Gastrointestinal histoplasmosis complicating pediatric Crohn disease:A case report and review of literature
2022-10-25QuinnMillerOmerSaeedKatrinaCollins
C Quinn Miller,Omer A M Saeed,Katrina Collins
C Quinn Miller,Omer A M Saeed,Katrina Collins,Department of Pathology,Indiana University School of Medicine,Indianapolis,IN 46202,United States
Abstract BACKGROUND Infection with Histoplasma capsulatum (H.capsulatum) can lead to disseminated disease involving the gastrointestinal tract presenting as diffuse abdominal pain and diarrhea which may mimic inflammatory bowel disease (IBD).CASE SUMMARY We report a case of 12-year-old boy with presumptive diagnosis of Crohn disease (CD) that presented with several months of abdominal pain,weight loss and bloody diarrhea.Colonoscopy showed patchy moderate inflammation characterized by erythema and numerous pseudopolyps involving the terminal ileum,cecum,and ascending colon.Histologic sections from the colon biopsy revealed diffuse cellular infiltrate within the lamina propria with scattered histiocytic aggregates,and occasional non-necrotizing granulomas.Grocott-Gomori’s Methenamine Silver staining confirmed the presence of numerous yeast forms suggestive of Histoplasma spp.,further confirmed with positive urine Histoplasma antigen (6.58 ng/mL,range 0.2-20 ng/mL) and serum immunoglobulin G antibodies to Histoplasma (35.9 EU,range 10.0-80.0 EU).Intravenous amphotericin was administered then transitioned to oral itraconazole.Follow-up computed tomography imaging showed a left lower lung nodule and mesenteric lymphadenopathy consistent with disseminated histoplasmosis infection.CONCLUSION Gastrointestinal involvement with H.capsulatum with no accompanying respiratory symptoms is exceedingly rare and recognition is often delayed due to the overlapping clinical manifestations of IBD.This case illustrates the importance of excluding infectious etiologies in patients with “biopsy-proven” CD prior to initiating immunosuppressive therapies.Communication between clinicians and pathologists is crucial as blood cultures and antigen testing are key studies that should be performed in all suspected cases of histoplasmosis to avoid misdiagnosis and inappropriate treatment.
Key Words: Crohn disease;Disseminated histoplasmosis;Endoscopy;Colon;Inflammatory bowel disease;Immunosuppression;Case report
lNTRODUCTlON
Histoplasmosis is an infection caused by inhalation of spores from the fungusHistoplasma capsulatum(H.capsulatum),found in soil enriched with bird and bat droppings and is endemic to the central and eastern states,prevalent in the Ohio and Mississippi River Valleys[1,2].Clinical manifestations are typically self-limiting in immunocompetent children,whereas immunocompromised children are likely to present with more severe or disseminated disease and may be indistinguishable from malignancy or tuberculosis[3,4].Single-organ histoplasmosis is rare,primarily affecting the lungs,occasionally lymph nodes,liver,bone marrow,skin and mucosal membranes[5-8].While the literature contains many reports of disseminated histoplasmosis reminiscent of Crohn disease (CD) radiographically and endoscopically in immunocompromised patients,there are relatively few reports of symptomatic gastrointestinal histoplasmosis occurring in immunocompetent patients.The most commonly involved sites are the terminal ileum and the colon[9].We report a case of an immunocompetent pediatric patient presenting with possible disseminated histoplasmosis after presumed initial diagnosis of CD.Early detection is critical to avoid treatment with immunosuppressive therapy and potential complications.
CASE PRESENTATlON
Chief complaints
History of present illness
The patient experienced abdominal pain,weight loss,and bloody diarrhea and was referred for upper and lower GI endoscopy with biopsy.
History of past illness
His medical history was remarkable for several mild and self-limiting respiratory illnesses with nonproductive cough.The most recent episode occurred fourteen months prior to his current presentation.
Personal and family history
No notable personal or family medical history.
Physical examination
Unremarkable physical examination.
