Hemostasis of massive bleeding from esophageal tumor:A case report
2022-10-25AlekseiKashintsevDmitriyRusanovMariyaAntipovaSergeyAnisimovOlegGranstremNikolaiYuKokhanenkoKonstantinMedvedevEldarKutumovAnastasyaNadeevaVitaliProutski
Aleksei A Kashintsev,Dmitriy S Rusanov,Mariya V Antipova,Sergey V Anisimov,Oleg K Granstrem,Nikolai Yu Kokhanenko,Konstantin V Medvedev,Eldar B Kutumov,Anastasya A Nadeeva,Vitali Proutski
Aleksei A Kashintsev,Sergey V Anisimov,Oleg K Granstrem,Vitali Proutski,Pandx Ltd.,Whittlesford,Cambridge,CB22 4NW,United Kingdom
Dmitriy S Rusanov,Mariya V Antipova,Nikolai Yu Kokhanenko,Konstantin V Medvedev,Eldar B Kutumov,Anastasya A Nadeeva,Pandx LLC.,Saint-Petersburg 194100,Russia
Abstract BACKGROUND Esophageal cancer is a common type of cancer and serious bleeding from esophageal tumors can occur in routine clinical practice.The arrest of bleeding from esophageal tumor is not a trivial task,which can sometimes require non-standard solutions.We report a case of successful hemostasis of massive bleeding from esophageal tumor performed by a novel two-balloon catheter inserted endoscopically,with a local hemostatic treatment applied.CASE SUMMARY A 36-years old male patient with advanced esophageal cancer developed bleeding from the tumor following endoscopic stenting with a self-expanding metal stent.Due to the ineffectiveness of standard approaches,after a medical conference,the patient was treated with a novel method based on the use of a two-balloon catheter creating an isolated area in esophagus and locally dispersing hemostatic polysaccharide powder inside the isolated interior.Hemostasis was successful and subsequent endoscopic examination revealed the presence of organized clot and localized defect,which was coagulated in a planned manner.CONCLUSION The authors present a new catheter-based method of hemostasis of esophageal tumor bleeding.
Key Words: Esophageal cancer;Esophageal bleeding;Two-balloon catheter;Endoscopic hemostasis;Hemostatic polysaccharide powder;Case report
lNTRODUCTlON
Various stages of dysphagia are common complications of esophageal cancer.Stenting of esophageal tumors is a standard method of treatment and palliative care.Placement of a self-expandable metal stent is required,on the one hand to facilitate oral nutrition and on the other hand as the first standard step of treatment pre-empting neoadjuvant chemotherapy with brachytherapy[1,2].At the same time,placement of a stent can lead to the development of various complications,the frequency of which can reach up to 50%[3].The most common are esophageal perforation,fistula,stent migration,and bleeding[4,5].The incidence of bleeding after stenting is not high and varies from 1% to 12%[6,7].However,the volume of bleeding if it occurs is often massive and is associated with high mortality[6,7].Due to the fact that this complication is rare,and its course is extremely aggressive,the experience of managing this group of patients is limited.The recommendations are nonsystematic in nature and one should be prepared for various scenarios,from the application of various hemostatic remedies and transfusion of blood components to angiographic methods to stop the bleeding.The unfavorable outcome of this complication can be caused by a stent itself that interferes with verification of the source of bleeding,by pathological hypervascularization of a tumor,rich blood supply of the esophagus,including from esophageal arteries stemming from the descending aorta,and by a limited amount of time available to help a patient[6-9].
Analysis of the literature suggests that time is the main factor in the unsatisfactory result of trying to achieve hemostasis during the first wave of bleeding.The time spent on patient admission and delays in identifying the source of bleeding,trying various options of endoscopic hemostasis,switching to endovascular methods,all negatively affect the outcome of treatment.To counter this,a method has been developed that consists of isolating the source of bleeding,in this case the part of the esophagus with a tumor,from other parts of the gastrointestinal tract,with the possibility of delivering hemostatic agents into it while maintaining the connectivity between the parts of esophagus proximal and distal to the isolated region.The latter feature enables concurrent and continuous drainage of the proximal part and administration of solutions and enteral nutrition.This approach achieves several important effects.First,it allows one to mechanically create an isolated area with high pressure in which blood,clots,and coagulation factors facilitate hemostasis.Second,it enables localized delivery of hemostatic agents such as polysaccharide hemostatic powders.Third,by maintaining functional connectivity of the gastrointestinal tract,the method allows both for essential nutritional support and provision of fluids,and for sufficient exposure time to achieve hemostasis.
