Pancreas sparing duodenectomy in the treatment of primary duodenal neoplasms and other situations with duodenal involvement
2021-11-08JuliBusquetsJosefinLopezDominguezAnGonzlezCstilloMrinVil
Juli Busquets ,, Josefin Lopez-Dominguez ,An Gonzlez-Cstillo ,Mrin Vil ,
Nuria Pelaez a,Lluis Secanella a,Emilio Ramos a,Juan Fabregat a
a Department of Hepatobiliary and Pancreatic Surgery, Hospital Universitari de Bellvitge, Research Group of Hepato-biliary and Pancreatic Diseases, Institut d’InvestigacióBiomèdica de Bellvitge - IDIBELL, Barcelona University, L’Hospitalet de Llobregat, Barcelona 08907, Spain
b Department of General Surgery, Hos pital del Mar, Barcelona 08907, Spain
c Department of General Surgery, Hospita l de Mataró, Barcelona 08907, Spain
Keywords: Duodenectomy Duodenal neoplasms Organ sparing treatments Pancreatic surgery Duodenal diseases
ABSTRACT Background: There are no clearly defined indications for pancreas-preserving duodenectomy. The present study aimed to analyze postoperative morbidity and the outcomes of patients undergoing pancreas-preserving duodenectomy. Methods: Patients undergoing pancreas-preserving duodenectomy from April 2008 to May 2020 were included. We divided the series according to indication: scenario 1, primary duodenal tumors; scenario 2, tumors of another origin with duodenal involvement; and scenario 3, emergency duodenectomy. Results: We included 35 patients. Total duodenectomy was performed in 1 patient of adenomatous duo-denal polyposis, limited duodenectomy in 7, and third + fourth duodenal portion resection in 27. The indications for scenario 1 were gastrointestinal stromal tumor ( n = 13), adenocarcinoma ( n = 4), neu-roendocrine tumor ( n = 3), duodenal adenoma ( n = 1), and adenomatous duodenal polyposis ( n = 1); scenario 2: retroperitoneal desmoid tumor ( n = 2), recurrence of liposarcoma ( n = 2), retroperitoneal paraganglioma ( n = 1), neuroendocrine tumor in pancreatic uncinate process ( n = 1), and duodenal in-filtration due to metastatic adenopathies of a germinal tumor with digestive hemorrhage ( n = 1); and scenario 3: aortoenteric fistula ( n = 3), duodenal trauma ( n = 1), erosive duodenitis ( n = 1), and bil-iopancreatic limb ischemia ( n = 1). Severe complications (Clavien-Dindo ≥IIIb) developed in 14% (5/35), and postoperative mortality was 3% (1/35). Conclusions: Pancreas-preserving duodenectomy is useful in the management of primary duodenal tu-mors, and is a technical option for some tumors with duodenal infiltration or in emergency interventions.
Introduction
Pancreaticoduodenectomy (PD) is the technique of choice in the surgical treatment of malignant periampullary tumors and in-flammatory disease of the head of the pancreas. The morbidity of this technique is not negligible and may present medium-and long-term sequelae. Different pancreas-preserving techniques such as duodenal-preserving pancreatectomy, ampullectomy or uncinec-tomy have been proposed for the treatment of benign pancreatic tumors or those of low malignancy potential [1–3] . Likewise, dif-ferent options of duodenectomy without removal of the pancreas have been described [ 1,4 ]. However, the indications of pancreas-preserving duodenectomy have not been clearly established. More-over, there are few studies in this regard, making it difficult to decide which technique is the most adequate in patients with non-infiltrating duodenal lesions and what technique is to be per-formed in emergency cases of irreversible duodenal pathology. Therefore, the aim of this study was to analyze the results of a retrospective series of pancreas-preserving duodenectomy.
Methods
We prospectively collected demographic, surgical and anato-mopathologic data as well as data related to postoperative mor-bidity, mortality and long-term follow-up of patients undergoing pancreas-preserving duodenectomy performed in our center from April 2008 to May 2020. This study was approved by the Clini-cal Research Ethics Committee of Hospital Universitari de Bellvitge (PR260/19).