Laboratory examinations
Esophagogastroduodenoscopy was performed and revealed focally ulcerated gastric mucosa and several inflammatory polyps arising within the second and third portions of the duodenum.Colonoscopy revealed patchy moderate inflammation characterized by erythema and numerous pseudopolyps involving the terminal ileum,cecum,and ascending colon (Figure 1).An erythematous region containing shallow ulcers was identified at the hepatic flexure.Multiple biopsies were taken from throughout the colon.A presumptive diagnosis of CD was made,methylprednisolone (40 mg/kg/d,IV) was administered and the patient was then discharged on oral prednisone (40 mg,QD) and oral mesalamine (1000 mg,TID).
Histologic examination of an H&E-stained colonic biopsy revealed a diffuse cellular infiltrate within the lamina propria with scattered histiocytic aggregates and occasional non-necrotizing granulomas (Figure 2A-C).Grocott-Gomori’s methenamine silver (GMS) and Periodic acid-Schiff stains confirmed the presence of numerous yeast forms morphologically suggestive ofH.capsulatum(Figure 2D and E),further confirmed with positive urineHistoplasmaantigen (6.58 ng/mL,positive range 0.2-20 ng/mL) and serum immunoglobulin G (IgG) antibodies toHistoplasma(35.9 EU,positive ≥ 10.0 EU).
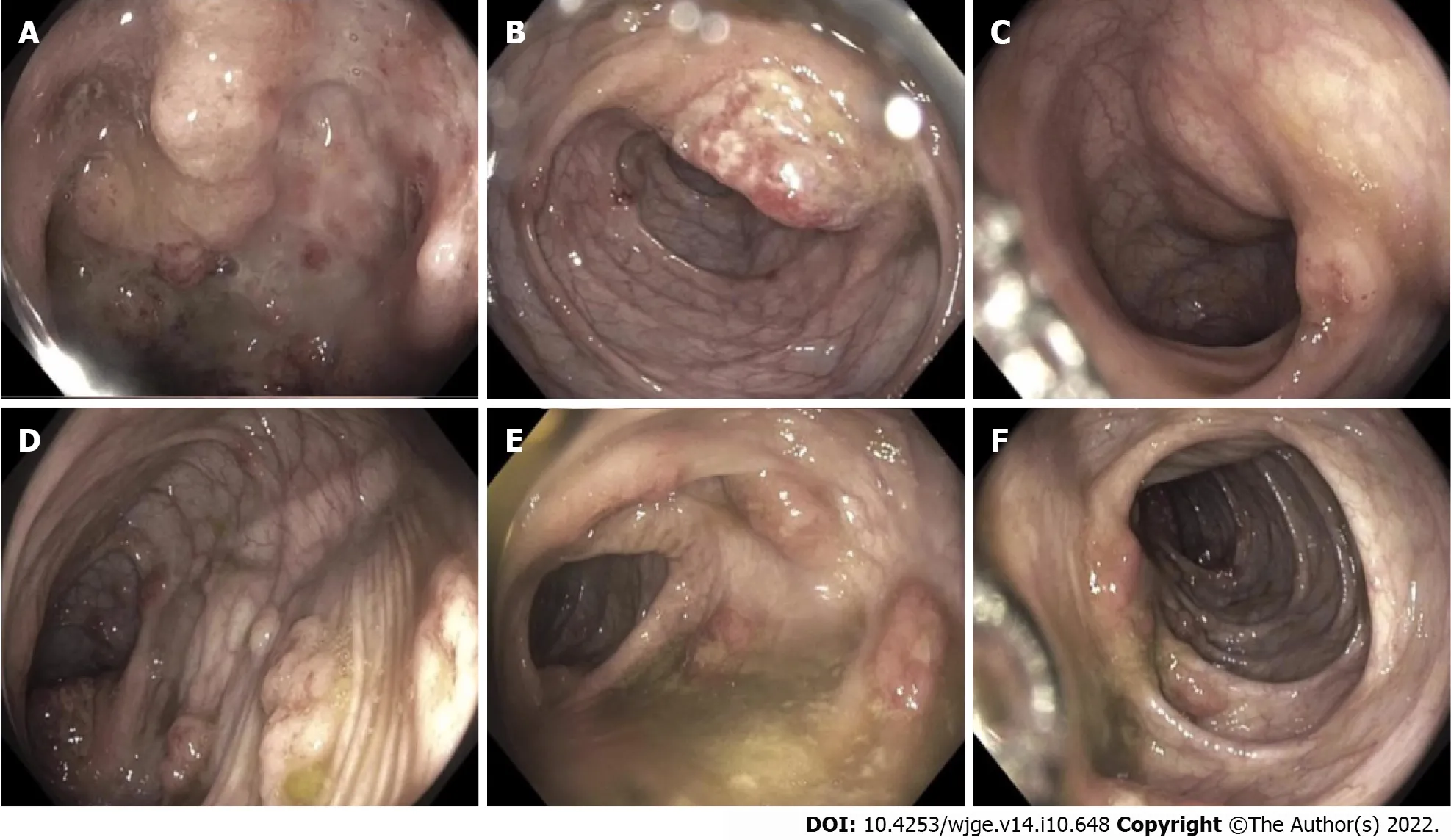
Figure 1 Colonoscopy findings.