CASE PRESENTATlON
Chief complaints
Vomiting with blood,melena,weakness,an episode of loss of consciousness.
History of present illness
A 36-year-old male patient was admitted on an emergency basis on November 14,2021,with manifestation of gastrointestinal bleeding.At the time of admission,the degree of blood loss,according to the changes in the level of hemoglobin,erythrocytes and hematocrit,was assessed as moderate.
History of past illness
When collecting an anamnesis,it was established that for the first time the dysphagia was observed in September 2021.An X-ray investigation performed at the time revealed changes characteristic of a tumor of the gastroesophageal junction (Figure 1).The patient categorically refused further examination and treatment and was discharged.Later he was followed up at the oncology clinic,and on October 29 diagnosed with cancer of gastroesophageal junction,type II according to Siewert classification,stage IVB,Grade 2,dMMR/MSI-h-negative,HER2-negative adenocarcinoma.Concomitant diseases: obesity class III,essential hypertension.On November 10,endoscopic stenting of esophagus was performed to resolve dysphagia.The patient was discharged on November 13,2021.

Figure 1 X-ray of esophagus revealing a filling defect.
Personal and family history
There was no personal and family history of cancer.
Physical examination
At the time of admission,blood pressure was 80/40 mmHg and heart rate was 114 beats/min.
Laboratory examinations
Blood analysis demonstrated high volume of loss,with erythrocyte count 2.1 mln cells/uL,hemoglobin 79 g/L,and hematocrit 31.0%.
Imaging examinations
Endoscopic examination revealed that there was ongoing bleeding from under the partially covered esophageal stent (Figure 2).It was however not possible to clearly establish the localization of the source of bleeding.
MULTlDlSClPLlNARY EXPERT CONSULTATlON
Given the severity and urgency of situation,a multidisciplinary meeting was held,which included surgeons,endoscopists and anesthesiologists.
FlNAL DlAGNOSlS
Cancer of the gastroesophageal junction,type II according to Siewert classification,stage IVB,Grade 2,dMMR/MSI-h-negative,HER2-negative adenocarcinoma.Complications: severe esophageal bleeding.Concomitant diseases: obesity class III and essential hypertension.
TREATMENT
Both standard intravenous hemostatic therapy and blood component transfusion were administered.An attempt to perform endoscopic hemostasis by electrocoagulation of the tumor failed to achieve positive results.It was decided that due to the impossibility of achieving hemostasis using standard methods and further deteriorating condition of the patient,it was advisable,according to vital indications,to use the isolation method and locally introduce a polysaccharide powdered hemostatic agent.The two-balloon catheter was inserted endoscopically into the stomach past the stent,so that the tumor site with the source of bleeding were located between the balloons.Balloons were inflated isolating the area of bleeding,and hemostatic powder was injected though the catheter opening located between the balloons and dispersed inside the isolated interior.The procedure stopped the bleeding,as demonstrated by normalization of hemodynamic parameters and absence of retrograde flow of blood through the main channel of the catheter.Over the next day,there was no sign of bleeding recurrence,which was supported by stable levels of hemoglobin and erythrocyte count.On November 15,the day after hemostasis,the catheter was removed,and repeated endoscopic procedure was performed in order to identify the source of bleeding and to reposition the esophageal stent.A 1.5-cm long defect with an organized clot was detected in the gastroesophageal junction (Figure 3).Argon plasma coagulation was performed after which the same stent was repositioned and fixed.Fluoroscopy performed on November 18 showed that stent’s position was adequate,the contrast medium freely entered the stomach,and there were no streaks or signs of stent migration (Figure 4).No recurrence of bleeding was observed,and the patient was discharged on November 18 in adequate condition to continue treatment at the oncology clinic.
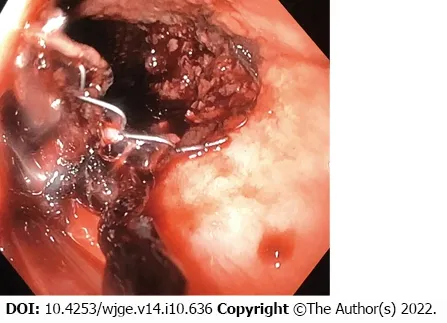
Figure 2 Endoscopic view of bleeding with visualization of uncovered part of the stent.There were visible signs of tumor growth.

Figure 3 View of a clot in the gastroesophageal junction after stent removal.
