无创高频振荡通气在早产儿呼吸支持中有效性及安全性的meta分析
2022-04-28奚伟健沈玲飞张志群
奚伟健 沈玲飞 张志群



[摘要] 目的 系統评价无创高频振荡通气用于早产儿的有效性及安全性。方法 计算机检索Cochrane、CNKI、PubMed、Embase、维普、万方等数据库中自数据库建立至2020年1月所有无创高频振荡通气和经鼻持续正压通气作为早产儿呼吸支持方式的随机对照试验,按照纳入和排除标准筛选文献、提取资料,并依据 Cochrane Handbook 的质量评价标准评价纳入研究质量后,用 RevMan5.3软件进行 meta 分析。结果 共纳入11个随机对照试验,合计927例患者。无创高频振荡通气与经鼻持续正压通气组相比较,无创通气失败率较低[RR=0.39,95%CI:(0.29,0.51),P=0.000],支气管肺发育不良发生率更低[RR=0.55,95%CI:(0.38,0.79)P=0.001],两组患儿坏死性小肠结肠炎、颅内出血、动脉导管未闭、早产儿视网膜病等并发症的发生率差异无统计学意义(P>0.05),CO2 清除效果更佳[WMD=-3.33,95%CI:(-6.23,-0.43)P=0.020]。结论 无创高频振荡通气对比经鼻持续正压通气可显著降低无创通气失败率,减少支气管肺发育不良发生率,并无加重或减少坏死性小肠结肠炎、颅内出血、动脉导管未闭、早产儿视网膜病等相关并发症风险,有效清除CO2。
[关键词] 无创高频振荡通气;经鼻持续正压通气;早产儿;支气管肺发育不良
[中图分类号] R722.1 [文献标识码] B [文章编号] 1673-9701(2022)09-0055-04
Meta-analysis of the efficacy and safety of noninvasive high-frequency oscillatory ventilation in respiratory support of premature infants
XI Weijian1 SHEN Lingfei1 ZHANG Zhiqun1,2
1.The Fourth Clinical Medical College, Zhejiang Chinese Medical University, Hangzhou 310053, China; 2.Department of Neonatology, Hangzhou First People's Hospital, Hangzhou 310003, China
[Abstract] Objective To systematically evaluate the efficacy and safety of noninvasive high-frequency oscillatory ventilation in premature infants. Methods Randomized controlled trials of all noninvasive high-frequency oscillatory ventilation and nasal continuous positive pressure ventilation as respiratory support for premature infants from database establishment to January 2020 in Cochrane, CNKI, PubMed, Embase, VIP, Wanfang databases were searched by computer. According to inclusion and exclusion criteria, literature was screened, data were extracted, and the quality of the included studies was evaluated according to the quality evaluation criteria of the Cochrane Handbook. meta-analysis was performed using RevMan5.3 software. Results A total of 11 randomized controlled trials with a total of 927 patients were included. Compared with the nasal continuous positive airway pressure ventilation group, the noninvasive high-frequency oscillatory ventilation group had lower ventilation failure rate [RR=0.39, 95% CI:(0.29, 0.51), P= 0.000], lower incidence rate of bronchopulmonary dysplasia [RR=0.55, 95% CI:(0.38, 0.79), P=0.001], and better CO2 removal effect [WMD=-3.33, 95% CI: (-6.23, -0.43), P=0.020]. There was no statistical difference in the incidence rate of complications such as necrotizing enterocolitis, intracranial hemorrhage, patent ductus arteriosus, and retinopathy of prematurity between the two groups. Conclusion Compared with nasal continuous positive airway pressure ventilation, noninvasive high-frequency oscillatory ventilation can significantly reduce the failure rate of noninvasive ventilation, reduce the incidence of bronchopulmonary dysplasia, and effectively remove CO2, without aggravating or reducing the risk of necrotizing enterocolitis, intracranial hemorrhage, patent ductus arteriosus, retinopathy of prematurity and other related complications.