Indication and preoperative study
The indications of pancreas-preserving duodenectomy were grouped into three scenarios for better comprehension and anal-ysis. Scenario 1 included primary tumors of the third and fourth duodenal portion, without pancreatic extension. These lesions were studied using computed tomography (CT) and upper fibrogas-troscopy with biopsy. Scenario 2 included extraduodenal tumors with duodenal infiltration by proximity. In these patients the study was based on CT, and upper fibrogastroscopy was optional. Sce-nario 3 included patients undergoing emergency duodenectomy due to isolated duodenal trauma or aortoenteric fistula ( Fig. 1 ) with pancreas-preserving duodenectomy being performed as an in-traoperative alternative. The preoperative study was based on CT results. Magnetic resonance cholangiopancreatography was used for the anatomical study of the periampullary area of the patients in scenarios 1 and 2 in order to determine the exact location of the biliopancreatic junction in relation to the tumor and for surgi-cal planning.
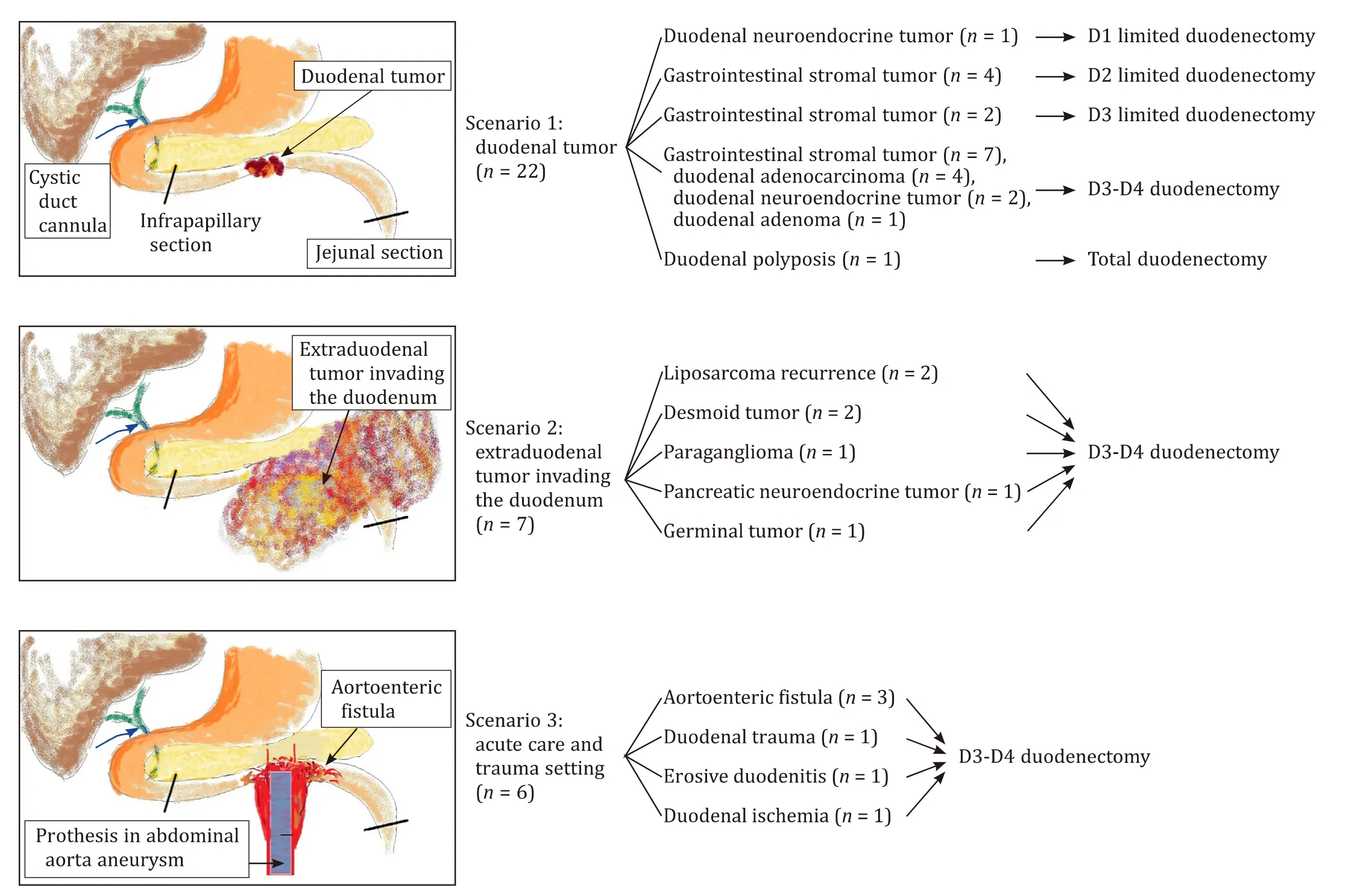
Fig. 1. The flow diagram of pancreas-preserving duodenectomy in three scenarios.