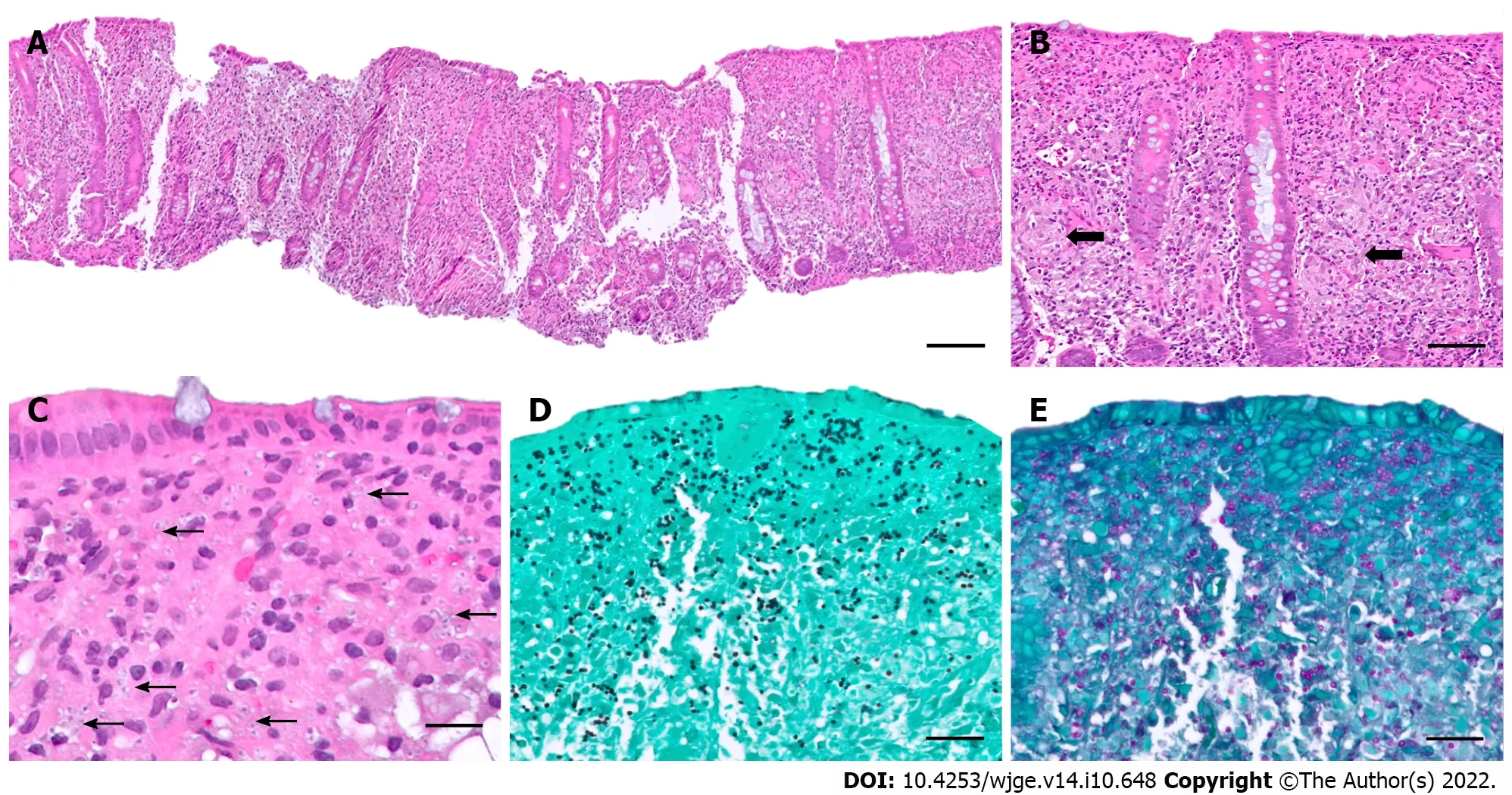
Figure 2 Histologic findings.
