Tracheoesophageal fistulas in coronavirus disease 2019 pandemic:A case report
2022-10-25MartinAlonsoGomezZuletaDanielMauricioGallegoOspinaOscarFernandoRuiz
Martin Alonso Gomez Zuleta,Daniel Mauricio Gallego Ospina,Oscar Fernando Ruiz
Martin Alonso Gomez Zuleta,Daniel Mauricio Gallego Ospina,Oscar Fernando Ruiz,Department of Internal Medicine,Gastroenterology unit,Universidad Nacional de Colombia,Bogota 11321,Colombia
Abstract BACKGROUND Tracheoesophageal fistulas (TEFs) can be described as a pathological communication between the trachea and the esophagus.According to their origin,they may be classified as benign or malignant.Benign TEFs occur mostly as a consequence of prolonged mechanical ventilation,particularly among patients exposed to endotracheal cuff overinflation.During the severe acute respiratory syndrome coronavirus 2 virus pandemic,the amount of patients requiring prolonged ventilation rose,which in turn increased the incidence of TEFs.CASE SUMMARY We report the cases of 14 patients with different comorbidities such as being overweight,or having been diagnosed with diabetes mellitus or systemic hypertension.The most common symptoms on arrival were dyspnea and cough.In all cases,the diagnosis of TEFs was made through upper endoscopy.Depending on the location and size of each fistula,either endoscopic or surgical treatment was provided.Eight patients were treated endoscopically.Successful closure of the defect was achieved through over the scope clips in two patients,while three of them required endoscopic metal stenting.A hemoclip was used to successfully treat one patient,and it was used temporarily for another patient pended surgery.Surgical treatment was performed in patients with failed endoscopic management,leading to successful defect correction.Two patients died before receiving corrective treatment and four died later on in their clinical course due to infectious complications.CONCLUSION The incidence of TEFs increased during the coronavirus disease 2019 pandemic (from 0.5% to 1.5%).We believe that endoscopic treatment should be considered as an option for this group of patients,since evidence reported in the literature is still a growing area.Therefore,we propose an algorithm to lead intervention in patients presenting with TEFs due to prolonged intubation.
Key Words: Tracheoesophageal fistula;COVID-19;Endoscopy therapy;Gastroenterology therapy;Case report
lNTRODUCTlON
Tracheoesophageal fistulas (TEFs) are defined as abnormal communications between the esophagus and the trachea or bronchi,leading to the passage of oral and gastric secretions into the respiratory tract[1].TEFs can be classified into two main categories: Congenital or acquired.The congenital form is frequently associated with type C esophageal atresia (85%),presenting in an isolated manner in 4% of cases.Characteristically,clinical manifestations of this condition develop early in life[2-4].On the other hand,acquired TEFs mainly affect adults and are most frequently found in the cervicothoracic junction.TEFs can be malignant or benign.Each type constitutes approximately half of the acquired cases[4].
Malignant TEFs are a catastrophic complication of invasive neoplasms of the esophagus (squamous cell carcinoma),trachea,lung,or mediastinum[4-6].On the other hand,benign fistulas mainly develop due to prolonged mechanical ventilation (through an endotracheal tube or tracheostomy);blunt trauma to the neck and chest;traumatic or surgical injury of the esophagus;granulomatous mediastinal infections;previous esophageal stents,or ingestion of foreign bodies/corrosives[5].In patients undergoing invasive mechanical ventilation,some of the risk factors for TEFs include prolonged intubation,endotracheal cuff overinflation,excessive movement of the endotracheal tube (prone positioning),hypotension,diabetes mellitus,previous respiratory tract infections,use of steroids,and requiring nasogastric tube feeding,among others[7,8].
The most common clinical presentation of TEFs includes respiratory distress,dysphagia,cough after swallowing (ONO sign),malnutrition,and recurrent pulmonary infections.The severity of symptoms largely depends on their size and location[8,9].A diagnosis should be made by combining characteristic findings on thoracic imaging (esophagogram and chest tomography with 3D reconstruction) and those on endoscopic studies such as bronchoscopy and upper endoscopy.These studies are also essential when planning the best treatment option for each patient[1,8,10,11].
The mean survival reported for patients with TEFs is less than 3 mo from the time of diagnosis.As such,adequate treatment should include an immediate multidisciplinary approach,including specialists in critical care,interventional pulmonology,gastroenterology,and thoracic surgery.Currently,there are few case reports regarding TEFs due to prolonged intubation in patients with coronavirus disease 2019 (COVID-19)[12-16].We herein present a case series on patients with COVID-19 who develop TEFs and discuss diagnostic and therapeutic approaches.