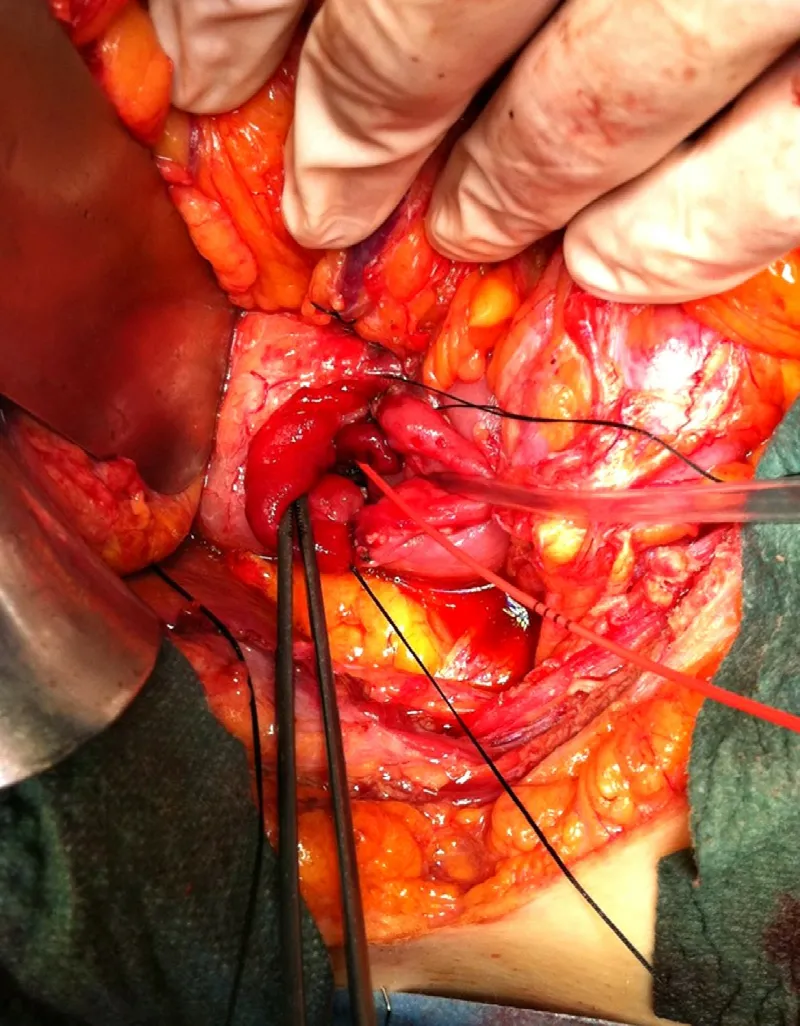
Fig. 2. Duodenal section preserving the papilla. The papilla is localized by palpating the cystic duct probe. The duodenal section begins on the free side of the duode-num, ending at the pancreatic duodenal side. To safely perform duodenal section the cutting line should be at least one centimetre distal to the papilla.
