 (21.00%) in control group with 55 participants tested positive. A total of 54 cases missed age and 9 cases missed gender. The results of comparison of characteristics between TCM group and control group were listed in Table 1. The detail of underlying diseases of close contacts was shown as Table 2.
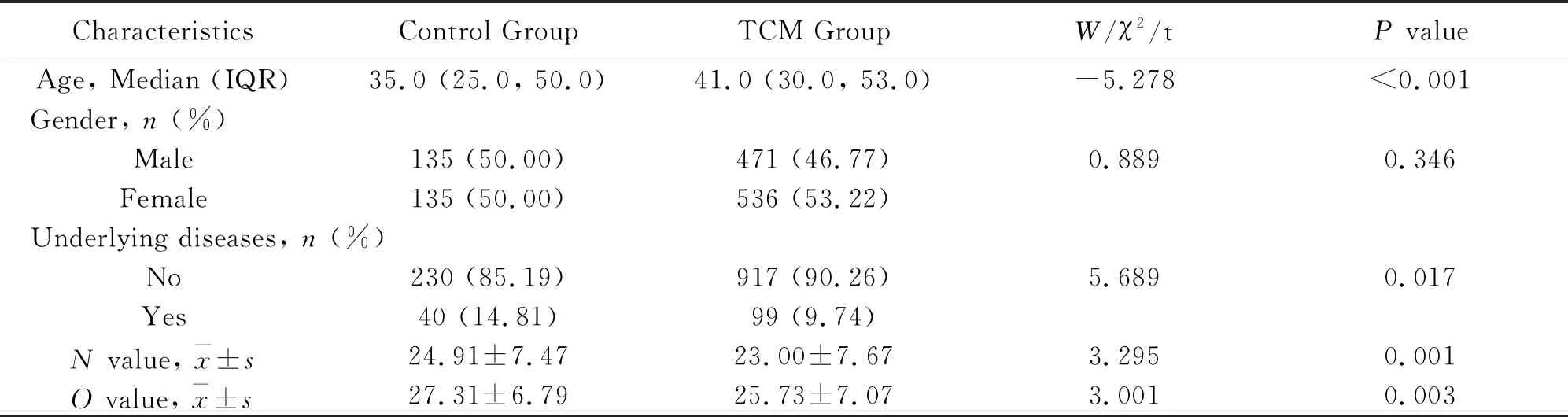
Table 1 Comparison of characteristics between TCM group and control group

Table 2 The detail of underlyingdiseases of close contacts
2.2 Inferential Statistical Results
Positive rate was analyzed between TCM and control groups in different subgroups based on gender and age (whether less than 60 years old), and the result was shown in Table 3. It was shown that the positive rate of TCM group was lower than that of control group for all subjects with statistically significant difference (P=0.019). Of male close contacts, the positive rate of TCM group was lower than that of control group with statistically significant difference (P=0.048). And of people ≥60 years old, the positive rate of TCM group was lower than that of control group with statistically significant difference (P<0.001).
