Stem cell therapies in tendon-bone healing
2021-07-30YueXuWanXiaZhangLiNaWangYueQingMingYuLinLiGuoXinNi
Yue Xu, Wan-Xia Zhang, Li-Na Wang, Yue-Qing Ming, Yu-Lin Li, Guo-Xin Ni
Yue Xu, Wan-Xia Zhang, Li-Na Wang, Yue-Qing Ming, Yu-Lin Li, Guo-Xin Ni, School of Sports Medicine and Rehabilitation, Beijing Sport University, Beijing 100084, China
Abstract Tendon-bone insertion injuries such as rotator cuff and anterior cruciate ligament injuries are currently highly common and severe. The key method of treating this kind of injury is the reconstruction operation. The success of this reconstructive process depends on the ability of the graft to incorporate into the bone. Recently,there has been substantial discussion about how to enhance the integration of tendon and bone through biological methods. Stem cells like bone marrow mesenchymal stem cells (MSCs), tendon stem/progenitor cells, synovium-derived MSCs, adipose-derived stem cells, or periosteum-derived periosteal stem cells can self-regenerate and potentially differentiate into different cell types, which have been widely used in tissue repair and regeneration. Thus, we concentrate in this review on the current circumstances of tendon-bone healing using stem cell therapy.
Key Words: Tendon; Bone; Stem cell; Anterior cruciate ligament; Rotator cuff
INTRODUCTION
The incidence of tendon-bone insertion (TBI) injuries has increased with today’s growing focus on sporting activities. TBI injuries are highly common in both the workplace and sports, such as rotator cuff and anterior cruciate ligament (ACL)injuries; in fact, over 30 million injuries occur worldwide each year[1]. The treatment of such orthopedic injuries includes the reconstruction of the tendon/ligament by moving a tendon graft into a bone tunnel to restore its insertion into the bone of a ruptured tendon or ligament. The success of these reconstructive procedures relies on the ability of the graft to incorporate into the bone.
Failure of tendon-to-bone remodeling can result in high rates of relapse after surgery. Tendon-bone healing also contributes to scar tissue formation, which has limited mechanical properties that make the healed tendons vulnerable to re-injury and thus have elevated re-tear rates[2,3]. The failure rates for rotator cuff repair, for example, have been reported to range from 20% to 94%[2,4], while ACL reconstruction has a failure rate of 10% to 25%[3]. In addition, inadequate tendon-bone healing can result in various secondary symptoms, including knee laxity, movement instability,damage to the meniscus and cartilage, and even early post-traumatic osteoarthritis[5,6]. The site of the tendon graft attachment to the bone is the weakest site in the early healing phase. To protect the healing graft from undue loads, it is also important to postpone mobilization, physical therapy, range of motion exercises, and complex activities[7]. The recovery period is lengthy, preventing an early return to sports.
Various experimental models have shown that after ligament repair, the complex structure and composition of the normal insertion site are not regenerated[7-9]. The interface between the transplanted tendon and the bone tunnel normally recovers along with the fibrous scar tissue, and the configuration and composition of the native direct tendon-bone interface are not reformed during curing; thus the interface mechanically and structurally decreases[10]. The poor healing of the tendon bone interface occurs due to various causes. First, osteointegration and graft remodeling typically recover slowly. Second, if the tendon injury is considerable or if the tendon retraction is broken, the tendon is poorly regenerated after trauma and degeneration[11]. Third, the fibrocartilage area has relative avascularity and bone loss at the injury site[12].
In orthopedics and sports medicine science and clinical practice, the firm healing of a tendon graft to bone involves the healing of two inhomogeneous tissues, which thus has been considered a crucial factor for the long-term success of many reconstructive operating procedures for weakened tendons. The effective integration of tendon-bone healing remains a challenge.
Accelerating and improving tendon-to-bone healing can diminish the risk of injury and allow earlier and more aggressive rehabilitation as well as earlier recovery from work, recreation, or pre-injury activities[13]. Scholars have therefore sought biological therapies to enhance the healing of the tendons. In orthopaedic basic science studies,methods to biologically accelerate and optimize tendon-to-bone healing have been studied meticulously over the past decade. In recent years, techniques such as the use of growth factors[14], platelet-rich plasma (PRP)[15], cell-based therapies[16,17], gene transfer[18], tissue engineering[19], and numerous other methods of delivery and induction have been applied and actively developed.
Stem cells can differentiate in endogenous and exogenous factors into established cell types; they are thus becoming increasingly interesting for researchers. The purpose of this paper is to delineate the current understanding of tendon-bone healing, and to summarize the current state of stem cell therapy for tendon-bone healing.
PHYSIOLOGICAL PROCESS OF TENDON-BONE HEALING
Native structure of TBI
The native TBI is a highly specialized and organized tissue[20] and deforms as a fibrous network[21], which acts as a stress absorber during mechanical loading[22] and transmits complex mechanical loads from soft tissue to bone. In general, TBI can be divided into two categories: Indirect and direct insertions. Indirect insertions, such as the tibial insertion of the medial collateral ligament, include tendon, Sharpey’s fibers,and bone. In contrast, direct insertions, such as the insertion of the ACL and rotator cuff, can be classically categorized into four zones. Benjaminet al[23] reported that the research of Dolgo-Saburoff in 1929 and Schneider in 1956 first showed four zones at TBI (Figure 1).