CASE PRESENTATlON
Chief complaints
Before creating this case series,we obtained informed consent from each patient or their legal guardians.We included patients who were admitted to a university hospital in the city of Bogotá,Colombia in the period between November 2020 and December 2021.We identified 14 adult patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia who developed TEFs as a complication of prolonged mechanical ventilation.
We present the sociodemographic variables of the patients and relevant information on their past medical histories in Table 1.The average age was 53.5 years (range 38-72 years).Half of the sample was composed by men.Comorbidities were found in 85.7% of the patients,with the most frequent being obesity/overweight,diabetes mellitus,and systemic hypertension.
History of present illness
The clinical characteristics of the patients are shown in Table 2.The most common symptoms,which lead all patients to attend the emergency room,were cough and dyspnea.All of the subjects were diagnosed with severe pneumonia due to COVID-19.At least 64.2% presented with septic shock,requiring vasoactive support.All patients required invasive mechanical ventilation for more than 14 d.Acute respiratory distress syndrome (ARDS) was documented in 13 patients,and this variable was no available for assessment in one patient.All patients were treated with a steroid (dexamethasone: 6 mg s.c.,q.d.for 10 d),and the steroid was prematurely stopped in one patient due to diabetic ketoacidosis during treatment.All patients received enteral nutrition through nasoenteral tubes.
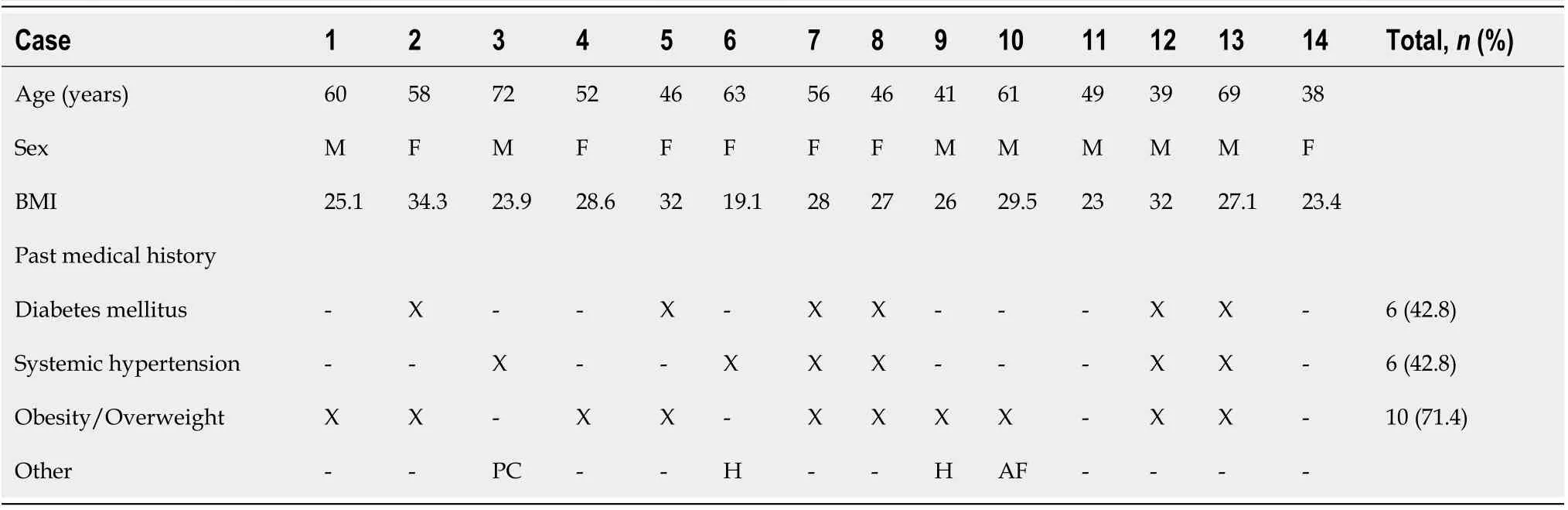
Table 1 Characteristics of patients with tracheoesofageal fistulas in 2020-2021
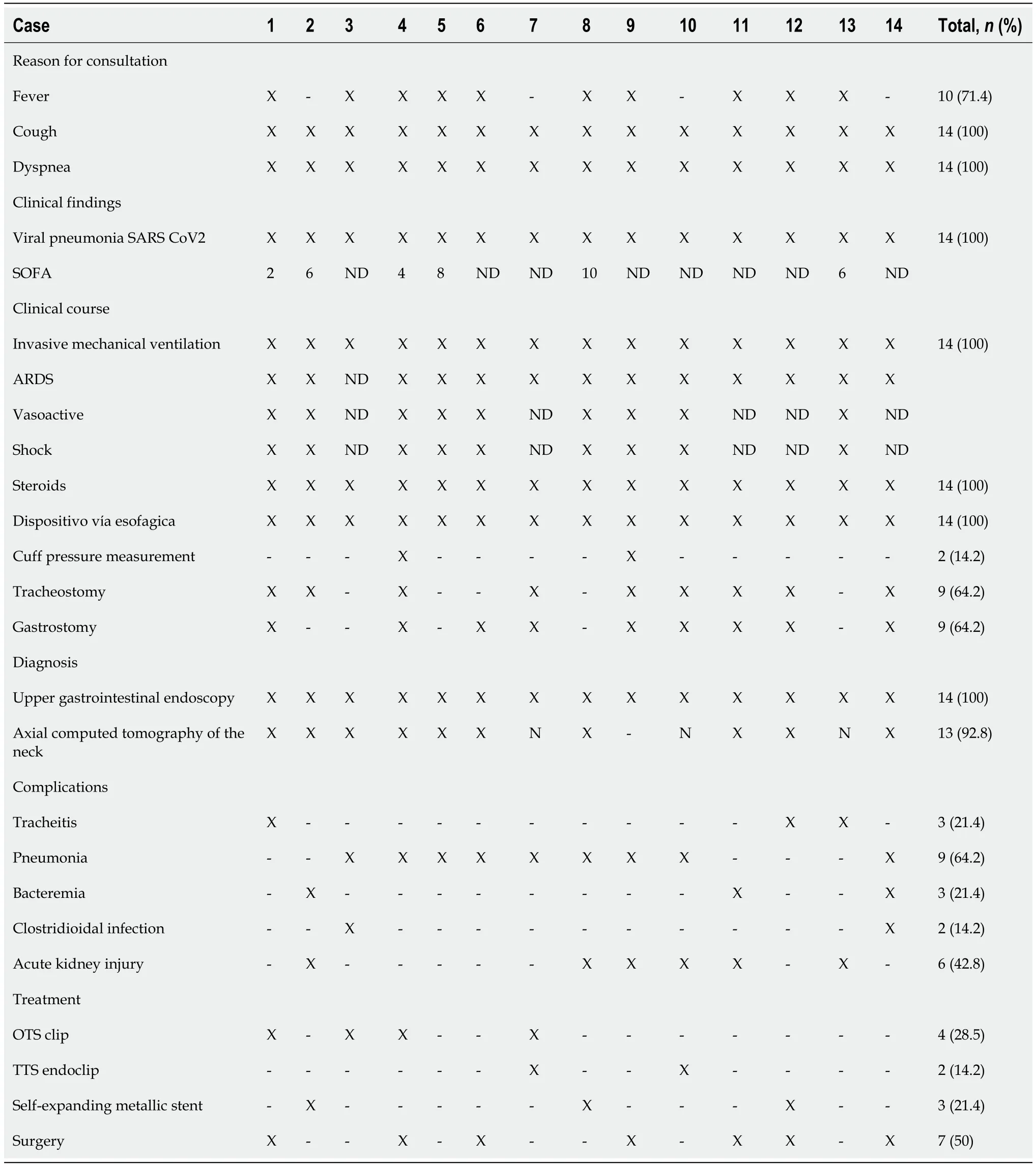
Table 2 Characteristics of patients with tracheoesophageal fistula in 2020-2021
The pressure of the endotracheal cuff was measured in only two patients (14.2%),being greater than 35 cmH2O in both cases.TEFs were documented by endoscopic study of the upper digestive tract (100%) and in some cases with three-dimensional reconstruction of neck computed tomography (71.4%).All TEFs were found in the proximal esophagus,with an average distance of 16.7 cm from the dental arch,and the average diameter was 18.2 mm (range 3 mm-40 mm) (Figure 1).