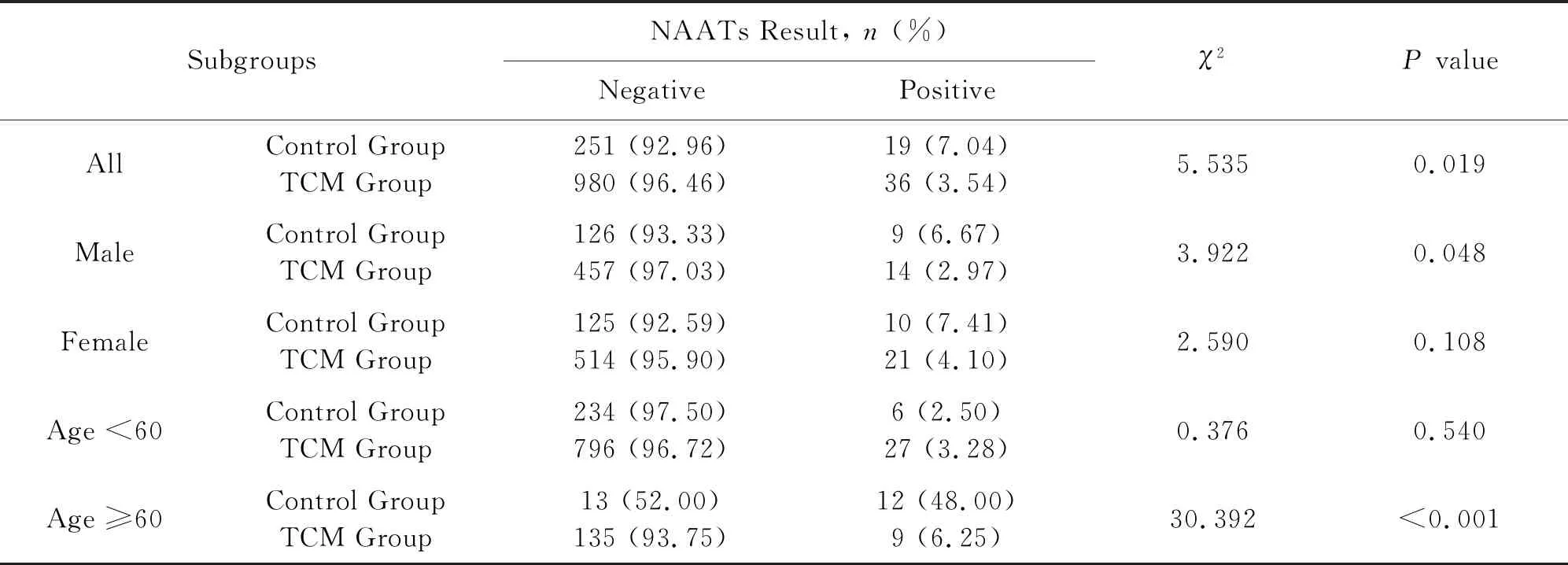
Table 3 Comparison of positive rate between TCM and control group before matching
Subjects with missing information need to be removed beforehand. The total number of subjects was 1 227 including 962 (78.40%) in TCM group and 265 (21.60%) in control group. Taking age and gender as matching variables and setting caliper value as 0.05, propensity score matching was conducted at a ratio of 1∶1 to match 259 participants in each group. There was no statistically significant difference in age (t=-0.402,P=0.688) and gender (χ2=0.378,P=0.538) between TCM and control groups after matching. The result pattern of propensity score matching was shown as Figure 1.
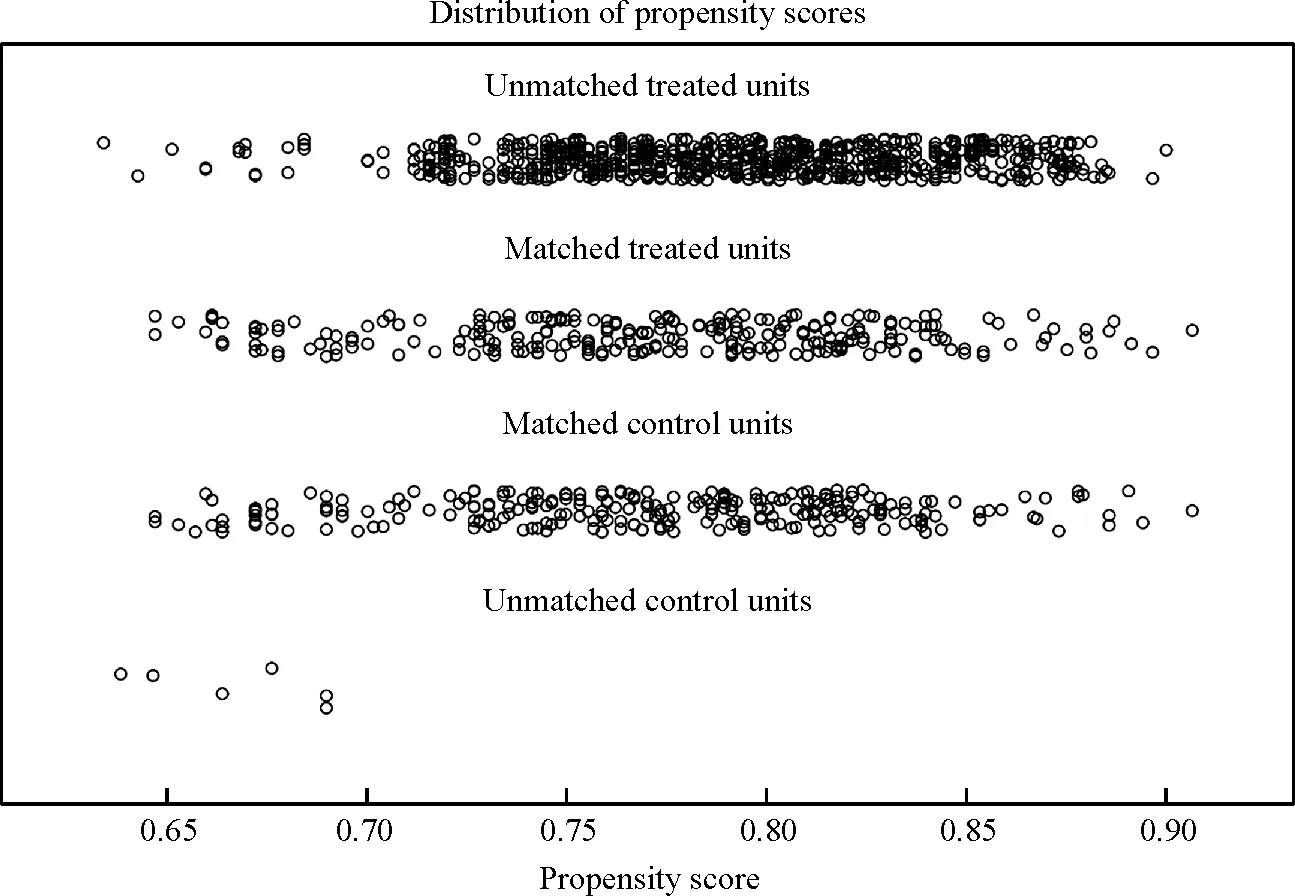
Fig. 1 Result pattern of propensity score matching