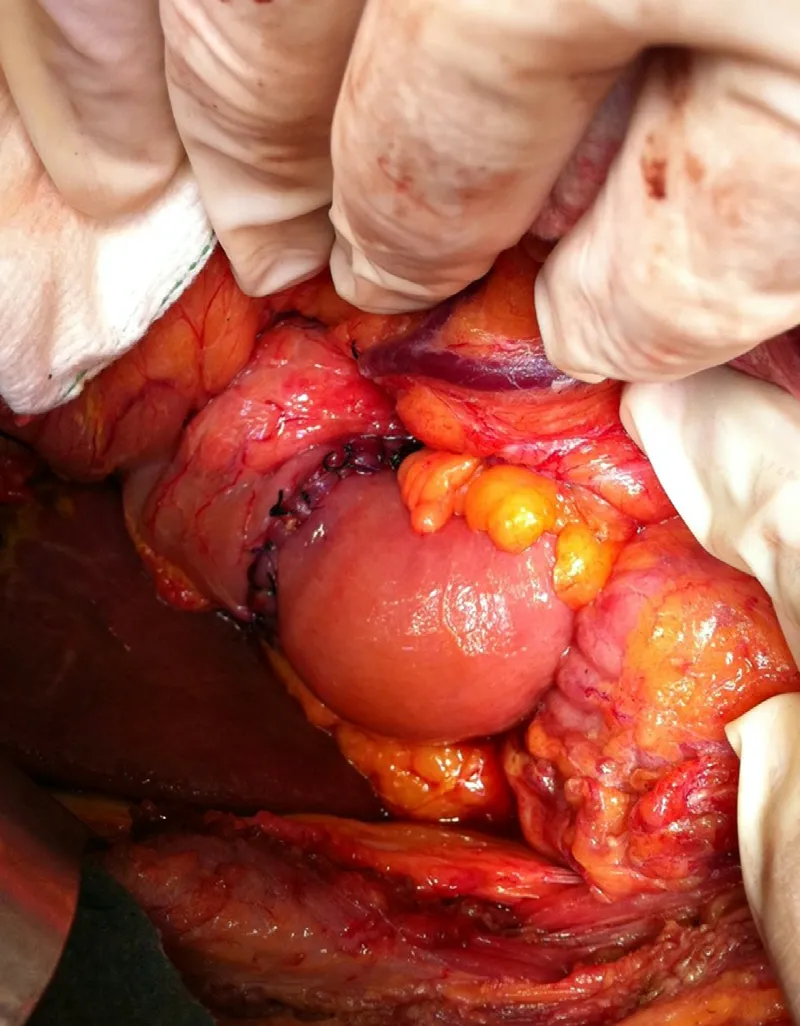
Fig. 3. Duodenojejunal anastomosis with interrupted sutures.
Surgical technique
A right subcostal incision was made followed by cholecystec-tomy and a wide Kocher maneuver, placing a cannula in the cystic duct (Taut cholangiogram catheter, Teleflex, Morrisville, NC, USA) and continuing to the duodenum ( Fig. 2 ). This step is crucial to safely perform duodenectomy. For correct cannulation of the nar-row cystic duct, we used a fine tip dissector or the Watson -Cheyne dissector (Aesculap Surgical Instruments, Tuttlinguen, Germany). Then, the duct was cannulated with a laparoscopic intraoperative cholangiography cannula or a Nelaton probe (Pennine, Derby, UK), as described previously [5] . The duodenal papilla was localized by palpating the probe to evaluate any possible association between the tumor and the papilla. After ruling out tumor involvement of the papilla, the jejunum was sectioned at the level of the Tre-itz angle and the duodenum uncrossed. During emergency proce-dures, this step facilitated localization of the duodenal papilla and avoided papillary avulsion. Thereafter, we performed infrapapillary duodenectomy and completed the resection of the third duode-nal portion while continuously controlling the localization of the papilla. Finally, end-to-end duodenojejunal anastomosis was made passing the transmesocolic jejunal loop ( Fig. 3 ) and non aspirative drainage was placed close to the suture. In small lesions, wedge resection with primary closure was performed. Whenever possible, all surgical procedures attempted to achieve R0 resection. Frozen slices of incisal margin and surgical specimen were routinely col-lected during surgery. Total duodenectomy was carried out in cases of adenomatous duodenal polyposis [ 3,4 ].
Statistical analysis
Demographic, surgical and pathological data, as well as those related to postoperative morbidity, mortality and long-term follow-up were collected from a prospective database. Categorical vari-ables are reported as proportion and normally distributed continu-ous variables as mean with standard deviation; non-normally dis-tributed variables are reported as median with range. SPSS18.0®statistical package (IBM, Chicago, IL, USA) was used for the analy-ses.
Results
From April 2008 to May 2020, 35 patients (21 men and 14 women) with a mean age of 59 years old underwent pancreas-preserving duodenectomy. Scenario 1 included 22 patients: 13 had a mesenchymal tumor (gastrointestinal stromal tumor, GIST), 4 duodenal adenocarcinoma, 3 duodenal neuroendocrine tumor, 1 duodenal adenoma, and 1 presented adenomatous duodenal poly-posis. Scenario 2 included 7 patients: 2 cases of recurrence of retroperitoneal liposarcoma, 2 retroperitoneal desmoid tumor, 1 duodenal infiltration by metastatic adenopathies of a germinal tu-mor, 1 retroperitoneal paraganglioma, and 1 neuroendocrine tumor in the pancreatic uncinate process. Six cases were included in sce-nario 3: 3 aortoenteric fistula in patients with an aortic prosthesis presenting digestive hemorrhage and hypovolemic shock, 1 duode-nal ischemia of the biliopancreatic limb in a patient with a previ-ous gastric by-pass, 1 abdominal trauma with duodenal lesion, and 1 of erosive duodenitis. The last patient presented digestive bleed-ing and hemodynamic instability secondary to erosive duodenitis and was undergoing chemotherapy for lymphoma.
