Cronkhite-Canada syndrome:First case report from Egypt and North Africa
2022-10-25AhmedElsayedAlzamzamyAshrafAboubakrHusseinOkashaAbeerAbdellatefShaimaaElkholyMahmouddWahbaMohamedAlboraieHusseinElsayedMohamedOthman
Ahmed Elsayed Alzamzamy,Ashraf Aboubakr,Hussein H Okasha,Abeer Abdellatef,Shaimaa Elkholy,Mahmoudd Wahba,Mohamed Alboraie,Hussein Elsayed,Mohamed O Othman
Ahmed Elsayed Alzamzamy,Ashraf Aboubakr,Department of Gastroenterology and Hepatology,Maadi Armed Forces Medical Complex,Military Medical Academy,Cairo 11711,Egypt
Hussein H Okasha,Abeer Abdellatef,Shaimaa Elkholy,Mahmoudd Wahba,Department of Internal Medicine,Division of Gastroenterology,Hepatology and Endoscopy,Cairo University,Cairo 11311,Egypt
Mohamed Alboraie,Department of Internal Medicine,Al-Azhar University,Cairo 11311,Egypt Hussein Elsayed,Department of Pathology,Military Medical Academy,Cairo 11711,Egypt
Mohamed O Othman,Department of Internal Medicine,Baylor College of Medicine,Houston,TX 77082,United States
Abstract BACKGROUND Gastrointestinal (GI) polyposis is a rare condition in GI diseases.To date about 500 cases of Cronkhite-Canada syndrome (CCS) have been reported worldwide.CASE SUMMARY We report a 60-year-old female patient who presented with dyspepsia,abdominal pain,and weight loss of 1-year duration.Her physical examination showed alopecia and onychodystrophy.Upper endoscopy revealed diffuse markedly thickened gastric mucosa involving the whole stomach with thickened gastric rugae and numerous polypoidal lesions.Histopathological examination showed marked hyperplasia of the foveolar glands with inflammatory cell infiltration.Endoscopic ultrasound showed a significantly hypertrophic mucosa and muscularis mucosa,while the submucosa and the muscularis propria were spared,favouring its benign nature.Colonoscopy showed multiple sessile polyps scattered at different parts of the colon.Histopathological examination revealed tubular adenomatous polyps with low-grade dysplasia.Differential diagnoses included CCS,Menterier disease (MD),other polyposis syndromes,lymphoma,amyloidosis,and gastric malignancies.The presence of alopecia,nail dystrophy,GI polyposis,markedly thickened gastric mucosa and folds,abdominal pain,weight loss,and marked foveolar gland hyperplasia;all was in favour of CCS.Lymphoma was excluded due to sparing of the muscularis propria.The presence of colonic polyps and antral and duodenal infiltration,and the absence of hypoproteinaemia decreased the possibility for MD.CONCLUSION The patient was diagnosed as having CCS.
Key Words: Gastrointestinal polyposis;Thickened gastric mucosa;Cronkhite-Canada syndrome;Case report
lNTRODUCTlON
Cronkhite-Canada syndrome (CCS) is one of the rarest nonhereditary diseases[1],and its exact aetiology is still unknown[2],with around 500 cases having been described in the literature[3].Most of CCS cases were reported from Japan,and to our knowledge,our case is the first case reported from Egypt and North Africa.
Patient with CCS usually presents with gastrointestinal (GI) symptoms such as abdominal pain,weight loss,and diarrhea,or with other symptoms such as onychodystrophy,alopecia,hyperpigmentation of the skin,and rarely vitiligo[4].GI polyposis is the main endoscopic feature in CCS,which is commonly non-neoplastic and rather inflammatory,hyperplastic,hamartomatous,and/or adenomatous polyps in nature[5].Moreover,some CCS cases may develop gastric and colorectal malignancies during the disease course[4].
CASE PRESENTATlON
Chief complaints
A 60-year-old female patient presented with dyspepsia,abdominal pain,and weight loss of 1-year duration.
History of present illness
The patient denied other GI or anaemic symptoms.She was a non-smoker and did not drink alcohol.
History of past illness
The patient’s past medical history was free apart from prolonged proton-pump inhibitor (PPI) intake.
Personal and family history
There was no family history of gastrointestinal polyposis or colorectal malignancy.
Physical examination
The physical examination was unremarkable apart from alopecia (Figure 1A) and onychodystrophy (Figure 1B).
Laboratory examinations
The patient’s laboratory profile was within normal limits including a full complete blood picture (CBC),chemistry,serum albumin,serum calcium,urine analysis,antinuclear antibody (ANA),and IgG-4.