All of the patients had bacterial infectious complications,including tracheitis (21.4%),pneumonia (64.2%),and bacteremia (21.4%).Therefore,they required treatment with broad-spectrum antibiotics leading toClostridioides difficileinfection in 14.2% of the sample.Six patients developed terminal acute kidney injury requiring renal replacement therapy.For the closure of TEFs,eight patients were taken to temporary or definitive endoscopic treatment: Four needed over the scope (OTS) clips,achieving successful endoscopic closure in two.Clip placement failed in one of the patients due to tissue fibrosis;a recurring defect was documented in another patient.Three patients received temporary management with a fully coated metallic stent (SEMS),managing to completely cover the defect.Hemoclips (TTS endoclips) were used in two patients.In one patient,with a 3 mm TEF,adequate closure of the defect was achieved;while in another patient,temporary reduction in diameter was achieved,allowing further management with an OTS clip (Figure 1).In six patients,a surgical approach was indicated given the location and size of the fistula.Surgical management was also provided to the patient with failure to therapy with the OTS clip,achieving successful correction of the defect.On follow-up,recurrence of TEFs was observed in only one patient treated with an OTS clip,and an increase in the size of the fistula was detected,for which surgical therapy was considered,successfully closing the defect.Despite the efforts made,42.8% (6/14) died due to infectious complications,with two patients dying before receiving surgical management.
History of past illness
Comorbidities were found in 85.7% of the patients,with the most frequent being obesity/overweight (71.4%),diabetes mellitus (42.8%),and systemic hypertension (42.8%).
Physical examination
Half of the sample was composed by women with an average weight of 72.4 kg (body mass index [BMI] 27.4).The men had an average weight of 82 kg (BMI 26.6).The pressure of the endotracheal cuff was measured in only two patients (14.2%),being greater than 35 cmH2O in both cases.
Imaging examinations
Three dimensional reconstruction of neck computed tomography was performed in 13 patients (92.8%),identifying the presence of a fistula in 71.4%.At the time of diagnosis,all patients were on invasive mechanical ventilation,so esophagogram was not performed in any of them.
FlNAL DlAGNOSlS
TEFs were documented by endoscopic study of the upper digestive tract (100%) and in some cases with three-dimensional reconstruction of neck computed tomography (71.4%).All TEFs were found in the proximal esophagus,with an average distance of 16.7 cm from the dental arch,and the average diameter was 18.2 mm (range 3-40 mm) (Figure 1).
TREATMENT
For the closure of TEFs,eight patients were taken to temporary or definitive endoscopic treatment: Four needed OTS clips,achieving successful endoscopic closure in two (video 1).Clip placement failed in one of the patients due to tissue fibrosis;a recurring defect was documented in another patient.Three patients received temporary management with a fully coated metallic stent (SEMS),managing to completely cover the defect.Hemoclips (TTS endoclips) were used in two patients.In one patient,with a 3mm TEF,adequate closure of the defect was achieved,while in another patient,temporary reduction in diameter was achieved,allowing further management with an OTS clip (Figure 1).In six patients,a surgical approach was indicated given the location and size of the fistula.Surgical management was also provided to the patient with failure to therapy with the OTS clip,achieving successful correction of the defect.On follow-up,recurrence of TEFs was observed in only one patient treated with the OTS clip,and an increase in the size of the fistula was detected,for which surgical therapy was considered,successfully closing the defect.
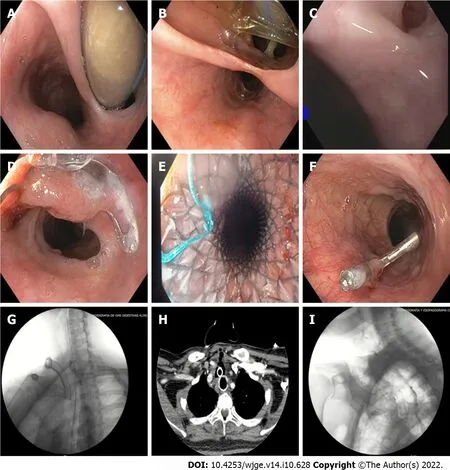
Figure 1 Tracheoesophageal fistulas: Diagnosis and management.
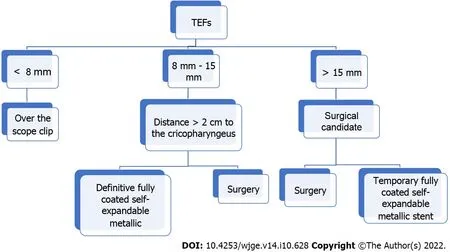
Figure 2 Suggested treatment algorithm.
OUTCOME AND FOLLOW-UP
Despite the efforts made,42.8% (6/14) of the patients died due to infectious complications,with two patients dying before receiving surgical management.
DlSCUSSlON
Acquired TEFs are a rare clinical entity,with incidence rates approaching 0.5%.Up to 75% of cases are due to trauma related to endotracheal cuff overinflation or prolonged mechanical ventilation[4,8,17].The pressure exerted by the endotracheal tube cuff erodes the tracheal mucosa,leading to ischemic destruction of the tracheal cartilage,which creates a communication with the esophageal wall[4,8].