The surgical technique involved pancreas-preserving duodenec-tomy (third and fourth duodenal portion with end-to-end duode-nojejunal anastomosis) in 27 patients, partial resection in 7, and total duodenectomy in 1. It is of note that the surgical technique in scenarios 2 and 3 was all duodenectomy of the third and fourth duodenal portion ( Fig. 1 ).
Seven patients underwent some type of additional resection. For example, during the resection of a well differentiated neuroen-docrine tumor of the uncinate process with infiltration of the third duodenal portion in case No. 15, we also performed duodenectomy of the third and fourth duodenal portion, resection of the upper mesenteric artery and reconstruction with a saphenous vein graft and uncinectomy ( Table 1,Fig. 4 ).

Fig. 4. A 67-year-old patient with neuroendocrine tumor of the uncinate pancreas. Uncinate pancreas tumor involved the superior mesenteric artery. A and B : Computed tomography: coronal view ( A ) and axial view (B ). C: A limited pancreatic resection and a duodenectomy were achieved, avoiding the need for pancreaticoduodenectomy; D: saphenous vein bypass was performed after resection. Tumor recurrence was diagnosed 5 years after resection. The patient remains alive 5 years and 8 months after the intervention. SMA: superior mesenteric artery; SMV: superior mesenteric vein; PUNC: pancreas uncinate; TM: tumor; JBSMA: jejunal branches of superior mesenteric artery; SMA-SF: superior mesenteric artery with a saphenous vein bypass.
Postoperative complications were observed in 54% of the pa-tients (19/35), 5 (14%) of which were Clavien-Dindo IIIb or greater. Three patients were reintervened: 1 for evisceration, 1 for hemoperitoneum and 1 for anastomotic dehiscence. The post-operative mortality was 3% (1/35), and the median postoperative hospital stay were 14 days (range 6–70), respectively. The only death was not directly related to surgery, but rather due to en-cephalopathy because of hyperammonemia which required admis-sion to intensive care because of respiratory insufficiency, followed by death 41 days after surgery with no intraabdominal complica-tions ( Table 1 ).
The anatomy pathology of the primary duodenal tumors (sce-nario 1) showed 13 cases of GIST, 4 duodenal adenocarcinomas, 1 adenomatous duodenal polyposis, 1 duodenal adenoma withinsitucarcinoma, and 3 duodenal neuroendocrine tumors. The study of the patients with GIST showed lesions with low-grade malignancy in 9, high-grade malignancy in 3 and no data related to aggressive-ness in 1. At the last follow-up, 30 patients remained alive and 5 had died. Seven cases of recurrence were reported during follow-up, including 4 undergoing surgery for GIST, 1 presenting a malig-nant retroperitoneal paraganglioma, and 2 undergoing surgery for 4th and 2nd relapse of liposarcoma, respectively ( Table 2 ).

Table 1 The surgical technique and postoperative morbidity.
