Endoscopic palliation of malignant biliary obstruction
2022-10-25AndrewCanakisMichelKahaleh
Andrew Canakis,Michel Kahaleh
Andrew Canakis,Department of Gastroenterology and Hepatology,University of Maryland School of Medicine,Baltimore,MD 21201,United States
Michel Kahaleh,Department of Gastroenterology and Hepatology,Robert Wood Johnson Medical Center,New Brunswick,NJ 08901,United States
Abstract Malignant biliary obstruction often presents with challenges requiring the endoscopist to assess the location of the lesion,the staging of the disease,the eventual resectability and patient preferences in term of biliary decompression.This review will focus on the different modalities available in order to offer the most appropriate palliation,such as conventional endoscopic retrograde cholangiopancreatography,endoscopic ultrasound guided biliary drainage as well as ablative therapies including photodynamic therapy or radiofrequency ablation.
Key Words: Biliary obstruction;Endoscopic retrograde cholangiopancreatography;Endoscopic ultrasonography;Stenting;Ablation therapy
lNTRODUCTlON
Palliation of unresectable malignant biliary obstruction is recommended to achieve biliary decompression and allow for symptomatic relief (i.e.,jaundice and pruritis).Minimally invasive endoscopic biliary drainage techniques have garnered significant attention as an effective patient friendly treatment option that can improve one’s quality of life when comparing it to the more invasive nature of surgery and/or percutaneous transhepatic biliary drainage (PTBD) approaches.At the present,endoscopic retrograde cholangiopancreatography (ERCP) serves as the cornerstone of biliary decompression.However,in instances of failed or inaccessible cannulation endoscopic ultrasound guided biliary drainage techniques have emerged as second line options with comparable clinical outcomes.Furthermore,localized endobiliary ablative toolsviaphotodynamic therapy and radiofrequency ablation have proven to be supplementary methods to palliate symptoms and optimize stent patency.As such this state-of-the-art review will shed light on palliative endoscopic modalities for the effective management of biliary drainage.
CONVENTlONAL ERCP
Malignant biliary obstruction can be categorized as a distal or hilar obstruction.This distinction is important as management options and outcomes differ.As such,the following two sections are subdivided to describe the ERCP approach in draining malignant distal biliary obstruction (MDBO) and malignant hilar biliary obstruction.
MDBO
MDBO represents a wide clinicopathologic spectrum of intrinsic and extrinsic bile duct compression arising within the pancreaticobiliary system.The most common etiologies are pancreatic adenocarcinoma and cholangiocarcinoma;in fact,up to 70% of patients with pancreatic cancer present with distal biliary obstruction[1,2].Since the majority of patients are diagnosed at advance stages,managementviapalliative endoscopic decompression is increasingly encountered.
ERCP with transpapillary stenting is the gold standard for decompressing unresectable MDBO with a success rate of 90%-95%[3,4].Palliative endoscopic biliary drainage is indicated as a means to treat cholangitis while providing symptomatic relief with improved quality of life measures[5,6].As an established therapeutic modality for over 40 years,ERCP has emerged as a more effective and less invasive option compared to surgery and PTBD.While surgical bypass may decrease rates of recurrent jaundice,it is associated with a significant morbidity and mortality[2,7,8].A meta-analysis of five randomized controlled trials (RCT) (379 patients) found that post-operative complications and 30 d mortality (16.3%vs9.6%) were higher in surgical cohort[8].In general many of these patients are poor operative candidates,whereby complications associated with surgical intervention can delay palliative chemotherapy options as well.Similarly,ERCP is often preferred over PTBD due to lower rates of adverse events,fewer re-interventions,decreased costs,shorter duration of hospital stay,and the lack of an external drain needed[4,6,9].A large national database comparing 7445 ERCPsvs1690 PTBD procedures at community and tertiary care centers associated lower adverse events with ERCP (8.6%vs12.3%,P< 0.001) regardless of the centers PTBD volume of expertise[9].There is also a risk of seeding metastasis with PTBD[10].That being said,PTBD is typically used as rescue therapy in cases of ERCP failure (which we highlight later on the EUS-BD section).
Stent selection
In order to ensure long term stent patency,placing a self-expandable metal stents (SEMS) is a wellestablished and cost-effective approach for patients with a life expectancy greater than 3 mo[4,11,12].The type of stents available include covered self-expandable metal stents (CSEMS) and uncovered selfexpandable metal stents (USEMS).The optimal stent type remains uncertain due to varying RCTs with mixed results (Table 1)[13-21].A recent meta-analysis of 11 randomized controlled trials involving 1272 patients (643 CSEMS and 629 USEMS) reported no significant difference in rates of recurrent biliary obstruction or mortality[22].While there was a 32% risk reduction for stent failure and mortality favoring CSEMS,this possibly benefit was offset but higher rates of sludge formation and stent migration[22].Another meta-analysis of 9 RCTs (1061 patients) found no difference in length of stent patency[23].In terms of adverse events (including pancreatitis and cholecystitis),there appears to be no major differences based on stent type[23,24].