Given the unusual nature of the histoplasmosis infection,an immunological workup was initiated and revealed profound hypogammaglobulinemia: Serum IgG 94 mg/dL (range 638-1453),IgM 9 mg/dL (range 56-242),and IgA 40 mg/dL (range 45-285) as well as CD8 lymphopenia (253/mm3,range 331-1445).Genetic testing was ordered for inborn error of immunity using Invitae Primary Immunodeficiency Panel and one pathogenic variant was identified in CD40LG c.43del (pThr15Leufs*7),associated with X-linked hyper-IgM syndrome (XHIGM) and two likely pathogenic variants in TNFRSF13B c.310T>C (p.Cys104RG) (homozygous),associated with recessive common variable immunodeficiency (CVID).
Imaging examinations
Computed tomography (CT) of the chest,abdomen,and pelvis demonstrated a calcified left lower lobe lung nodule with associated hilar lymphadenopathy,diffuse colitis with wall thickening of the distal small bowel through the cecum,abdominal lymphadenopathy,and abnormal-appearing adrenal glands,likely related to disseminated histoplasmosis infection.
At daybreak,17 even before the sun was up, the woman came and woke the two children: Get up, you lie-abeds, we re all going to the forest to fetch wood
FlNAL DlAGNOSlS
Combined with the patient’s medical history,the final diagnosis was isolated gastrointestinal histoplasmosis complicating newly diagnosed,presumed CD.
TREATMENT
An induction regimen of liposomal amphotericin was administered (3 mg/kg/d,IV) followed by 1 year of oral itraconazole (200 mg,BID) and treatment with oral mesalamine (1000 mg,TID) to maintain endoscopic remission with plans for endoscopy and colonoscopy in the future after trailing off medication at 6 mo.
OUTCOME AND FOLLOW-UP
Ongoing follow-up is planned for diagnostic evaluation of CD and the treatment plan includes maintaining clinical improvement andHistoplasmaantigen clearance.Decisions on whether to initiate treatment for CD are pending as duration of antifungal therapy and safety of immunosuppressive therapy are to be determined.To date,our patient has completed 5 mo of a 12-mo course of antifungal therapy and is maintained on mesalamine until follow-up endoscopy and colonoscopy.The patient’s symptoms have largely resolved and remain stable after 5 mo of follow-up.
DlSCUSSlON
Gastrointestinal involvement commonly occurs as part of disseminated histoplasmosis;however isolated colonic involvement with lack of respiratory symptoms is rare[10].Histoplasmosis can occur at any age.Nonspecific clinical manifestations of gastrointestinal involvement such as abdominal pain,fever,weight loss,and diarrhea are variably present and may only be mild[6,10,11].Immunocompromised patients are at increased risk of developing disseminated disease and may experience complications such as bleeding or intestinal obstruction more readily than immunocompetent individuals.A high index of suspicion is required for diagnosing histoplasmosis and the gold standard for diagnosis includes isolation of the fungus in blood culture and antigen testing in suspected cases,as utilizing both serum and urine consistently provides the highest sensitivity for detection.Testing for anti-Histoplasmaantibodies further increases the sensitivity for diagnosis[12].