Dataaftermatchingwascomparedonpositiverateinallsubjectsanddifferentsubgroups.TheresultwasshowninTable4,whichindicatedthatthepositiverateofTCMgroupwaslowerthanthatofcontrolgroupforallsubjectswithstatisticallysignificantdifference(P=0.009).Ofmaleclosecontacts,thepositiverateofTCMgroupwaslowerthanthatofcontrolgroupwithstatisticallysignificantdifference(P=0.032).Andofpeople≥60yearsold,thepositiverateofTCMgroupwaslowerthanthatofcontrolgroupwithstatisticallysignificantdifference(P<0.001).
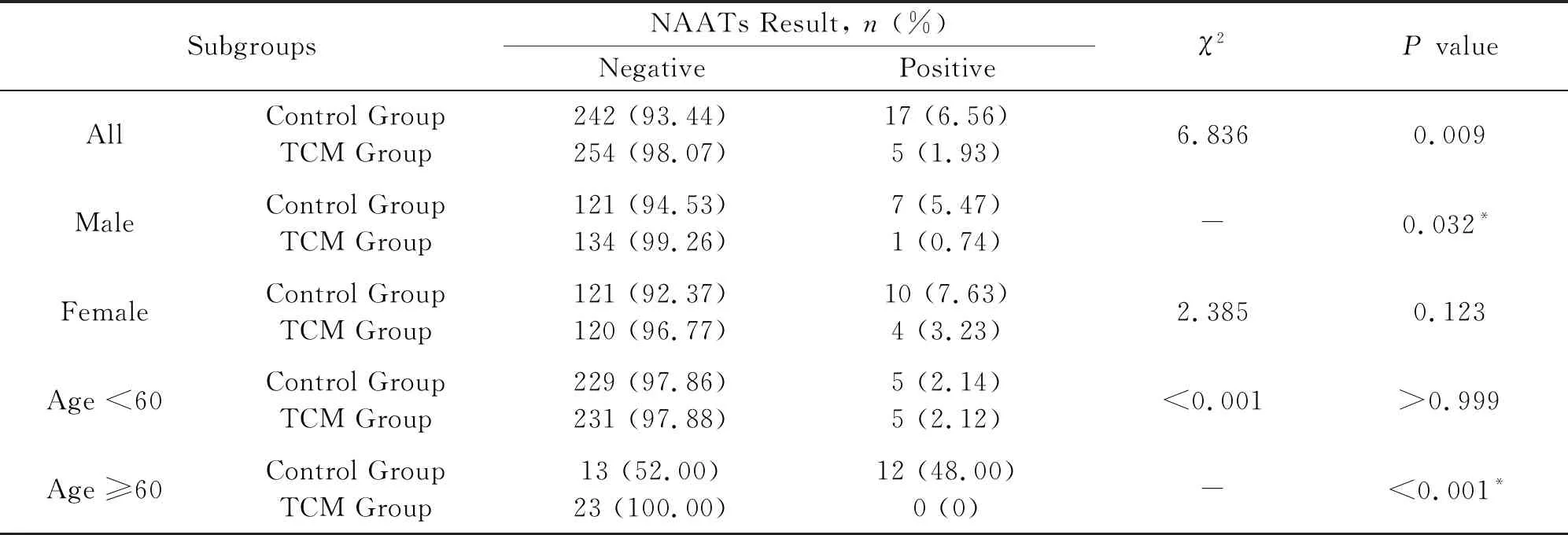
Table 4 Comparison of positive rate between TCM and control groups after matching
Multi-variable regression analysis was performed before matching data to examine the preventative effect of Chinese medicine on COVID-19 after adjusting gender and age. Compare to control group, the risk of testing positive was reduced by 0.547 times (OR=0.453, 95%CI: 0.251-0.842) in TCM group after adjusting age and gender, as shown in Table 5 and Figure 2. After further adjustingNvalue andOvalue, no statistically significant difference (OR=0.933,95%CI: 0.131-2.251,P=0.868) was observed between taking Chinese medicine and the risk of testing positive, as shown in Table 6.