Imaging examinations
Oesophago-gastro-duodenoscopy (OGD) revealed diffuse markedly thickened gastric mucosa involving the whole stomach (fundus,body,and antrum),with thickened and tortuous gastric rugae,and numerous polypoidal lesions (3-10 mm in diameter),with a hyperaemic mucosa,and to a lesser extent down to the duodenal bulb and second part of the duodenum (Figure 2A and B).Multiple conventional biopsies were taken,and polypectomy was done for the large polyps for histopathological examination.Biopsies showed marked hyperplasia and cystic dilation of foveolar glands with inflammatory cell infiltration including eosinophils,hyperplastic polyps,chronic gastritis,andHelicobacter pylori(H.pylori) infection with no atypia or malignancy (Figure 3).IgG4-immunohistochemistry showed a very faintly positive signal.
Endoscopic ultrasound was done later and showed a significantly hypertrophic mucosa and muscularis mucosa,while the submucosa and the muscularis propria were spared,favouring its benign nature.Wall thickness was up to 8-10 mm (normal wall thickness is up to 4 mm) (Figure 2C).
Colonoscopy showed multiple variable-sized,sessile,and pedunculated polyps (~15),scattered at different parts of the colon.Snaring of the large polyps was done after submucosal injection (Figure 2D and E),and histopathological examination showed typical features of benign juvenile-like and hamartomatous polyps without dysplastic changes,while pathology of other polyps revealed tubular adenomatous polyps with low-grade dysplasia.

Figure 1 Physical examination.
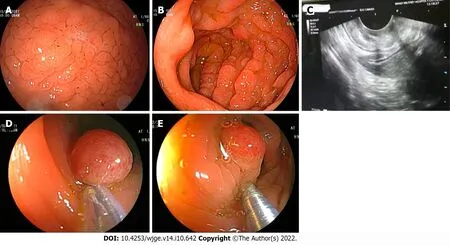
Figure 2 Endoscopy.
Both push enteroscopy and terminal ileoscopy showed no polyposis with a normal mucosa in the 3rdand 4thportions of the duodenum,the proximal jejunum,and the terminal ileum.
Computerized tomography (CT) scan of the abdomen &pelvis with oral and intravenous (IV) contrast revealed mild circumferential mural thickening of the gastric wall.
FlNAL DlAGNOSlS
The patient was diagnosed as having CCS.
TREATMENT
The patient started a sequential therapy forH.pyloriinfection with complete eradication,followed by a proton pump inhibitor (40 mg once daily),prednisolone (30 mg/d),and mesalazine (500 mg QID) for 6 mo.
DlSCUSSlON
In our case,the following differential diagnoses were raised and discussed with our gastroenterologists: CCS,MD,other polyposis syndromes (such as familiar adenomatous polyposis,Gardner syndrome,juvenile polyposis,Peutz-Jeghers syndrome,and Turcot syndrome),lymphoma,amyloidosis,duodenal gastric heterotopia,and gastric malignancies.
The final diagnosis was based on the medical history,physical examination,endoscopic findings,and the histopathological examination.The presence of anomalies of ectodermal tissues (such as alopecia and nail dystrophy),gastrointestinal polyposis (hamartomatous and adenomatous polyps),markedly thickened gastric mucosa and folds,abdominal pain,weight loss,and marked foveolar gland hyperplasia;all was in favour of the CCS.On the other hand,there was no protein-losing enteropathy,diarrhea,hypoalbuminaemia,or skin pigmentation.
Lymphoma was excluded due to sparing of the muscularis propria.Furthermore,markedly thickened gastric mucosa and folds and the histopathological examination which revealed marked foveolar gland hyperplasia were consistent with MD.In addition,abdominal pain and weight loss are common presentation of MD,but the presence of colonic polyps,and antral and duodenal infiltration,and the absence of hypoproteinaemia decreased the possibility for MD.
The patient started a sequential therapy forH.pyloriinfection with complete eradication,followed by a proton pump inhibitor (40 mg once daily),prednisolone (30 mg/d),and mesalazine (500 mg QID) for 6 mo.
Common complications of CCS include anemia,intussusception,rectal prolapse,and GI bleeding,as well as other less common ones such as recurrent severe acute pancreatitis,myelodysplastic syndrome,cecal intussusception,portal thrombosis,membranous glomerulonephritis,and osteoporotic fractures that may result from malabsorption of calcium or prolonged glucocorticoid therapy or both.The most serious complication is malignancy;however,the incidence of CCS-related cancer is estimated to be 5%-25%,especially gastric and colon cancer[6].
The follow-up endoscopies (OGD and colonoscopy) after 6 and 12 mo of treatment showed significant remission with a reduced number of gastric and colonic polyps and regression of hypertrophic gastric folds (Figure 4).Consequently,the patient's clinical condition was markedly improved,and the prednisolone dose was reduced gradually to 7.5 mg/d,but the mesalazine dose remained the same.