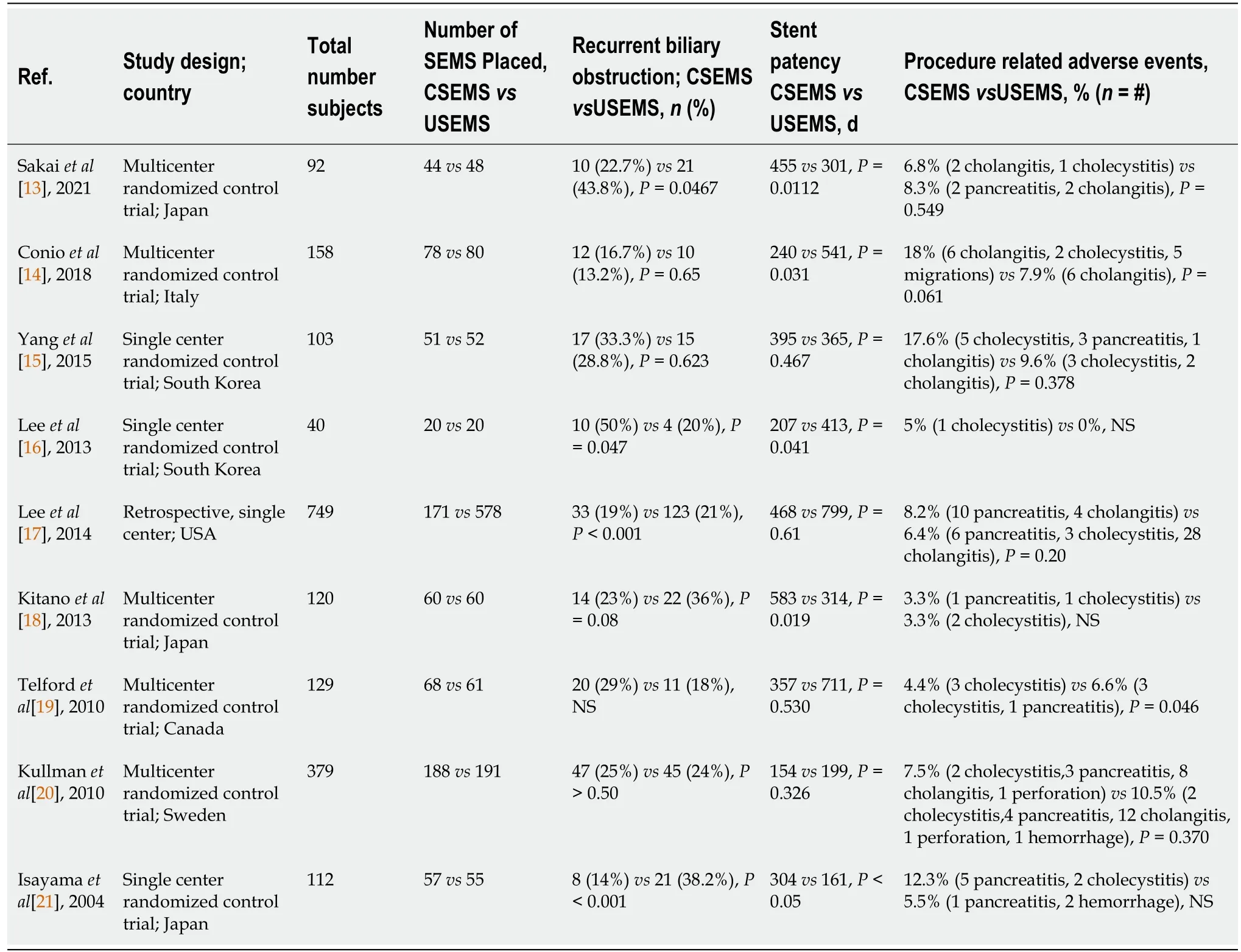
Table 1 Covered versus uncovered self-expandable metal stents in malignant distal biliary obstruction
To combat tumor ingrowth and prolong stent patency,paclitaxel-incorporated drug eluting metal stents have been developed in South Korea.The stent is coated with membrane layers of polytetrafluoroethylene to prevent bile acid degradation and sodium caprate to enhance paclitaxel delivery[25].A meta-analysis of 5 studies comparing drug eluting stents (197 patients) to SEMS (151 patients) reported a pooled stent patency of 168 d and 149 d,respectively[26].There were no major differences in rates of cholangitis (17%vs15%) or cholecystitis (6.5%vs5.0%).Further studies are needed to determine if these drugs eluting stents can alter the management of MDBO.None of those stents have received FDA clearance so far.
Malignant hilar lesions
Malignant hilar obstruction poses its own set of unique challenges,especially since the endoscopic intervention is often technically challenging.In a large study analyzing 59437 ERCPs,successful outcomes and reduced adverse events were associated with high volume endoscopists and centers[27].This highlights the importance of managing these patients in a high volume multidisciplinary center,as technical failure can significantly shorten the median length of survival compared to successful biliary drainage (8.7 movs1.8 mo,P< 0.001) in type III and IV hilar cholangiocarcinoma[28].