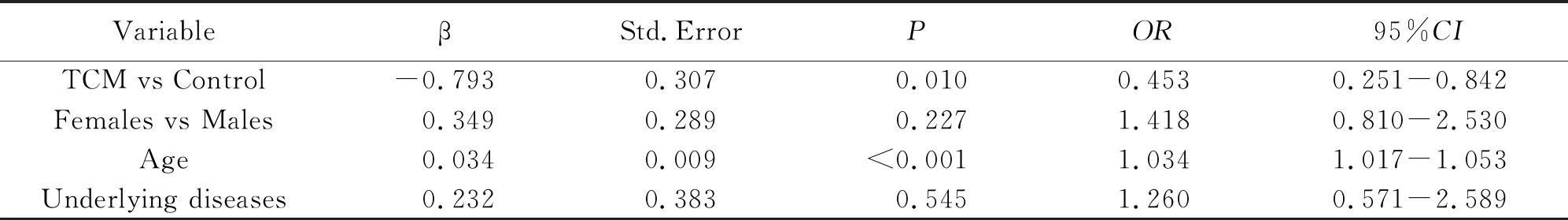
Table 5 Multivariable logistic regression of TCM reducing positive rate
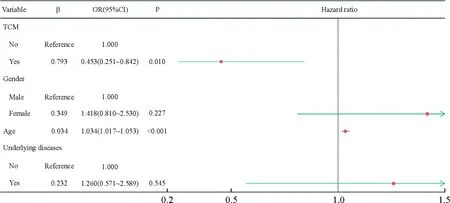
Fig. 2 Forest plot of multivariable logistic regression
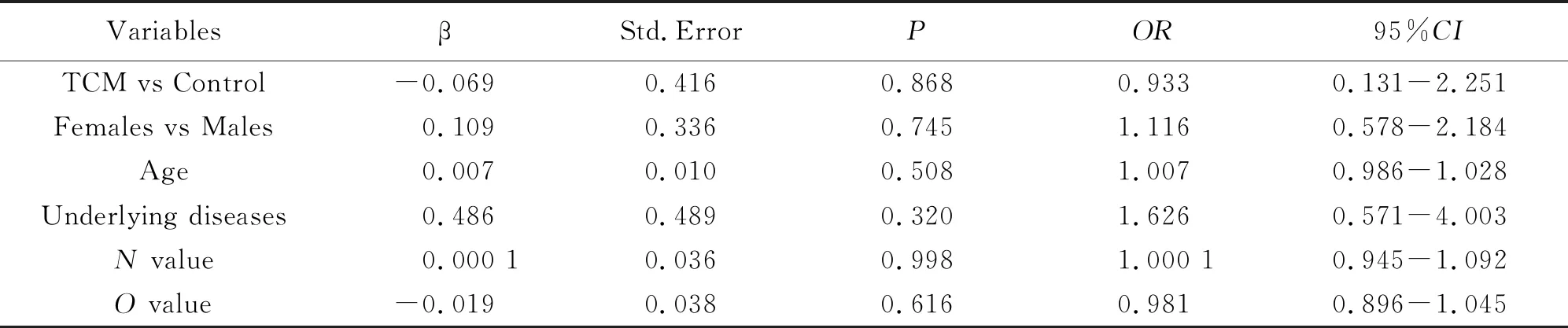
Table 6 Multi-variable logistic regression of TCM reducing positive rate after adjusting N and O value
For the analysis of viral load and classification in 55 close contacts who tested positive, the comparison result ofN/Ovalue of TCM and control groups showed that theNvalue of TCM group (27.00±6.05) was higher than that of control group (22.05±7.12), which indicated a statistically significant difference (P=0.017); and theOvalue of TCM group (28.42±6.01) was higher than that of control group (24.99±5.55), which indicated a statistically significant difference (P=0.045). Details were shown on Table 7 and Figure 3-4.