The terminal ileum is most commonly involved,presumably because of the lymphoid-rich tissue in this area,but can be found throughout the gastrointestinal tract[9].The pathologic findings of gastrointestinal histoplasmosis include mucosal ulceration,polypoid lesions,and obstructing masses[6,11,13].Histologically,tissue shows diffuse expansion of lamina propria and submucosa by macrophages containing intracellular yeast forms[6,10].As in our case,due to similarities in presentation,pattern of involvement and associated granulomatous inflammation,gastrointestinal histoplasmosis can mimic CD[6,14-17].
To our knowledge,only 7 cases of isolated gastrointestinal histoplasmosis occurring in the pediatric age group (younger than 18 years of age) have been previously reported,mostly from individual case reports (Table 1)[18-22] and one small case series[23].Ages ranged from 4 to 16 years with a median age of 13 years.Of the previously described cases,the male/female ratio was 5:2.Our patient presented at a slightly younger age than the median (12 yearsvs13 years).The most common presenting symptoms included abdominal pain and weight loss,with diarrhea,anorexia,and fever appearing occasionally.Pulmonary symptoms at presentation or during the disease course were not reported in any case.Five patients were presumed immunocompetent[20-22],while two patients were known to have immunocompromising conditions (hyper-IgE syndrome) prior to their presentation[18,19].One patient with hyper-IgE syndrome was effectively treated seven months prior for cough and fever of unknown origin[19].As in our case,five patients were given a presumptive diagnosis of CD based on clinical presentation and endoscopic findings[20-23].A broad range of diagnostic laboratory tests were performed including immunological tests for antigen and/or antibody detection.Microscopic examination revealed the presence of yeast forms (by routine hematoxylin and eosin staining and/or special staining methods) in all cases.