Malignant hilar strictures can be categorized based on their extent of hilar and/or hepatic duct involvementviathe Bismuth-Corlette classification system[29].Since the majority of these strictures are inoperable with varying degrees of anatomical complexity,this classification can help guide the palliative approach for biliary decompression[30].In general Bismuth grades I/II are amenable to ERCP,however grades III/IV are typically managed by a combination of ERCP and/or PTBD[4].Choosing between ERCP and PTBD for types III/IV was analyzed in a meta-analysis of 9 studies (n=546 patients) where there was a higher success rate seen with PTBD over ERCP in types III/IV with comparable rates of adverse events and 30 d mortality,unfortunately the skillset of the endoscopists involved in that study was not provided[31].Another study of 110 patients with inoperable Bismuth type III/IV,found that failure of endoscopic stenting was associated with an acute angulation at the common bile duct and intrahepatic duct[32].While pre-operative imaging may help guide an approach,PTBD can be technically challenging in the setting of liver metastases,ascites,and if intrahepatic bile duct is not fully dilated;thus,ERCP remains the preferred modality for drainage[33].
Choosing between the two modalities is based on multiple factors ranging from local expertise,risk of infection,possible seeding by PTBD,life expectancy,comorbidities and patient preference regarding an external catheter[31].While there have been studies with mixed results favoring ERCP[34] and PTBD[35,36] the optimal stenting technique should be guided by achieving ≥ 50% of total liver volume drainage in order to relieve jaundice and reduce the risk of cholangitis[37].Previously it was thought that draining 25% of liver volume was sufficient;however another study found that at least 50% drainage was a predictor of effective drainage and longer overall survival (199 dvs59 d),especially in Bismuth type III strictures[38].Another retrospective study of 78 patients with unresectable type II-IV hilar strictures found that effective liver volume drainage correlated with liver function: in which biliary drainage ≥ 33% can be obtained with preserved liver function and ≥ 50% with impaired liver function[39].In addition to liver function,the anatomical difference in liver volume may also effect drainage,as the right lobe accounts for 55%-60% of volume,followed by 30%-35% in left and 10% of the caudate lobes[40,41].Consequently,utilizing bilateral or multi-sectoral stenting is typically advised in high grade strictures based on varying anatomical involvement of disease[4].
Unilateral vs bilateral drainage
Choosing unilateral and/or bilateral stenting is typically based on the patient’s presentation,degree of obstruction and local anatomy.Pre-endoscopic imaging is also imperative to understand and calculate the liver volume drainage needed.It is well established that one stent provides sufficient drainage in Bismuth I.However,for Bismuth II-IV there is no clear consensus.
A recent metanalysis of 21 studies with 1292 patients comparing both techniques noted similar rates of clinical efficacy and complications for both unilateral and bilateral drainage though there were higher rate of technical success in the unilateral group (97%vs89%,P=0.003)[42].However,these results were not analyzed based on the bismuth classification or etiology of obstruction.A multitude of studies have compared unilateralvsbilateral drainage with similar rates of success[43-47].One multicenter RCT of 133 patients with Bismuth grades II-IV reported no major differences in technical success,however the bilateral group had longer duration of stent patency (252 dvs139 d) and fewer rates of reinterventions (42.5%vs60.3%,P=0.049)[43].Similarly,a retrospective study of 141 patients found that bilateral drainage portended a longer survival advantage (255 dvs80 d,P< 0.0001)[45].Such advantages come at the expense of higher rates of complications and risk of death with bilateral drainage,irrespective of Bismuth grade[44].
Bilateral stenting techniques
In order to ensure adequate drainage,bilateral stenting techniques using a stent-by-stent (SBS) or stentin-stent (SIS) have been utilized,though there is no clear consensus on what technique is superior due to limited data.Following deployment of the intrahepatic bile duct a second stent can be placed parallel using the SBS method or sequentially through the mesh within in the initial stent using the SIS approach[37].These are technically challenging procedures that require high levels of experience with technical success rates ranging from 73% to 100%[33].One retrospective comparing SIS (n=40) to SBS (n=24) reported similar rates of technical success (100%vs96%),clinical success (93%vs96%) and rates of recurrent biliary (48%vs43%)[48].Though there was a higher rate of post-procedural related pancreatitis exclusively seen in the SBS group[48].At the same time another study found no significant difference in early (31.6%vs22.7%) or late (36.8%vs50.0%) complications for SBSvsSIS[49].This was also demonstrated in a meta-analysis of 158 patients that found no significant difference in technical success,complications or stent occlusion[50].Many centers prefer the SBS approach since deploying multiple stents is relatively easier and in cases of stent dysfunction reintervention is possible[33,51].Reintervention with plastic stents placed inside SEMS is also possible after the SIS approach.Recently a newly designed Y-shaped bilateral endoscopic stent has been investigated,though further studies are needed to better define its role in clinical practice[52-54].At our center we use the SBS approach preferentially.
ENDOSCOPlC ULTRASOUND GUlDED BlLlARY DRAlNAGE
Since its introduction in 2001,EUS-guided biliary drainage (EUS-BD) has emerged as an effective and reliable alternative for managing malignant biliary obstruction[55].While ERCP remains the current gold standard,it is associated with a failure rate of up to 10%-especially in cases of surgically altered anatomy (SAA),tumor infiltration/obstruction,periampullary diverticulum,prior duodenal stenting or stenosis[4,56,57].However,unsuccessful ERCPs may vary based on institutional experience.Two studies with extensive ERCP expertise reported unsuccessful canulation in 0.60% to 0.68% of patients[58,59].Of note,one of those studies described 3 out of 524 failed ERCPS in native papillas with limited instances of SAA (n=2) or duodenal obstruction (n=3)[59].On the other hand a large prospective study of 4561 patients from 66 hospitals (with varying degrees of expertise) found that 17.2% of ERCPs were unsuccessful[60].The European guidelines recommend repeating ERCP in select patients,ideally two to four days after the first ERCP,with success rates up to 82%[4].