[Key words] Noninvasive high-frequency oscillatory ventilation; Nasal continuous positive airway pressure; Premature infants; Bronchopulmonary dysplasia
早产儿最常见的疾病之一是新生儿呼吸窘迫综合征[1]。产前激素可以有效降低新生儿呼吸窘迫综合征的发生率[2]。有创通气常作为呼吸支持手段但易致支气管肺发育不良(bronchopulmonarydysplasia,BPD)等相关并发症风险上升[3]。无创高频振荡通气(noninvasive high frequency oscillatory ventilation,NHFOV),具有高通气频率、低潮气量、稳定的气道压等优点[4]。最近发表的一篇NHFOV的meta分析[5]有效评估了其CO2清除率及插管风险,但受限于纳入文献数量过少及样本量未对BPD等远期指标进行分析。国外最新发表了2项样本量较大的随机对照试验[6,7],为进一步验证NHFOV在早产儿呼吸支持中的疗效及安全性,本文收集了国内外发表的有关NHFOV的随机对照试验进行meta分析,现报道如下。
1资料与方法
1.1 一般资料
1.1.1检索策略 分别在中国学术期刊全文数据库(CNKI)、万方数据库、V.I.P、PubMed、Embase、Cochrane 等数据库,检索数据库建立至2020年1月有关无创高频振荡通气(NHFOV)和经鼻持续正压通气(nasal continuous positive pressure ventilation,NCPAP)作为早产儿呼吸支持方式的随机对照试验。
1.1.2文献纳入标准 ①研究类型为随机对照试验;②研究对象为早产儿,随机使用NHFOV或NCPAP治疗;③报告了以下结局指标中的一个以上:主要结局指标:无创通气失败率、BPD发生率;次要结局指标:CO2水平;坏死性小肠结肠炎(necrotizing enterocolitis ,NEC)、颅内出血(intraventricular hemorrhage,IVH)、动脉导管未闭(patent ductus arteriosus,PDA)、早产儿视网膜病(retinopathy of prematurity,ROP)发生率。
1.1.3文献排除标准 ①非随机对照试验;②无法提取数据的文献;③重复发表的文献。
1.2研究方法
1.2.1资料提取 由2位评价者各自独立阅读符合入选条件的研究文献,独立摘录每一项研究的信息,同时对入选研究资料的设计、实施和分析过程进行再评价。有争议的文献通过第三位作者进行评定是否纳入。
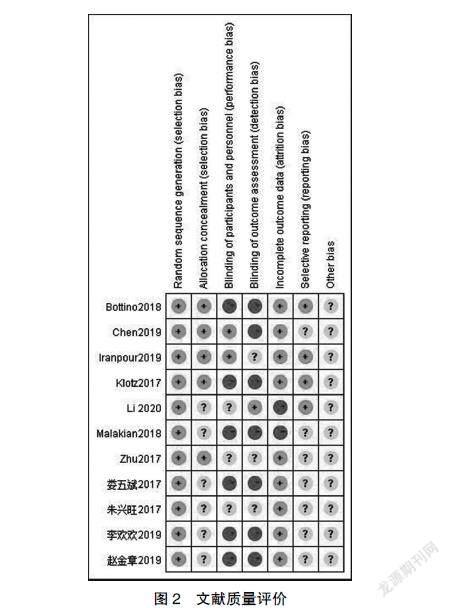
1.2.2文献质量评价 采用 Cochrane 评价手册 5.1.0 推荐的标准评价纳入研究的质量,评判先由2名经过严格循证医学学习人员独立评判,若出现分歧,则交由第3名经过严格循证医学学习的人员独立评判。
1.3观察指标
主要指标:无创通气失败率、BPD发生率;次要指标: IVH、ROP、NEC、PDA发生率;CO2水平。
1.4 统计学方法
由作者按meta分析要求独立提取整理入选文献,提取内容为文献的基本信息、研究类型、研究对象特征。由两名经过循证医学学习人员独立验证后,制作文献信息提取表。
2 结果
2.1文献检索基本情况
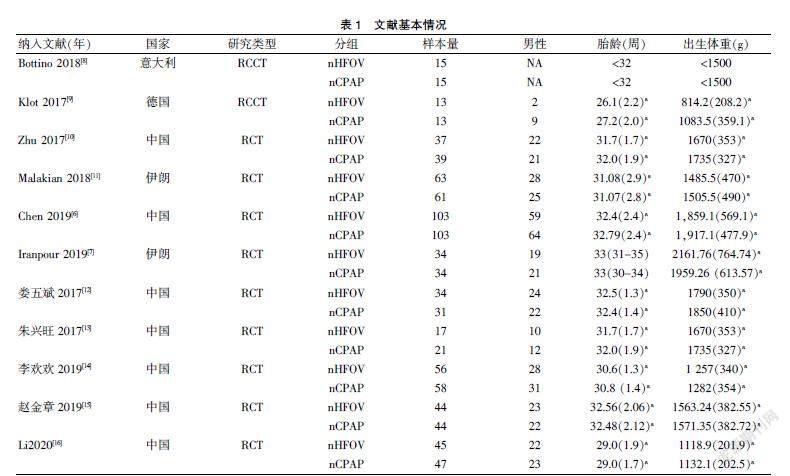
本研究的文献筛选流程见图1,纳入文献的质量评价见图2,文献的基本情况具体见表1,最后纳入11篇随机对照试验研究[6-16]。采用Stata12.1软件检测无创通气失败率、BPD发生率的发表偏倚,P>0.05,提示无明显发表偏倚。