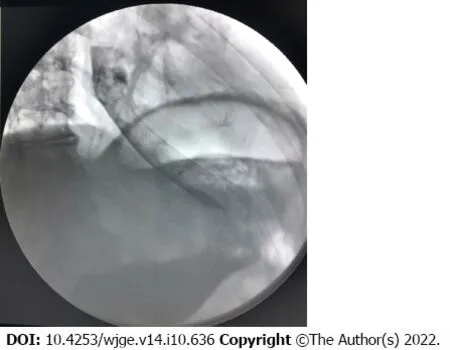
Figure 4 X-ray of esophagus.
OUTCOME AND FOLLOW-UP
After 4 mo of follow-up on March 9,2022,patient was hospitalized with recurrent dysphagia.Endoscopy of the upper part of the stent revealed tumor overgrowth and infiltration with stenosis of the esophagus.Endoscopic ablation with tumor coagulation and recanalization of the esophagus was performed successfully.Two days after the procedure,clinical signs of dysphagia disappeared,as confirmed by controlled esophageal fluoroscopy,and the patient was discharged.
DlSCUSSlON
Bleeding after stenting of esophageal cancer is a severe complication with a high rate of mortality.Most often it develops in the first 2 wk after manipulation[8,9].The main reasons include mucosal trauma caused by the free uncovered part of the stent during active esophageal peristalsis and increased pressure on the wall of the organ at the time of its expansion by the stent,leading to necrotic changes[10].Since the esophagus is well supplied with blood,the bleeding is often massive.The presence of a stent hampers identification of the source of bleeding,and prevents application of argon plasma coagulation,injection of adrenaline or clipping.Large number of collateral blood vessels and segmental type of blood supply of the esophagus are the reason why many authors recommend supplementing endoscopic approaches with endovascular methods of hemostasis,which nevertheless often fail to achieve the desired effect[8-10].It is important to have a wide range of methods available for both identification and tackling of the source of bleeding.In clinical practice however,resources are often limited and implementation of extensive care is associated with loss of time,which in this case is critical.Presence of disseminated tumor and poor somatic status of a patient can also play an important role,limiting the surgeon’s options.
The method of hemostatic treatment described here allows for localization of the source of bleeding by isolating it from other parts of the gastrointestinal tract.At the same time,it does not require identification of precise location of the site of bleeding.The method implements four hemostatic approaches: (1) Applying pressure on the submucosal vessels by the inflated balloons;(2) tamponade of the source of bleeding by blood clots;(3) targeted delivery of hemostatic agents to the bleeding site;and (4) prevention of migration of hemostatic agents and blood clots to other parts of the gastrointestinal tract due to peristalsis.The latter prolongs exposure to hemostatic agents,which is enhanced by the ability of the two-balloon catheter used in the procedure to preserve connectivity of the gastrointestinal tract and to remain in place long enough to achieve the desired hemostatic effect.
CONCLUSlON
Availability of a fast and simple method for stopping bleeding from a tumor in the esophageal lumen,which does not require a high level of specialist training,is easy to perform and that provides long-term hemostasis and ability to administer enteral nutrition and drain the upper part of the esophagus,will help save time and improve the quality of care for this group of patients.While the present case is focused on esophageal bleeding,the method proposed could be applied to treating bleeding in other parts of the gastrointestinal tract.
FOOTNOTES
Author contributions:Kashintsev AA,Anisimov SV,Granstrem OK,Kutumov EB,Nadeeva AA and Proutski V designed the study;Kashintsev AA,Rusanov DS,Antipova MV,Kokhanenko NY and Medvedev KV performed the study;Kashintsev AA,Anisimov SV,Granstrem OK,and Proutski V analyzed the results and wrote the manuscript;all authors have read and approve the final manuscript.
lnformed consent statement:All study participants,or their legal guardian,provided informed written consent prior to study enrollment.
Conflict-of-interest statement:All authors report no relevant conflict of interest for this article.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016),and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United Kingdom
ORClD number:Aleksei A Kashintsev 0000-0002-3708-1129;Sergey V Anisimov 0000-0003-1976-9912;Vitali Yu Proutski 0000-0002-2432-8698.
Corresponding Author's Membership in Professional Societies:American Association for cancer research,No.461256.
S-Editor:Wu YXJ
L-Editor:Kerr C
P-Editor:Wu YXJ
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Endoscopic palliation of malignant biliary obstruction
- Gastric intestinal metaplasia development in African American predominant United States population
- Water-jet vs traditional triangular tip knife in peroral endoscopic myotomy for esophageal dysmotility:A systemic review and metaanalysis
- Laparoscopic Janeway gastrostomy as preferred enteral access in specific patient populations:A systematic review and case series
- Tracheoesophageal fistulas in coronavirus disease 2019 pandemic:A case report
- Cronkhite-Canada syndrome:First case report from Egypt and North Africa