In instances of ERCP failure where salvage therapy is needed,PTBD has conventionally been pursued;however,as mentioned above it is associated with a significant morbidity,decreased quality of life and need for re-interventions.In this context EUS-BD emerged as another less invasive option with fewer procedure related adverse events (8.80%vs31.22%,P=0.022) and re-intervention rates (0.34vs0.93,P=0.02) when compared with PTBD in a randomized open label study[61].A meta-analysis with 483 patients confirmed these findings and found that while there was no difference in technical success,the EUS-BD group was associated with better clinical success,less reinterventions and fewer postprocedure adverse events[62].
EUS-BD is an appealing approach,though at the moment it is a specialized technique limited to a high-volume centers.In this regard understanding the associated learning curve is needed before its widespread applicability.A few studies have looked into this,and there appears to be a clear association with significantly decreased adverse events with increased operator procedural volume over time[10,63-67].In a single center study with 215 procedures performed by one experienced endoscopist over a 6.6 year period,there was a notable decrease in adverse events as procedural volume increased each year[67].Other studies have proposed that 33 and 100 cases were required to achieve technical proficiency and mastery,respectively[65,66].
The routes of biliary decompression can be accomplished through a rendezvous (RV),antegrade or transluminal (intra- or extrahepatic) approach[3].The application of EUS-RV is limited to intact gastroduodenal anatomy,when conventional ERCP cannulation fails,in which a guidewire is accessed across the anastomosis in an antegrade fashion-this salvage approach is limited by a success rates of 74%-80% with a relatively high major adverse event rate of 11%[3].Antegrade stenting has also fallen out of favor as it can be cumbersome with a limited technical success rate of 77%[3].The puncture site (transgastric into left intrahepatic duct) allows for guidewire placement across the stricture/papilla without the need for fistula tract formation at the puncture site[68].In instances of technical failure,antegrade stenting can be converted to transmural or PTBD[68].Overall,direct transmural drainage is preferredviaextrahepatic or intrahepatic approach.
Extrahepatic approach
EUS-guided choledochoduodenostomy (EUS-CDS) is a transluminal approach that creates a fistula between the duodenum and extrahepatic bile duct using a fully covered SEMS or lumen-apposing metal stents (LAMS)[68].This biliodigestive anastomosis provides optimal palliation of MDBO;however it cannot be performed in cases of proximal obstruction or instances of gastric outlet obstruction where access to the duodenal bulb may be hindered[69].A recent multicenter retrospective study compared EUS-CDS (n=28) to PTBD (n=58) and found that EUS-CDS was associated with higher clinical success (84.6%vs62.1%,P=0.04) with significantly lower rates of reintervention (10.7%vs77.6%,P< 0.001)[70].As a clinically effective technique (up to 96.2%),EUS-CDS has emerged as reliable alternative with acceptably low adverse events (10.5%)[71].
Recent studies have increasingly been using LAMS,which may be attributing to lower rates of stent malfunction.A large multicenter cohort in the United Kingdom and Ireland found that the technical success,clinical success,adverse events and reintervention rates using LAMS were 90.8%,94.8%,17.5%,and 8.3%,respectively[72].Initially,plastic stents were used when EUS-CDS was first introduced.However,CSEMS quickly replaced plastic stents as a means to reduce bile leaks and stent occlusion[3] with significantly lower rates of adverse events (13.0%vs42.8%,P=0.01) and improved stent patency when compared to plastic stents[73-75].At the moment the use of CSEMSvsLAMS varies from center to center.The large,tubular and rigid shape of CSEMS can theoretically increase the risk of stent migration[3].In this context,LAMS were designed as a short,dumbbell shaped stents wit bilateral flanged ends which provide anti-migratory properties by anchoring across non-adherent lumens[3].Further improvements were made with the development of an electrocautery-enhanced delivery system that enables a faster single step “free-hand” puncture which has led to high rates of technical success by eliminating the need for accessory changes[76].However,two recent studies comparing LAMSvsSEMS found no differences in technical and clinical success or postprocedure related adverse events[77,78].
Intrahepatic approach
In instances of proximal malignant obstruction EUS-guided hepaticogastrostomy (EUS-HGS) creates a fistulized tract between the gastric wall and left intrahepatic duct.Its technical feasibility was first introduced in 2004 and since then it has become a widely used technique[79].The European Society of Gastrointestinal Endoscopy recommends placement of partially or fully covered SEMS for drainage of malignant obstruction[68].HGS can be performed where there is dilation of the left intrahepatic duct with segment III being the preferred puncture site[80].There are a few contraindications to the procedure which include gastric wall tumor infiltration,large volume ascites,and coagulopathy[80,81].Its role in hilar obstruction is reserved for specific cases as drainage from the left intrahepatic duct does not equate to drainage of a right sided obstruction[69].A study described access from the proximal duodenum to right intrahepatic duct (hepaticoduodenostomy) for cases of isolated right sided obstruction (with a technical success 100% and clinical success 83%)[82],but widespread use of this technique has not been adopted due to difficulty with scope positioning and proper identification of the duct[83].