Among 55 close contacts who tested positive, 38 (69.09%) of them had moderate symptoms and 13 (23.64%) had mild symptoms (4 cases missing illness categories). There was no statistically significant difference (P=0.464) in composition ratio of categories between TCM and control groups, as shown in Table 8. Multi-variable regression analysis indicating the association between TCM use and illness categories was not significant (OR=1.761, 95%CI:0.357-8.696,P=0.487), as shown in Table 9.

Table 7 Comparison of N/O values between TCM and control groups
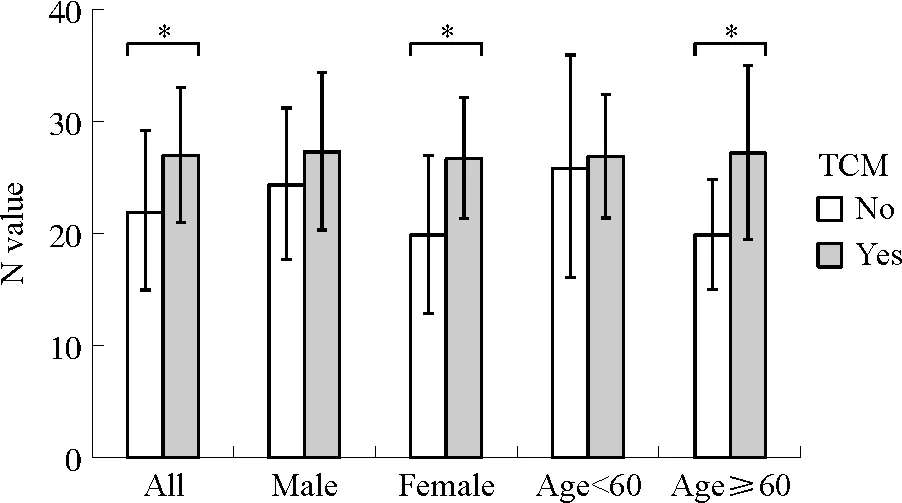
Note: *P<0.05.
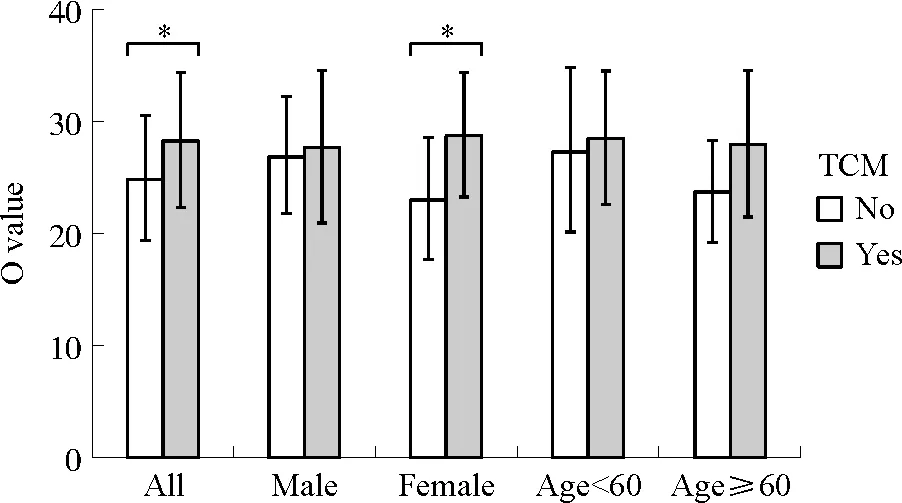
Note: *P<0.05.