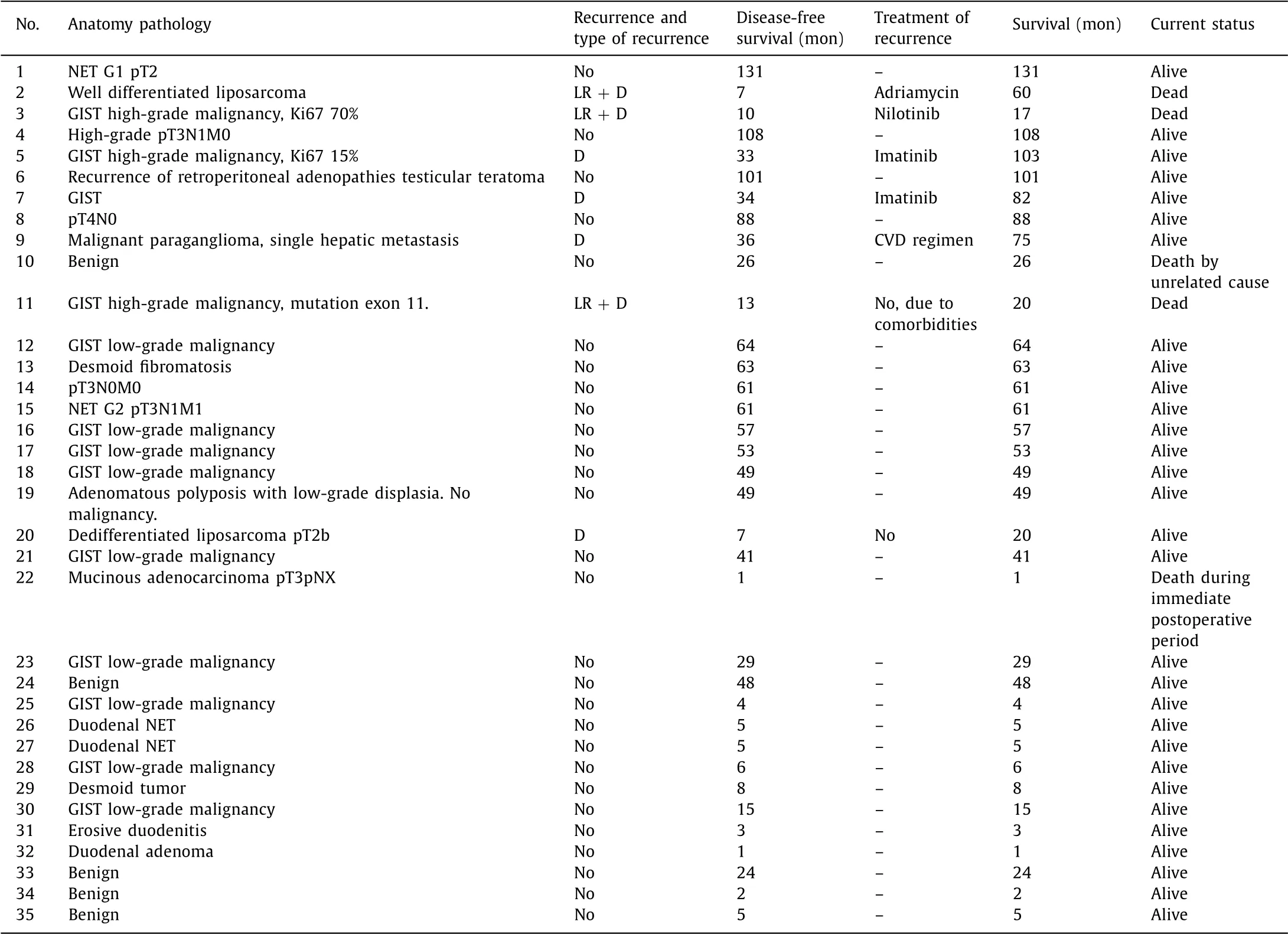
Table 2 Anatomy pathology and long-term evolution.
Discussion
The high morbidity presented by patients following PD has led to the search for strategies aimed at minimizing the use of this procedure. Duodenectomy is performed with the aim of re-secting the duodenum and avoiding extirpation of the head of the pancreas taking into account the inherent morbidity this im-plies [ 1,6,7 ]. Sauvanet et al. [8] stated that “pancreatic surgery should not be seen as the alternative between PD and distal re-section”, and thus, pancreas-sparing techniques may be useful in selected cases. In the present study we aimed to demonstrate that pancreas-preserving duodenectomy is a useful technique and can be indicated in three scenarios: duodenal tumoral disease, periduo-denal disease affecting the duodenum, and/or non-reparable duo-denal trauma.
Total duodenectomy has been described in the treatment of adenomatous duodenal polyposis [9] . The indication for surgery in these patients is focused on cases with severe dysplasia and an el-evated number of lesions or large-sized lesions according to the Spiegelman classification [9–11] . Our series included one case of total duodenectomy due to duodenal adenomatous polyposis. In a recent study, Rangelova et al. [3] compared 81 PDs considered at risk with 20 total duodenectomies and found a higher rate of com-plications among the PDs, thereby justifying the indication of total duodenectomy only in cases of adenomatous duodenal polyposis. The technical complexity of this surgery is high and requires in-depth understanding of the anatomy of the region. Magnetic reso-nance cholangiography can help intervention planning.