In general,this intrahepatic approach has been favored for distal malignant biliary drainage.The HGS route is associated with a lower risk of bile leakage as the localized liver parenchyma around the fistula site can provide a tamponade effect[73].A prospective randomized trial comparing HGS (n=24) and CDS (n=24) in MDBO following failed ERCP reported a higher clinical success rate in the HGS group (91%vs77%) at the expense of slightly more adverse event rates (20.0%vs12.5%)[84].A multitude of studies have compared CDS and HGS approaches (Table 2)[64,84-95].A meta-analysis of 10 studies comparing HGS (n=208) and CDS (n=226) found no difference in technical success (94.1%vs93.7%),clinical success (88.5%vs84.5%),or rates of adverse events[96].
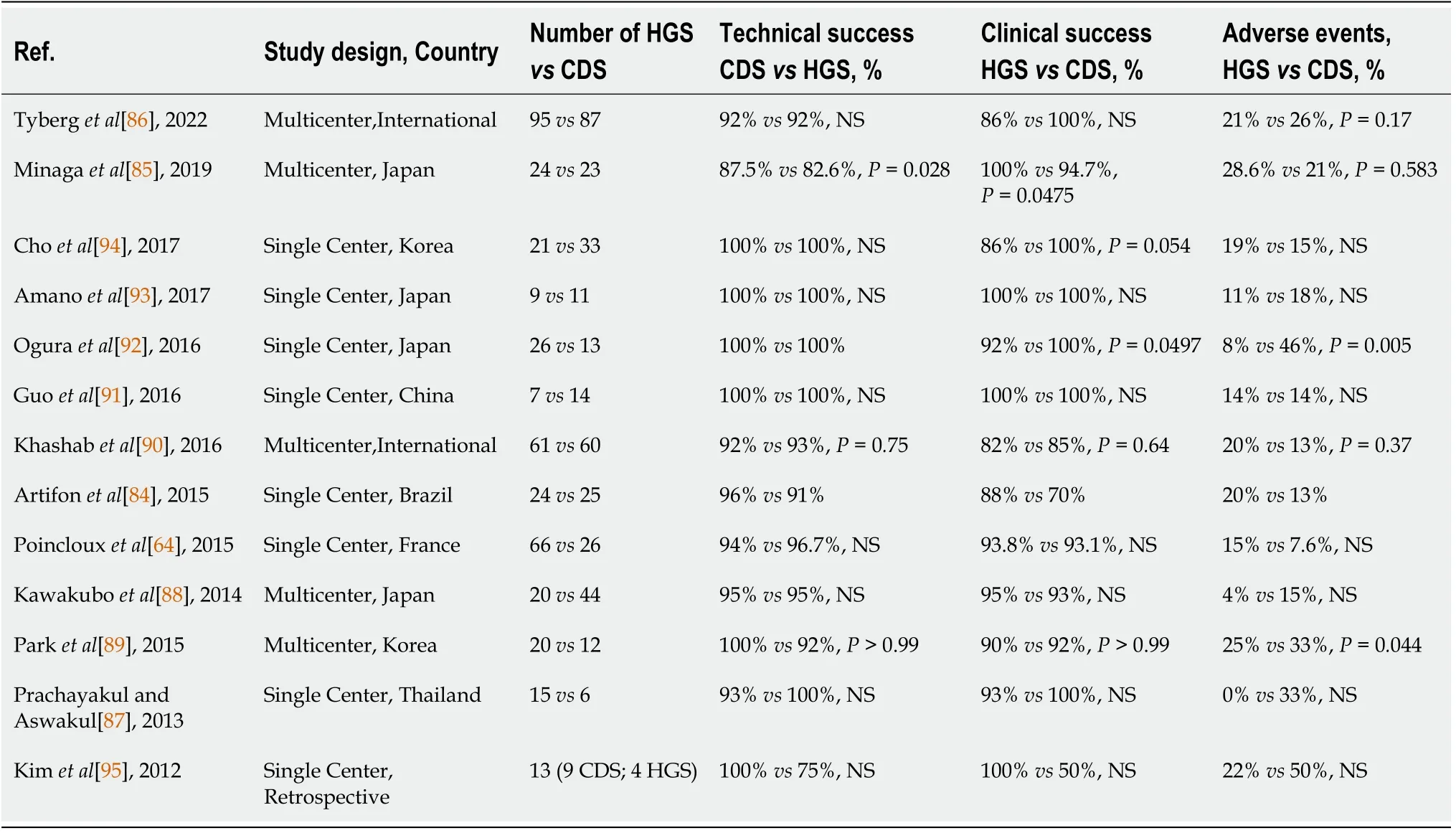
Table 2 Comparative studies of endoscopic ultrasound guided hepaticogastrostomy and choledochoduodenostomy
Recently,a large single center study of 215 patients (130 malignant lesions,85 benign lesions) undergoing transhepatic biliary drainage by one endoscopist showed that the HGS approach used in up to 90% of cases was technical and clinically effective with few instances of reintervention (17.4%) needed within the malignant cohort that survived > 6 mo[67].In this study,the endoscopist preferred HGS over CDS to decrease the risk of bleeding,stent misdeployment and potential making pancreatic surgical resection more difficult[67,97].Of note,a study of 23 patients with concomitant duodenal and biliary obstruction undergoing single session EUS-HGS and gastrojejunostomy found that one patient with pancreatic cancer underwent successful pancreaticoduodenectomy 168 days post-biliary drainage and the fistula remained in situ with no complications[98].On the other hand,in a large multicenter study comparing HGS (n=24 ) to CDS (n=23),the authors preferred CDS as it takes advantage of the anatomical proximity between the duodenal bulb and extrahepatic duct,by which puncture can be easier with shorter procedure times and less guidewire manipulation[85].Another large international study of 182 patients (95 HGS,87 CDS) suggested that CDS was associated with being 4.5 times more likely to achieve longer stent patency at the expense of higher adverse events,which may influence decisions based on patients survival[86].In light of advancements with oncologic care,the prospect of reduced long reintervention may steer one to use CDS,especially since reintervention is easier due to shorter stent size,cannulation and steering in the duodenum[83].