RCT:随机对照试验;RRCT:随机对照交叉试验;PS(Pulmonary surfactant)肺表面活性物质NA;无法获取;a:mean(sd)
2.2 主要结局指标
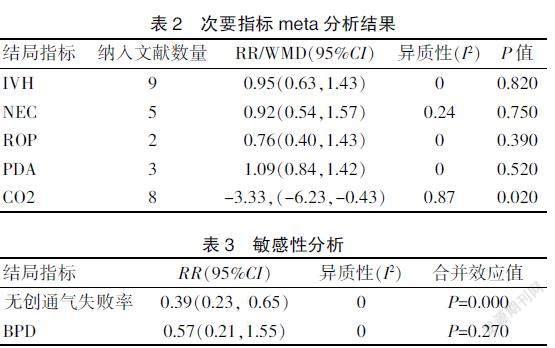
2.2.1无创通气失败率 纳入9篇文献,结果显示两组差异有统计学意义[RR=0.39,95%CI:(0.29,0.51),P=0.000]见图4;敏感性分析后P=0.000,证实了结果的可靠性见表3。
2.2.2支气管肺发育不良(BPD)发生率 纳入6篇文献,结果显示两组差异有统计学意义[RR=0.55,95%CI:(0.38,0.79),P=0.001],见图5;敏感性分析后P=0.270,见表3。
2.3次要结局指标
除CO2清除率差异有统计学意义[WMD=-3.33,95%CI:(-6.23,-0.43),P=0.020]外,其余次要结局指标,两组差异无統计学意义(P>0.05)。见表2。
3 讨论
本文同之前发表的meta分析[5]结果一致,证实NHFOV对比NCPAP可显著降低无创通气失败率,降低插管风险,行敏感性分析,P=0.000结果同前,证实了结果的可靠性。BPD是一类多遗传因素与环境因素相互作用的慢性肺疾病,在早产儿中尤为常见[17]。本文对结局指标包含BPD发生率的6篇文献进行meta分析,NHFOV组BPD发病率低于NCPAP组,两组差异有统计学意义(P=0.001),但敏感性分析后P=0.270,前后结果不一致,这可能是因为:①BPD 发病因素复杂,除有创机械通气外,感染、营养、氧毒性以及基因易感性也是重要病因[14];②敏感性分析仅纳入2项研究, 样本量偏小, 检验效能不足;③极早产儿(GA<28周)是BPD的高危人群[18],Gortner等[19]的研究报道GA<26周BPD发生率高56%,本文研究人群胎龄偏大。
自Vander等[4]的研究指出NHFOV能有效清除CO2,其后陸续有一些研究[20-21]的结论与Vander等一致,但多为回顾性研究,样本量小,缺乏足够的循证医学证据。本文较之前发表的有关NHFOV的meta分析[5]新纳入5项RCT,有效评估了BPD、IVH等远期并发症风险。
本文尚存在以下局限性:①纳入患儿胎龄偏大; ②缺乏高质量随机对照试验。③呼吸机参数设置、通气失败标准、疗效评估等存在差异。
本研究发现NHFOV对比NCPAP可显著降低无创通气失败率,减少BPD发生率,并无加重或减少IVH、NEC、PDA、ROP等相关并发症风险,有效清除CO2。该结论有待高质量大规模多中心随机对照试验验证。
[参考文献]
[1] Olaloko O, Mohammed R, Ojha U. Evaluating the use of corticosteroids in preventing and treating bronchopulmonary dysplasia in preterm neonates[J].Int J Gen Med, 2018, 11: 265-274.
[2] Sweet DG,Carnielli V,Greisen G,et al. European consensus guidelines on the management of respiratory distress syndrome-2019 update[J].Neonatology,2019,115(4): 432-450.
[3] Natarajan G,Pappas A,Shankaran S,et al. Outcomes of extremely low birth weig-ht infants with bronchopulmonary dysplasia: impact of the physiologic definition[J]. Early Hum Dev, 2012, 88(7): 509-515.