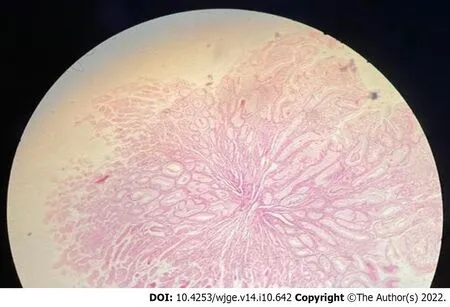
Figure 3 Histopathological examination showed marked hyperplasia and cystic dilation of foveolar glands with inflammatory cell infiltration including eosinophils,chronic gastritis,and Helicobacter pylori infection with no atypia or malignancy.
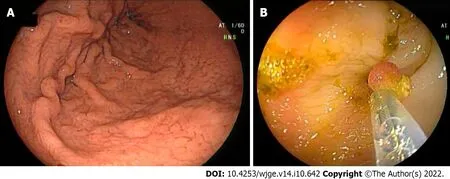
Figure 4 Follow-up endoscopies after 6 mo and 12 mo of treatment showed significant remission with a reduced number of gastric and colonic polyps and regression of hypertrophic gastric folds.
There is a tendency of malignant transformation or coexistence of gastrointestinal malignancies in patients with CCS.Therefore,endoscopic documentation of regression in CCS is important despite the lower incidence of CCS-related cancer in remission patients.Therefore,the comprehensive endoscopic annual surveillance eitherviachromoendoscopy or directed biopsy from irregular polyps,to exclude pre-cancer lesions before development of invasive carcinoma is mandatory;however,there are still no recommended guidelines to be followed[7].
Nutritional support,electrolytes,and mineral and vitamin supplementation remain the cornerstone in treatment of CCS beside antibiotics and corticosteroids;however,the definitive treatment is still unknown[4,7].
Till now,there is still much that needs to know about this syndrome.In this context,the most important issue is to maintain treatment monitoring and provide appropriate measure to prevent relapse[8].
CONCLUSlON
CCS is a form of uncommon,acquired polyposis with obscure aetiology.To date around 500 cases have been reported all over the world.Most of CCS cases were reported from Japan,and to our knowledge,our case is the first case reported from Egypt and North Africa.CCS is generally characterized by GI symptoms,such as diarrhea and skin changes (e.g.,alopecia,skin pigmentation,and onychodystrophy),while GI polyposis is the main endoscopic feature in CCS,which is commonly non-neoplastic and mainly include inflammatory,hyperplastic,hamartomatous,and/or adenomatous polyps.CCS has a malignant potential,and some cases may develop gastric and colorectal malignancies during the disease course.Till now,there is no uniform standard treatment for CCS.
ACKNOWLEDGEMENTS
We would like to acknowledge our hospitals and their workers,nurses,and staff members for all the support and help in this study and throughout our careers.
FOOTNOTES
Author contributions:Alzamzamy A contributed to data acquisition,analysis,and interpretation,all endoscopies,and drafting of the manuscript;Aboubakr A,Okasha H,and Othman M edited the manuscript and supervised the research;Alzamzamy A and Abdelatif A wrote the manuscript;Elsayed H contributed to the histopathology work and result analysis;Elkholy S,Wahba M,and Alboraie M contributed to data acquisition,analysis,and interpretation;all authors approved the final version of the manuscript.
lnformed consent statement:Informed written consent was obtained from the patients for the publication of this report and any accompanying images.
Conflict-of-interest statement:The authors declare that they have no conflict of interest.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016),and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Egypt
ORClD number:Ahmed Elsayed Alzamzamy 0000-0002-3817-5370;Ashraf Aboubakr 0000-0002-3453-9317;Hussein H Okasha 0000-0002-0815-1394;Abeer Abdellatef 0000-0001-9945-9767;Shaimaa Elkholy 0000-0003-4322-6467;Mohamed O Othman 0000-0002-5888-4334.
Corresponding Author's Membership in Professional Societies:American Society for Gastrointestinal Endoscopy.
S-Editor:Chen YL
L-Editor:Wang TQ
P-Editor:Chen YL
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Endoscopic palliation of malignant biliary obstruction
- Gastric intestinal metaplasia development in African American predominant United States population
- Water-jet vs traditional triangular tip knife in peroral endoscopic myotomy for esophageal dysmotility:A systemic review and metaanalysis
- Laparoscopic Janeway gastrostomy as preferred enteral access in specific patient populations:A systematic review and case series
- Tracheoesophageal fistulas in coronavirus disease 2019 pandemic:A case report
- Hemostasis of massive bleeding from esophageal tumor:A case report