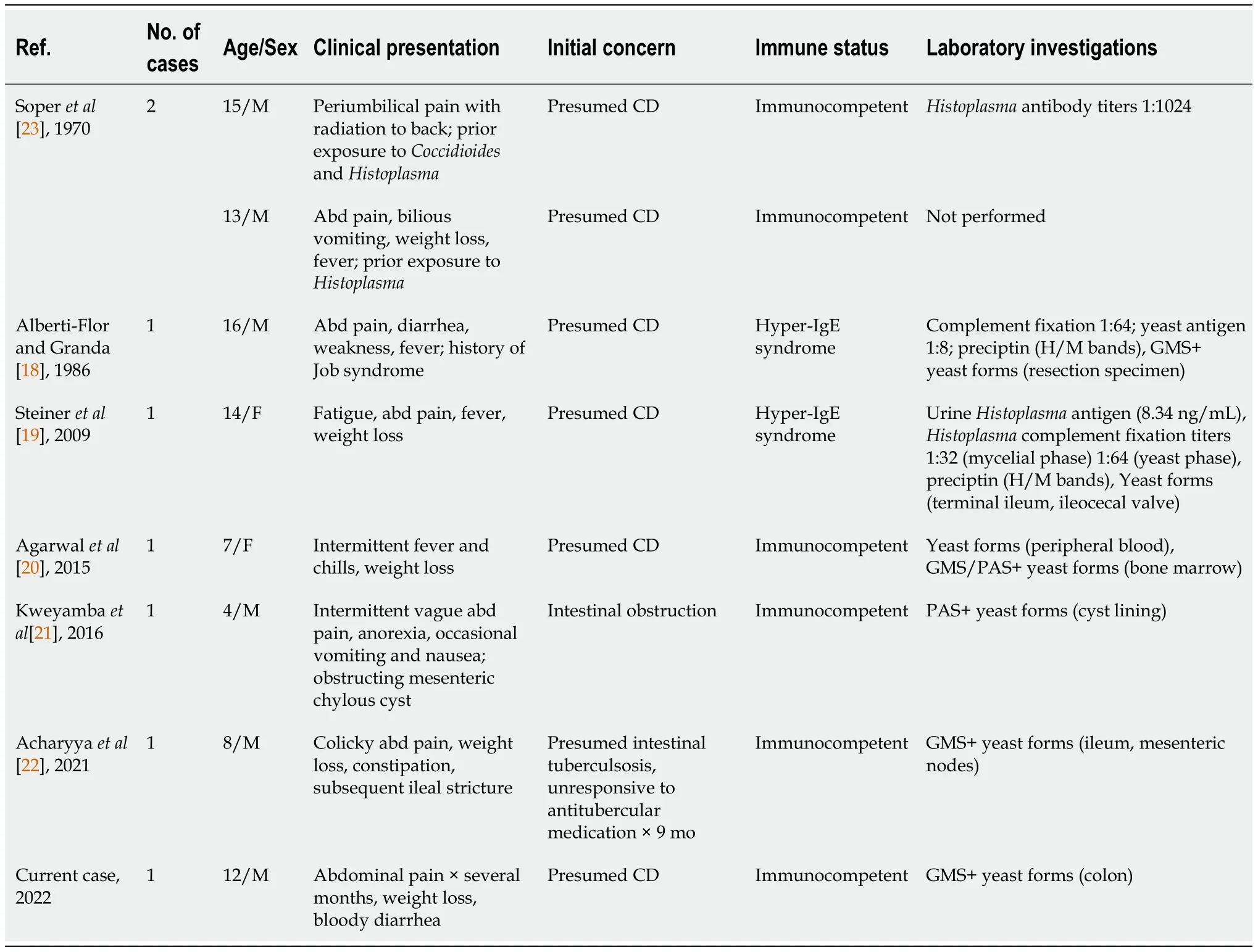
Table 1 Reports of histoplasmosis mimicking inflammatory bowel disease in pediatric immunocompetent patients: Cases published between 1970-present (including current case)
In our present case,the patient presented with gastrointestinal symptoms alone and endoscopic findings suggestive for CD and was started on corticosteroids and subsequently mesalamine.An interesting feature of our case is that while the gastrointestinal tract was the only site of symptomatic disease,it is unlikely to be the primary focus of infection.It is more likely that after inhalation of the fungus,dissemination by the bloodstream occurred before an immune response was mounted with some unidentifiable factor favoring persistence in the gastrointestinal tract exclusively.After additional workup,the patient was identified as more susceptible to histoplasmosis because of the dysregulation of cell-mediated immunity associated with his XHIGM and CVID,as suggested by his immunological testing results.Distinction of these entities is vital as the optimal treatment for one disease could lead to exacerbation of the other.A list of infectious diseases that should be excluded in patients diagnosed as inflammatory bowel disease (IBD) is provided in Table 2.
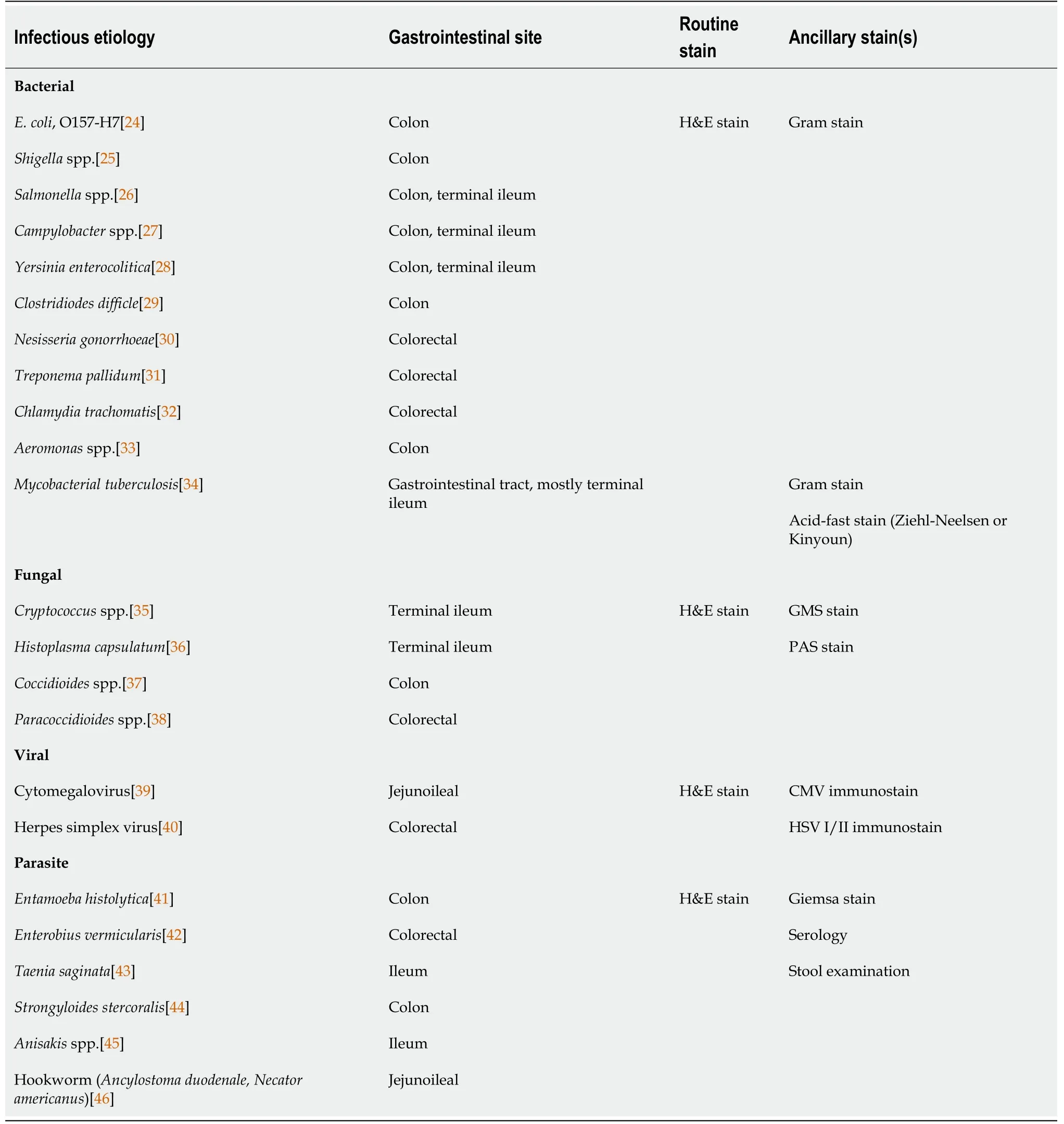
Table 2 lnfectious mimics of inflammatory bowel disease1
CONCLUSlON
Gastrointestinal involvement withH.capsulatumin the absence of pulmonary manifestations is exceedingly rare and may lead to delay in recognition due to overlapping symptoms with IBD.This case highlights the importance of excluding infectious etiologies in patients with “biopsy-proven” CD prior