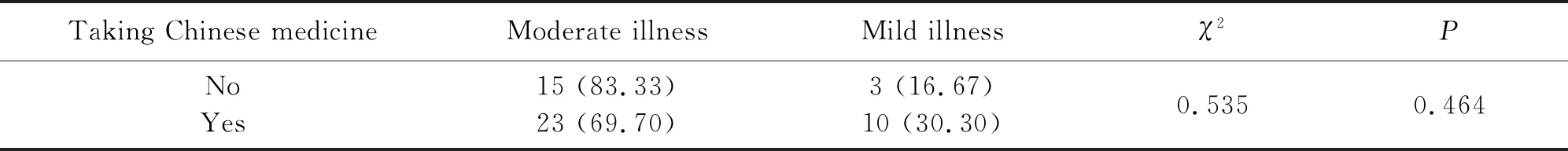
Table 8 Illness categories of positive cases between TCM and control groups
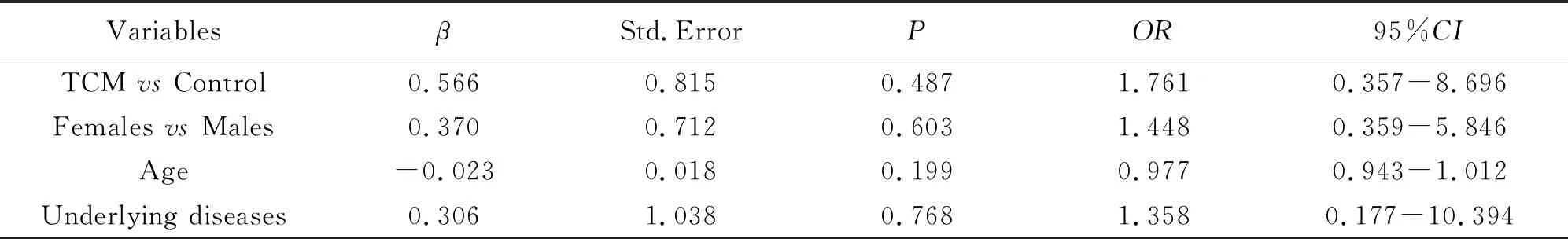
Table 9 Multi-variable logistic regression of the effect of TCM on illness severity
In conclusion, the data before and after matching revealed that the positive rate of TCM group was lower than that of control group in all subjects, male subjects, and subjects whose age is ≥60 in the analysis of positive rate between TCM and control groups, and the difference in composition ratio showed statistically difference. Multi-variable logistic regression (excluding NO viral load) indicated that the risk of testing positive was reduced by 0.547 times in TCM group compared to control group. Moreover, CT value of TCM group was higher than that of control group in all subjects and female subjects, and the result showed statistically significant difference.
3 DISCUSSIONS
The study used the data collected on site, by EDC system, and provincial CDC. Statistical subjects were filtered out after tripartite matching and cleaning, and a total number of 1 286 were collected as participants, of which 1 016 were in TCM group while 270 in control group. Taking age and gender as matching variables and setting caliper value as 0.05, propensity score matching was conducted at a ratio of 1∶1 to match 259 subjects in each group. The result showed that data before and after matching both indicated that the positive rate of TCM group was lower than that of control group in all subjects, male subjects, and subjects whose age is ≥60, which elucidated that the use of Chinese medicine in centralized quarantine sites was effective on preventing testing positive of close contacts to COVID-19 exposure, especially in specific population groups showing more remarkable preventative effect, such as males and people whose age is ≥60. This trial did not yet involve the pharmacological mechanism of Chinese medicine, which was believed to have the following effects: ①Most Chinese herbs used in these formulas had function of tonifying Qi, such as Huang qi, Bai zhu, and Shan yao, which could improve immunity of the body.[10-11]Therefore, it can be deduced that Chinese medicine may be effective by regulation the immune function of the close contacts, which is also consistent with the TCM theory of “healthy Qi is stored in the body and the pathogenic factors cannot be interfered”[12]. ②It was believed that bad emotion is a significant pathogenic factor in TCM. Chinese herbal ingredients have the effect of soothing the liver and relieving depression. Use of Chinese medicine could relieve panic and anxiety by reducing psychological stress, so as to improve the immune function of close contacts in centralized quarantine sites. ③The preventative effect of Chinese medicine is more noteworthy in close contacts whose age is ≥60 since elderly could have more underlying diseases. Chinese medicine may be effective by intervening on those basic problems and improve quality of life. In addition, COVID-19 vaccine rate may be lower in the elderly, which highlights the effect of Chinese medicine in unvaccinated population. ④The preventative effect is more remarkable in male close contacts in the analysis of subgroups, which may be contributed to the underlying diseases and higher smoking rates in males. Thus, male close contacts are more likely to get sick. More research is required for further illustration of gender specific effect of TCM.