While both techniques have acceptable outcomes,there is still no clear choice.Yet tailoring the technique based on anatomical features,altered anatomy,duodenal stenosis and dilated bile ducts may help endoscopists choose the right route for each patient[57,99].A novel individualized algorithm was proposed based on patient anatomy following failed ERCP where the authors suggested using crosssectional imaging to determine if an intrahepatic or extrahepatic approach based on the presence or absence of intra-hepatic biliary tree dilation[99].The algorithm favored an intrahepatic approach if possible as a means to preserve anatomy.Yet,if intrahepatic dilation was technically unsuccessful,they recommended converting to an extrahepatic approach.In their prospective cohort of 52 patients,there was a technical success rate of 96% (35 intrahepatic,17 extrahepatic).
COMPARlNG ERCP AND EUS-BD FOR MANAGEMENT OF MALlGNANT BlLlARY OBSTRUCTlON
As detailed above,ERCP remains the first choice when treating malignant biliary obstruction.Its widespread use and high success rate,especially in expert hands,makes it an effective modality for biliary decompression.The application of EUS-BD as a rescue therapy has proven to be a reliable tool with high technical and clinical success rates with moderate adverse event rates.Furthermore,instances of SAA or duodenal invasion may preclude the use of ERCP,and EUS-BD has gained momentum as the preferred therapy (as opposed to PTBD).
There is growing interest in using EUS-BD as a potential first line approach.A multicenter retrospective study comparing ERCP (n=104) to EUS-BD (n=104) demonstrated similar rates of technical success (94%vs93%) and adverse events (8.65%vs8.65%);though 4.8% of the ERCP cohort experienced post-procedural pancreatitis[100].EUS-BD does have an added benefit of shorter procedural times with the possibility of longer stent patency by avoiding the diseased bile duct in question[3,101].Additionally,in cases of an indwelling gastroduodenal stent,EUS-BD has been proven as a technical and clinically superior option when compared to endoscopic transpapillary stenting[102].A recent meta-analysis of 9 studies with 634 patients found no significant differences between technical and clinical success,though the EUS-BD cohort had fewer rates of reintervention[103].
ABLATlON THERAPY OF THE BlLE DUCT
The goals of palliative biliary drainage aim to improve obstructive symptoms and quality of life.Yet endoscopic biliary decompression may only provide temporary relief;hence,the ability to provide supplemental biliary ablation as means to induce local tumor necrosis,optimize stent patency,palliate symptoms and possibly enhance long term survival have been investigated with photodynamic therapy (PDT) and radiofrequency ablation (RFA)[104].
Photodynamic therapy
PDT utilizes a photosensitizing agent (which is activated by laser light) to ablate tumor tissueviaapoptosis,necrosis,and an immunomodulatory effect[105].The porphyrin phototoxic substance is given intravenously 3-4 d prior to the procedure to allow for preferential accumulation in the malignant tissue-during this period patients are advised to stay in a darkened room to avoid an accidental inflammatory reaction in normal tissue if exposed to light[106,107].Next a guidewire and catheter position the fiberoptic probe in the bile duct where laser light at certain wavelengths (typically 630 nm) trigger the photosensitizing agent for 750 sec to generate free oxygen radicals that destroy the tumor bed and/or stricture[106,108,109].An added benefit to this local apoptotic and inflammatory cascade is that these light waves can refract to the proximal biliary tree which are often beyond reach of the guidewire[110].Following PDT,a stent is often placed.This highly specialized technique is limited to a few centers.
PDT has been shown to improve overall survival,stent patency and quality of life in unresectable cholangiocarcinoma.A sentinel PDT study in 2003 prospectively randomized 20 patients to PDT plus biliary stenting and 19 with stenting alone,and found that the PDT significantly increased the median survival (493 dvs98 d) while also improving quality of life and biliary drainage[111].Similar findings of improved survival were also confirmed in another randomized trial[112].Another retrospective comparative study of 48 patients with unresectable cholangiocarcinoma (19 PDT with stent versus 29 with biliary stent only) demonstrated a significant survival advantage (16.2 movs7.4 mo) with only three adverse events related to skin phototoxicity that were treated with topical therapy[113].The survival benefit of PDT plus stenting has been confirmed in three meta-analyses[114-116].Of note,while one of these studies reported an improved survival rate favoring the PDT cohort (525vs146),the analysis was limited by its inclusion of endoscopically and percutaneous administration of PDT and/or biliary stents[116].That being said all studies favored PDT’s improved survival benefit,with a relatively low adverse event rate of 11% specific to phototoxic reactions (i.e.,blisters,erythema,and pruritis)[115].In order to avoid such a reaction,it is recommended that patients avoid direct sunlight for 4-6 wk after the procedure[104].