Pancreas-sparing total duodenectomy was begun with widely mobilizing the duodenum and cephalic pancreas and locating the papilla with a probe. The intestine was then sectioned, and the duodenum was carefully removed, ensuring that all the vessels ir-rigating the duodenum were ligated. Upon reaching the papilla, the section was made with a scalpel, identifying the pancreatic and the bile ducts. In this case, the patient had a biliary prosthesis, and re-section of the distal bile duct was necessary. After removal of the surgical piece, an ampullary-jejunal suture was performed. The je-junal loop was passed through the retroperitoneum because the transmesocolic passage involved a tension suture and was consid-ered unsafe. Ampullary-jejunal anastomosis was then constructed with neoduodenum. With the jejunal mesentery positioned poste-riorly, the anastomosis was created with an absorbable interrupted 6–0 suture.
The indications for duodenectomy of the third and fourth duodenal portions include cases of malignant duodenal tumors such as duodenal adenocarcinoma, benign tumors such as duode-nal adenoma, neuroendocrine tumors, and duodenal GIST, among others [ 1,12–23 ]. Several studies [ 1,18–22 ] have described the in-dications for duodenectomy in duodenal adenocarcinoma. In 1996, Maher et al. [1] reported their results in 11 patients undergoing surgery for duodenal adenocarcinoma by pancreas-preserving duo-denectomy. Later, in 1998, Sohn et al. [18] analyzed 55 cases un-dergoing surgery: 35 PDs, 13 pancreas-preserving duodenectomies, and 7 palliative surgical procedures. They reported that tumors of the first and second duodenal portions, which should undergo PD, had a worse long-term prognosis. In a study on duodenal adeno-carcinoma of only the third and fourth duodenal portions, Toc-chi et al. [19] found no long-term differences between pancreas-preserving duodenectomy (16 patients) and PD (9 patients). A retrospective populational study in 1611 patients undergoing surgery [20] analyzed the prognostic factors after radical (53.7%) or segmentary resection (46.3%) techniques. The type of surgery performed was not a factor of bad prognosis. On the other hand, the number of lymph nodes resected was greater following rad-ical resection. The extension of lymph node dissection in the re-section of duodenal adenocarcinoma is one of the factors found to influence patient survival [21] . It is clear that surgery is the treatment of choice in duodenal adenocarcinoma, and this proce-dure should include resection with free surgical margins as well as lymphadenectomy of the duodenal lymph node territory [ 18,22 ]. None of the patients with duodenal adenocarcinoma undergoing pancreas-preserving duodenectomy in our study presented dis-ease recurrence. In our opinion, duodenectomy with regional lym-phadenectomy in duodenal adenocarcinoma is a useful option in tumors of the third and fourth duodenal portion without pancreas infiltration.
Duodenectomy may be used for the resection of tumors that infiltrate the duodenum without the need for pancreatic resection to thereby reduce the procedure-related morbidity and mortality. This scenario can be used in surgery of retroperitoneal tumor le-sions or lesions with a low potential of malignancy [ 1,24 ]. In our experience, individualization of the technique is essential to indi-cate this surgery. Therefore, surgery for recurrence of retroperi-toneal liposarcoma is justified since it can lengthen patient sur-vival [24] . In fact, in this latter scenario duodenectomy likely of-fers more advantages over PD because of the overall reduction in surgical aggressiveness. As described above, we performed a duo-denojejunal termino-terminal suture below the papilla similar to what has been reported previously [15] . Another study advocated latero-lateral reconstruction [25],however, this implies performing three anastomoses in the periampullary area, while we prefer to perform only one to avoid further problems during the postopera-tive period.
The treatment of duodenal trauma or major perforated ulcers is technically challenging, and duodenectomy may be considered in patients with this type of lesion. However, recent studies did not include the use of duodenectomy [26–28] . Although major perfo-rated ulcers or duodenal traumatic injuries are uncommon, their management is always technically demanding due to the intrin-sic difficulty of repairing large duodenal perforations with major loss of tissue. Safer techniques such as simple closure with an omental patch, gastric antrectomy with reconstruction, or pyloric exclusion [29] are among the most common options undertaken by emergency room surgeons. Nevertheless, postoperative morbidity in patients with duodenal injuries greater than 2 cm is very high at up to almost 70% [30] . In a recent study, Di Saverio et al. [5] de-scribed the ampulla-preserving first and second portion duodenec-tomies for the treatment of major duodenal intrapapillary perfora-tions with a postoperative morbidity and mortality of 60% and 20%, respectively. This Italian group explained the technique to locate and preserve the papilla safely in detail. However, the technique proposed can only be used in first and second portion duodenal lesions.