[4] Van der Hoeven M,Brouwer E,Blanco CE.Nasal high frequency ventilation in neonates with moderate respiratory insufficiency[J].Arch Dis Child Fetal Neonatal Ed, 1998, 79(1): F61-63.
[5] Li J, Li X, Huang X, et al. Noninvasive high-frequency oscillatory ventilation as respiratory support in preterm infants: a meta-analysis of randomized controlled trials[J]. Respir Res, 2019, 20(1): 58.
[6] Chen L, Wang L, Ma J, et al. Nasal high-frequency oscillatory ventilation in preterm infants with respiratory distress syndrome and ARDS after extubation: a randomized controlled trial[J].Chest,2019,155(4): 740-748.
[7] Iranpour R, Armanian AM, Abedi AR, et al. Nasal high-frequency oscillatory ventilation (nHFOV) versus nasal continuous positive airway pressure (NCPAP) as an initial therapy for respiratory distress syndrome (RDS) in preterm and near-term inf-ants[J].BMJ Paediatr Open, 2019,3(1): e000443.
[8] Bottino R,Pontiggia F,Ricci C,et al. Nasal high-frequency oscillatory ventilation and CO2 removal: A randomized controlled crossover trial[J].Pediatr Pulmonol, 2018, 53(9): 1245-1251.
[9] Klotz D,Schneider H,Schumann S,et al.Non-invasive high-frequency oscillatory ventilation in preterm infants: A randomised controlled cross-over trial[J].Arch Dis Child Fetal Neonatal Ed, 2018, 103(4): F1-F5.
[10] ZHU XW, Zhao JN, Tang SF, et al.Noninvasive high-frequency oscillatory ventilation versus nasal continuous positive airway pressure in preterm infants with moderate-severe respiratory distress syndrome: A preliminary report[J].Pediatr Pulmonol, 2017, 52(8):1038-1042.
[11] Malakian A, Bashirnezhadkhabaz S, Aramesh M-R, et al.Noninvasive high-frequency oscillatory ventilation versus nasal continuous positive airway pressure in preterm infants with respiratory distress syndrome: A randomized controlled trial[J].The Journal of Maternal-Fetal & Neonatal Medicine, 2020,33(15):2601-2607.
[12] 娄五斌,张卫星.经鼻无创高頻振荡通气和持续气道正压通气在早产儿呼吸窘迫综合征撤机后的应用比较[J].广东医学,2017,38(13):2037-2040.
[13] 朱兴旺,闫军,冉琴,等.无创高频振荡通气治疗新生儿呼吸窘迫综合征的初步研究[J].中华新生儿科杂志,2017, 32(4):291-294.
[14] 李欢欢,朱兴旺,汪万军.无创高频振荡通气在早产儿有创机械通气撤机后呼吸支持效果的随机对照研究[J].第三军医大学学报,2019,41(17):1688-1692.
[15] 赵金章,刘玲,张莉,等.无创高频振荡通气与经鼻持续气道正压通气在新生儿呼吸窘迫综合征初始治疗中的疗效评价[J].陕西医学杂志,2019,48(11):1461-1463,1467.
[16] Li Y,Wei Q,Zhao D,et al.Non-invasive high-frequency oscillatory ventilation in preterm infants after extubation: A randomized, controlled trial[J].J Int Med Res,2021,49(2): 300 060 520 984 915.
[17] Bhandari V.The potential of non-invasive ventilation to decrease BPD[J].Semin Perinatol,2013,37(2):108-114.
[18] Fischer HS, Rimensberger PC.Early noninvasive high-frequency oscillatory ventilation in the primary treatment of respiratory distress syndrome[J].Pediatric Pulmonology, 2018, 53(2): 126-127.
[19] Gortner L,Misselwitz B,Milligan D,et al.Rates of bronchopulmonary dysplasia in very preterm neonates in Europe: Results from the MOSAIC cohort[J].Neonatology, 2011, 99(2): 112-117.
[20] Mukerji A, Singh B, Helou SE, et al.Use of noninvasive high-frequency ventilation in the neonatal intensive care unit: A retrospective review[J].Am J Perinatol, 2015, 30(2): 171-176.
[21] Ali YAH, Seshia MM, Ali E, et al.Noninvasive high-frequency oscillatory ventilation: A retrospective chart review[J].Am J Perinatol, 2020,11(2):23.
(收稿日期:2021-09-11)