In light of these favorable findings,additional studies have been pursued to characterize the potential benefits of stent patency and effect of combination systematic therapy.A retrospective of 33 patients with unresectable disease found that the PDT cohort (n=18) had noticeable longer periods of stent patency (224 dvs177 d,P=0.002) by which the authors felt that PDT may induce tumor “remodeling” to lessen cholestasis and prolong biliary decompression[117].A synergistic effect between PDT and systematic chemotherapy has also been prospectively[118] and retrospectively confirmed to enhance overall survival[119,120].In on such study,96 patients with unresectable perihilar and distal CCA were stratified by treatment type where median overall survival was 20 mo,15 mo,and 10 mo in the combination PDT plus chemotherapy (n=36),PDT alone (n=34),and chemotherapy alone (n=26) groups,respectively[120].
These positive findings must also be analyzed in context of the limitations of PDT use.It is a complex and exceedingly expensive procedure that typically is only performed in highly specialized centers[2].The phototoxic side effects may not acceptable to patients,especially since minimizing direct sunlight one month after the procedure could impair the quality of life in a patient with a potentially short life expectancy[110].While the last author in this present review has pioneered early PDT studies,we feel that the lack of FDA approval of this therapy,in the biliary tree,has made this therapy very difficult to be offered outside of specialized centers.
Radiofrequency ablation therapy
RFA uses electromagnetic energy and high wave frequencies to deliver thermal energy to targeted tissues[121,122].This localized thermal energy induces direct coagulative necrosis and an indirect localized inflammatory response and T-lymphocyte activation which have anti-tumor properties[110,122].Intraductal RFA can be performed during a conventional ERCP where a RFA catheter can pass over the guidewire in order to place the bipolar probes upstream from the stricture site,whereby ablation is applied with 7-10 watts for 1-2 min bursts,along the length of the stricture[104,123].Afterwards the bile duct is cleared with a balloon sweep to remove residual debris and necrotic tissue followed by placement of plastic or metal stent to maintain adequate drainge[104,123].Of note,RFA can also be used with balloon enteroscopy-assisted ERCP[124] or an EUS-guided HGS approach[125,126].
The indication for endobiliary RFA is to improve stent patency and survival in cases of inoperable malignant strictures[106,123].In 2011,a prospective pilot study analyzed the utility of RFA in 21 patients with unresectable malignant biliary obstruction,and found that biliary patency was maintained by 20 and 16 patients at 30 and 90 d,respectively with no adverse events related to RFA[127].However,a subsequent single center retrospective study of 66 patients demonstrated no added benefit in prolonged stent patency when comparing metal stenting with RFA to stenting alone[128].Of note,this study did not differentiate their findings based on the stent used.Another study found a significant improvement and durability of stricture diameter using plastic (n=6) and metal stents (n=14)[129].As such,analyzing endobiliary RFA according to the type of stent used may allow for a better interpretation of stent patency;as etiology of recurrent biliary obstruction varies from sludge formation,migration and tumor ingrowth for plastic stents,covered SEMS and uncovered SEMS,respectively[123,130].
Plastic stents are often used if repeated RFA sessions are planned.Two recent RCTs have examined the stent patency of RFA and plastic stents with conflicting results[131,132].In one study,of 65 patients (32 RFA plus plastic stent,33 plastic stent alone),stent patency was significantly longer (6.8 movs3.4 mo) with a higher survival time (13.2 movs8.3 mo) favoring the RFA and plastic stent arm[133].While the other RCT also reported a higher survival time (14.3 movs9.2 mo) there was no significant difference in stent patency or jaundice control in either group[134].One possible reason for the discrepancy is that in the first RCT by Yanget al[133] patients underwent stent exchange every 3 mo,while the study by Gaoet al[134] only performed a stent exchange as clinical indicated.In our practice we offer systematic stents revision at three months interval.
The use of SEMS is largely depending on the patient’s life expectancy and unresectability.Both uncovered and covered SEMS have been investigated with mixed results[131,132,135].A retrospective[131] and RCT[132] examining USEMS,found no significant differences in stent patency.Meanwhile,a single center retrospective study using UCSEMS and CSEMS in a cohort of 31 patients favored the use of either stent with RFA with prolonged stent patency (220.0 dvs106.5 d)[135].One meta-analysis of nine studies with 505 patients demonstrated a favorable mean stent patency of 50.6 d with improved survival in those undergoing RFA with SEMS compared to SEMS alone[136].However,these findings should be interpreted with caution as four of these studies used a percutaneous route for RFA.In this context,another meta-analysis of 263 patients undergoing endoscopic RFA showed that strictures improved by 3.5 mm when using RFA with a median stent patency of 7.6 mo[137].Yet,the authors did not stratify their findings based on the type of stent used.