to initiating immunosuppressive therapies,especially in the setting of recent travel or exposure in an endemic area.Communication between clinicians and pathologists is crucial as tests forHistoplasmaantigen in urine or serum should be performed once histoplasmosis is suspected.
FOOTNOTES
Author contributions:Miller CQ served as the primary author;Miller CQ and Collins K are responsible for this literature review;Miller CQ,Saeed OAM,and Collins K were responsible in the construction of the manuscript;Collins K served as the senior author,provided invaluable educational input and managed the edits of the manuscript,and guided the primary author through the submission process;All authors read,revised,and gave approval of the manuscript.
lnformed consent statement:All study participants or their legal guardian provided informed written consent about personal and medical data collection prior to study enrollment.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016),and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United States
ORClD number:C Quinn Miller 0000-0002-1362-7828;Omer A M Saeed 0000-0002-4584-9222;Katrina Collins 0000-0002-9603-6731.
S-Editor:Fan JR
L-Editor:A
P-Editor:Fan JR
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Endoscopic palliation of malignant biliary obstruction
- Gastric intestinal metaplasia development in African American predominant United States population
- Water-jet vs traditional triangular tip knife in peroral endoscopic myotomy for esophageal dysmotility:A systemic review and metaanalysis
- Laparoscopic Janeway gastrostomy as preferred enteral access in specific patient populations:A systematic review and case series
- Tracheoesophageal fistulas in coronavirus disease 2019 pandemic:A case report
- Hemostasis of massive bleeding from esophageal tumor:A case report