The viral load of close contacts to COVID-19 exposure who tested positive were calculated, and the results showed that the CT value of the virus in TCM group was higher than that in control group for all subjects and females. Our results clarified that Chinese medicine could not only prevent testing positive in close contacts, but also reduce the viral load of confirmed cases, relieving symptoms and shortening infectious period. Based on the result of subgroup analysis, females may benefit more from the use of Chinese medicine, which may be contributed to their low body weight. As the same dosage can get the higher serum concentration, it indicates that taking weight as a reference on dosage may strengthen the effect of Chinese medicine.
The development of Chinese medicine prescriptions for specific diseases is recommended, as well as its preparation, quality control, and adverse reaction monitoring. During COVID-19 outbreak in Yangzhou, the early administrative involvement plays an indispensable role in the early intervention and high coverage rate of Chinese medicine use in centralized quarantine sites, which as well laid the foundation for the implementation of distributing Chinese medicine prescriptions. However, the lack of standard medication plan in the early stage and the use of local empirical prescriptions in different regions increased the difficulty for the preparation of Chinese medicine and pharmaceutical services in later stage. TCM treatment varies on individuals, places, and time, and focuses on the symptom-oriented adjustment and personalized diagnosis. It is considered that “one prescription to one person” is the inevitable result from TCM theory of syndrome differentiation. However, the statement ignores the ideology of TCM outlines and empirical effects of specific prescriptions and medications. Modern Chinese medicine should combine syndrome differentiation with disease differentiation especially when being involved in the public health emergencies. Not only should syndrome be targeted, but also the disease. Since the outbreak of COVID-19, the disease and the pathogenesis did not alter even though the place, timing, and strains varied over time. Therefore, the treatment experiences in Wuhan and Guangzhou in the early stage are advisable. Chinese medicine granules or oral liquids are required as their convenience and can be accurately used relying on body weight. Half dose of Qingfei Paidu Decoction is recommended to prevent from getting sick, which is proved to be effective in reducing positive rates in certain population. Ma huang, Ku xing ren, Sheng shi gao and Zhi gan cao has been used for the treatment of common cold, fever, and influenza virus infections, which means remove cold by dispersing Lung-Qi. She gan, Kuan dong hua and Xi xin are benefit to symptoms like cough, asthma, tonsillitis and sore throat. Bei chai Hu, Huang qin, Jiang ban xia, Ginger and Gui zhi have effect on exogenous febrile disorder containing cold and heat. Ze xie, Zhu ling, Fu ling, Bai zhu, Shan yao, Zhi shi and Chen pi can regulate Qi and eliminate turbidity, a prescription for nephritic syndrome, can improve kidney excretion function and inhibit inflammatory response.
Another proscription, Fuzhengyiqing is a Chinese medicine comprising 12 herbs.One the one hand, it is mainly administered in the treatment of “warm disease” characterized by clinical symptoms including cough, fever and headache. Jin yin hua, Lian qiao, Sang ye, Lu gen, Mint and Lian zi xin are good to clear heat and detoxigy. On the other hand, it is typically used strengthen the immune system, improve cells metabolism and promote blood circulation. Ren shen, Huang qi, Shan yao, Fu ling, Chen pi, Huo xiang and Sheng gan cao played significant roles in pathogenesis of multiple organ injury. All of them have been found to supporting health and suppling Qi.
In conclusion, widely use of Chinese medicine to prevent from COVID-19 in centralized quarantine sites is recommended, especially in population whose age is ≥60 to achieve higher benefits.
ACKNOWLEDGMENTS
We would like to express our appreciation and gratitude to Yangzhou Hospital of TCM for the data collection from isolation site and Jiangsu Provincial Center for Disease Control and Prevention for the data of close contacts providing.