While the findings of stent patency and survival benefit are confounded by study heterogeneity and route of RFA,there is a likely benefit of stent patency and overall survival with RFA in malignant biliary obstruction.In fact a recent RCT found that a combination of oral 5-fluoouracil and RFA improved the median overall survival (16 movs11 mo) and period of stent patency (6.6 movs5.6 mo)[138].With more wide spread use,developments of newly automatic temperature controlled RFA systems[139] and endoluminal devices[140] have produced favorable results pertaining to both stent patency and survival.Interestingly,RFA appears to be a relatively safe procedure with few instances of cholecystitis (10%),cholangitis (6.2%),and pancreatitis (2.1%) that did no differ significantly when compared to stenting alone[107,136].
Only a handful of studies have directly compared RFA to PDT (Table 3).One retrospective study found no statistically significant difference in the survival benefit between RFA (n=16) and PDT (n=32) in their cohort of unresectable cholangiocarcinoma (9.6 movs7.5 mo)[141].However,the other retrospective study showed that RFA was associated with better short-term effects (i.e.,reduction in bilirubin with fewer unplanned stent replacements)[142].A recent meta-analysis of 55 studies comparing PDT (n=1149),RFA (n=545),and stent-only strategy (n=452) found that PDT was associated with an improved overall survival rate (11.9 movs8.1 movs6.7 mo,respectively) and decreased 30-d mortality (3.3%vs7.0%vs4.9%,respectively)[143].Though PDT did display higher rates of cholangitis (23.4%vs9.5%) and liver abscess (4.9%vs2.6%) when compared to RFA.The authors felt that RFA may be favored in the setting of lower adverse events,decreased costs (Photofrin dose $37000vsRFA catheter $1200) and similar lengths of stent patency (PDT 6.1 movsRFA 5.5 mo).
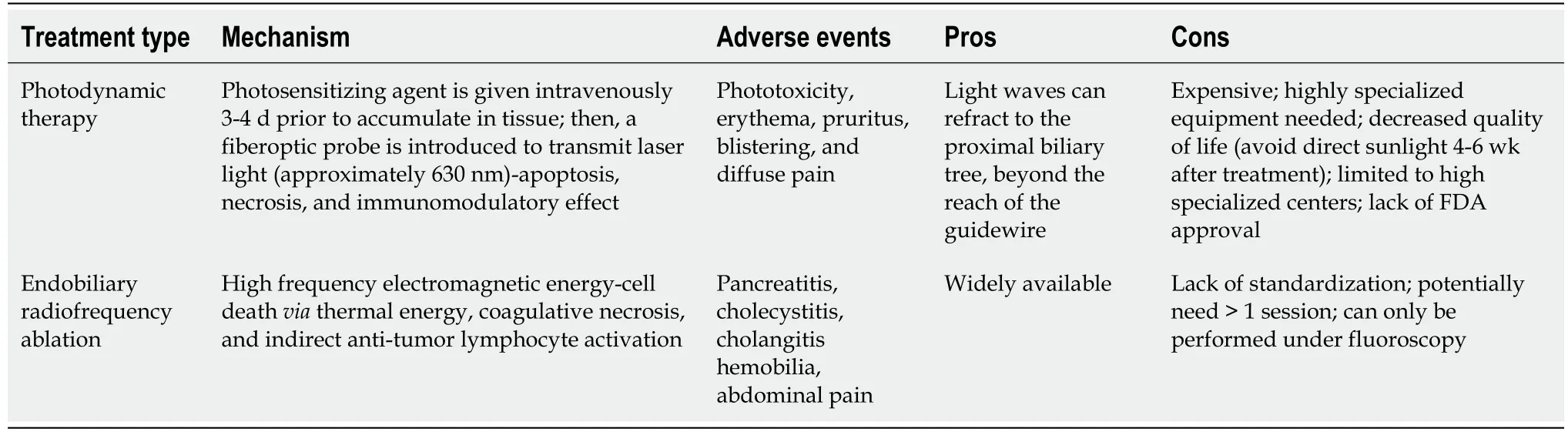
Table 3 Comparing Photodynamic therapy to endobiliary radiofrequency ablation
CONCLUSlON
In conclusion,the optimal palliation of malignant obstruction remains a challenging task for endoscopists and requires a dedicated team able to offer a variety of intervention based on patient presentation,symptoms and expected survival.
FOOTNOTES
Author contributions:Canakis A was responsible of drafting and reference editing;Kahaleh M was responsible for concept,final drafting,and final approval of manuscript.
Conflict-of-interest statement:Dr.Kahaleh is a consultant for Boston Scientific,Medtronic and Abvvie,he has received research grant from Boston Scientific,Apollo,Olympus,Cook,Microtech and Fuji;Dr Canakis has no disclose.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United States
ORClD number:Michel Kahaleh 0000-0003-0836-6114.
Corresponding Author's Membership in Professional Societies:American Gastroenterological Association,No.276889;and American Society for Gastrointestinal Endoscopy,No.90809.
S-Editor:Chen YL
L-Editor:A
P-Editor:Chen YL
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Gastric intestinal metaplasia development in African American predominant United States population
- Water-jet vs traditional triangular tip knife in peroral endoscopic myotomy for esophageal dysmotility:A systemic review and metaanalysis
- Laparoscopic Janeway gastrostomy as preferred enteral access in specific patient populations:A systematic review and case series
- Tracheoesophageal fistulas in coronavirus disease 2019 pandemic:A case report
- Hemostasis of massive bleeding from esophageal tumor:A case report
- Cronkhite-Canada syndrome:First case report from Egypt and North Africa