The current health situation,due to the SARS-CoV-2 pandemic,which significantly increased cases of severe pneumonia and ARDS,led to a parallel increase in TEFs associated with prolonged endotracheal intubation.We found that 14 out of 894 patients undergoing mechanical ventilation for severe COVID-19 pneumonia,developed TEFs (incidence 1.56%).In most patients,several risk factors were simultaneously found;these included prolonged mechanical ventilation,hypotension,steroid use,diabetes mellitus,obesity,and excessive movement of the endotracheal tube due to frequent position changes (supine-prone)[18].We hypothesize that monitoring of the endotracheal cuff pressure was insufficient,possibly due to overcrowding in critical care units,as well as the exhaustion,anxiety,and depression developed by healthcare workers during the pandemic[19,20,21,22].
Spontaneous closure of TEFs is rare,and therefore requires the use of different treatment approaches,including endoscopic and surgical options[4,7,23].Among the endoscopic options is the use of fully coated metallic stents (SEMS),OTS clips,TTS endoclips,and suture systems among others[24-27].These procedures have allowed for high success rates (73%-83%) regarding closure of perforations,leaks,and gastrointestinal fistulas[28].However,due to a low incidence of TEFs,no consensus guidelines on the management of this entity currently exist,particularly concerning patients with SARS-CoV-2 infection.It has been reported that mechanical ventilation increases the risk for suture dehiscence.Furthermore,comorbidities and the critical condition of patients with severe COVID-19 pneumonia usually lead to deferral of surgical procedures until after mechanical ventilation withdrawal.This is why considering endoscopic interventions as initial management in critically ill patients with tracheoesophageal fistula associated with mechanical ventilation due to COVID-19 should be sought.
We present a treatment algorithm for this group of patients in Figure 2.Our approach is determined by the size and location of the fistula,using OTS clips for defects below the size of 8 mm.For lesions between 8 and 15 mm,we suggest to use SEMS as long as the fistula is more than 2 cm distal to the cricopharyngeus where the stent can be properly fixed.In lesions larger than 15 mm,we propose upfront surgical treatment,as well as when the fistulas are less than 2 cm from the cricopharyngeus (because at this distance the stent may lead to foreign body sensation).When the patient is not a good surgical candidate and has lesions larger than 15 mm located more than 2 cm away from the cricopharyngeus,a fully SEMS can be placed as bridging therapy until the patient becomes stable and in better condition for surgical treatment.Although we have a small sample size,to the best of our knowledge,this is the first study to illustrate the management of this type of patients in the context of the coronavirus pandemic.
CONCLUSlON
Due to the significant increase in diagnosis of TEFs in patients with severe pneumonia due to COVID-19,and the high frequency of risk factors for TEFs in these patients,we recommend early identification and prevention of these conditions,in addition to frequent measurement of the endotracheal cuff pressure.If possible,we recommend periodic evaluation of the tracheal mucosa by bronchoscopy to identify early lesions that could lead to the development of TEFs.Regarding treatment,we suggest providing initial endoscopic management in small fistulas (below 15 mm) or until optimal conditions for surgical management are met (if larger than 15 mm).Definitive endoscopic treatment may be offered according to the size and location of the fistula.
FOOTNOTES
Author contributions:Gomez M was responsible for the revision of the manuscript for important intellectual content;Gallego D and Ruiz O reviewed the literature and contributed to manuscript drafting;all authors were the patient’s gastroenterologists;all authors issued final approval for the version to be submitted.
lnformed consent statement:Informed consent was obtained from each of the patients or their legal representatives.
Conflict-of-interest statement:The authors declare that they have no conflict of interest to disclose.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016),and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Colombia
ORClD number:Martin Alonso Gomez Zuleta 0000-0002-2377-6544;Daniel Mauricio Gallego Ospina 0000-0002-0483-2723;Oscar Fernando Ruiz 0000-0001-6555-1573.
Corresponding Author's Membership in Professional Societies:Asociación Colombiana De Gastroenterologia;American Society for Gastrointestinal Endoscopy.
S-Editor:Ma YJ
L-Editor:Wang TQ
P-Editor:Ma YJ
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Endoscopic palliation of malignant biliary obstruction
- Gastric intestinal metaplasia development in African American predominant United States population
- Water-jet vs traditional triangular tip knife in peroral endoscopic myotomy for esophageal dysmotility:A systemic review and metaanalysis
- Laparoscopic Janeway gastrostomy as preferred enteral access in specific patient populations:A systematic review and case series
- Hemostasis of massive bleeding from esophageal tumor:A case report
- Cronkhite-Canada syndrome:First case report from Egypt and North Africa