On many occasions, duodenal lesions involve the destruction of the third or fourth part of the duodenum, with avulsion of the in-testinal wall that prevents repair by simple suturing and cannot be treated by omental patch or first-party duodenectomy. In this sce-nario, resection of the third and fourth duodenal portion is neces-sary. Surprisingly, this technique is not included in trauma review articles [27–29],perhaps because it is a little-known tool. Indeed, the algorithm proposed by the Western Trauma Association for the management of duodenal trauma [28] including the largest series of duodenal trauma [29] does not include duodenectomy. Accord-ing to the American Association for the Surgery for Trauma (AAST), duodenal lesions classified as AAST IV and V grades should be re-paired by Roux-en-Y duodenoejunostomy or PD [28] . In our opin-ion, the resection of a diseased duodenum and termino-terminal anastomosis seem to be more effective.
While resection of the duodenum is prone to complications, PD also presents significant morbidity, and therefore, the nutri-tional and hemodynamic status of the patient should be evaluated when deciding the most adequate surgical approach. Based on our experience, morbidity with duodenectomy is 54%, although only 14% of our cases were Clavien-Dindo IIIb or greater. Notwithstand-ing, only one patient died following this intervention for reasons not related to the surgical technique. Very few studies have com-pared duodenectomy and PD [ 18,19 ]. In a recent study, Nakayama et al. [2] divided their patients into three groups: PD, and duo-denectomy with or without ampullectomy. There were no deaths in any of the three groups. The postoperative morbidity was sim-ilar in the three groups, with the PD group requiring a higher use of blood derivatives and having a greater index of pancreatic fistula. Nonetheless, the patients undergoing duodenectomy with ampullectomy required a longer hospital stay than the other two study groups. It was of note that they reported less cholangitis in the long-term follow-up in the group undergoing duodenec-tomy without ampullectomy compared to those of the group re-ceiving duodenectomy with ampullectomy and PD (0% vs. 9% vs. 29%, respectively). Two comparative studies on total duodenectomy in adenomatous duodenal polyposis and PD have recently been published [ 3,30 ]. de Castro et al. [30] found no differences between the two surgical techniques, while Rangelova et al. [3] reported fewer postoperative complications in the group undergoing total duodenectomy. In another study, Chen et al. [31] reported pancre-atic fistula in a group undergoing pancreas-preserving duodenec-tomy, and in a comparative study using the propensity score, Liu et al. [32] described a higher mortality in the PD group. Although the postoperative morbidity of pancreas-sparing surgery is high in the short-term, as shown in previous studies [ 8,33 ], the benefit of this type of intervention can be justified in the long term [34] .
In conclusion, pancreas-preserving duodenectomy can be safely used in the treatment of duodenal tumors of the third and fourth duodenal portion, extraduodenal tumors with duodenal infiltration due to proximity and lesions involving duodenal trauma requiring procedures other than primary suture.
Acknowledgments
The authors thank Donna Elaine Pringle and Ariadna Busquets for reviewing the final draft of the manuscript for its content and English style.
CRediT authorship contribution statement
Juli Busquets:Conceptualization, Formal analysis, Investigation, Methodology, Writing -original draft, Writing -review & edit-ing.Josefina Lopez-Dominguez:Data curation, Writing -review & editing.Ana Gonzalez-Castillo:Data curation.Marina Vila:Data curation.Nuria Pelaez:Data curation.Lluis Secanella:Software.Emilio Ramos:Supervision, Validation.Juan Fabregat:Funding ac-quisition, Supervision, Validation, Writing -review & editing.
Funding
This study was supported by grants from the Institut de Inves-tigacióBiomèdica de Bellvitge (IDIBELL Foundation) and the CERCA Programme/Generalitat de Catalunya.
Ethical approval
This study was approved by the Clinical Research Ethics Com-mittee of Hospital Universitari de Bellvitge (PR260/19).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the sub-ject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Comparison and development of advanced machine learning tools to predict nonalcoholic fatty liver disease: An extended study
- Hepatobiliary&Pancreatic Diseases International
- Influence of weight management on the prognosis of steatohepatitis in chronic hepatitis B patients during antiviral treatment
- Key factors and potential drug combinations of nonalcoholic steatohepatitis: Bioinformatic analysis and experimental validation-based study
- LC-MS-based lipidomic analysis in distinguishing patients with nonalcoholic steatohepatitis from nonalcoholic fatty liver
- Cryptococcosis in patients with liver cirrhosis: Death risk factors and predictive value of prognostic models