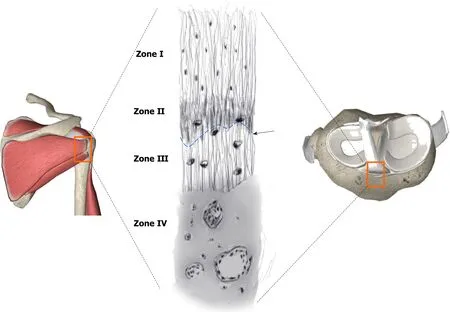
Figure 1 Structure of the tendon-bone insertion. Zone I consists of ligament. Zone II comprises nonmineralized fibrocartilage. Zone III is composed mineralized cartilage. Zone IV consists of bone. Tidemark between Zone II and Zone III (black arrow) is shown.
Zone I is a ligament that contains an extracellular matrix of proteoglycans and consists of highly aligned type I collagen[24,25], particularly of dermatian sulphate.The only cells in this region are fibroblasts. The mechanical properties are identical to the mid-substance tendon-like properties[26]. Zone II is a nonmineralized cartilage region of fibrocartilage cells aligned within the bundles of collagen. This zone primarily contains a mixture of forms of collagen II and III and the proteoglycan aggregate[27] and has a more networked organization[28]. Zone III is the region of cartilage that is mineralized. The fibrocartilage is mineralized in this area and inserted into the subchondral bone layer. Between Zones II and III, there is a distinct basophilic“blue line” or the “thread mark” between the mineralizations. The structure is reinforced by mineral deposits on the nanometer scale[29]. Here, collagen type II predominates, and both the collagen type X and aggrecan are important in specific quantities[26,27]. Zone IV is made up of bone attached to the ligament. Its matrix consists mainly of chondroitin sulfate and mainly of collagen type I mineralized in osteoblasts, osteocytes, and osteoclasts[28]. Traditionally, these areas are known to be explicitly differentiated but structurally continuous. This particular anatomy insertion point is intended to serve as a “two-layered defense system” shielding the bone from excessive shear stress and the tendon from excessive pressure or strain.
Process of tendon-bone healing
A dog tendon-bone healing model was used by Rodeoet al[8], who suggested that bone tendon healing should be carried out by the development of a fibrovascular interface tissue between the tendon and bone, accompanied by gradual bone ingrowth into this interface tissue. In the 24 wk after ACL reconstruction in rabbits, Schiavone Panniet al[30] demonstrated that the junction between tendon and bone was morphologically complete. Granaet al[7] then found in an ACL reconstruction model of rabbit,the strengthening of collagenous fibers in the tubes in a bone at 12 wk after the operation had been completed by intertwining of graft and connective tissue and the attachment of connective tissue to bone in tunnels. The collagenous fibers appear in an indirect inclusion of the Sharpey’s fibers. In 1997, Liuet al[31] outlined the process of tendon-bone healing in a rabbit model. Inflammatory cells in the tendon-bone interface are present after 1 wk. Scar tissue occurred after 2 wk. The scar tissue at the interface from bone to tendon was then gradually reorganized 4 wk after the surgery into a dense connective tissue matrix, continuously with bone and tendon juxtapositions. After 6 wk, a more longitudinal reorganization of the disorganized collagen fibers was observed, and Sharpey’s fibers were noted.
The histological findings concerning hamstring insertion healing of the ACL reconstruction in 12 patients were recorded by Robertet al[32]. The initial tendon-bone contact region was osteolyzed, with lamellar bones partially covered by an osteoid bone at a rate of 3 mo replaced with highly cellular and fibrovascular tissue. After 6 mo, the fibrous interface came into continuous contact with the lamellar bone osteoid tissue, while Sharpey-like fibers began to become evident. The quantity of Sharpeylike fibers became apparent at 10 mo, and the healing process matured. It was reported that the time needed for a mature indirect anchorage was 10 to 12 mo, which is approximately 6 to 24 wk longer than that in the animal model. But few studies have examined tendon-to-bone healing for human beings, mostly because patients have biopsied the whole grease in a small focal area, without examining the entire graft, as would be done in an animal model[33]. Second, the harvest is simple using an arthroscopic technique in the joint part of a graft, although it is truly difficult to harvest the bone-tendon intersection[34].
Luiet al[35] summarized the tendon graft stage a few years later for the bone tunnel cure. It can be divided into four different phases. Stage 1 is the inflammatory phase;during this stage, inflammatory and marrow-derived stem cells are invaded and recruited. An interposed fibrovascular layer of scar tissue is at the interface between the graft and tunnel. Stage 2 is the proliferative phase, which involves the proliferation and differentiation of the stem cells. Interface cells release cytokines and growth factors, resulting in blood vessels and nerves growing[36]. Stage 3 involves the process of matrix synthesis, and the new extracellular matrix is synthesized and processed with the incremental entry of the bone. Stage 4 is the phase of the matrix regeneration,wherein, the newer bone, interfacial fabric, and graft remodeling, like Sharpey's fibers of an indirect insertion, are developed with consistency between the tendon graft and the bone of collagen fibers[37,38]. A decrease in cellularity occurs at the interface. As Sharpey's fibers continuously increase over time, the mechanical strength of the interface increases gradually.
TYPES OF STEM CELLS
Stem cells have the capacity to self-regenerate, differentiate into different cell types,and harness a repair mechanism by being able to divide without limits to regenerate other cells; they are therefore currently being studied by researchers and becoming a common treatment option for musculoskeletal injuries such as ACL injuries and rotator cuff tears. For successful results of stem cell therapies, the cell source is important[39].
Numerous sources for stem cells are available and so stem cells can also be classified according to their origin tissue: Embryonic stem cells, fetal stem cells, umbilical cord stem cells, and adult stem cells. One study has shown that human placenta-derived mesenchymal stem cells (MSCs) with strong proliferative ability have rich sources and can remarkably promote tendon-bone healing in a rat model after cell transplantation[40], but the ethical and legal issues arising from human placenta-derived MSCs,making it difficult to perform more trials. It still needs more evidence to confirm the efficiency of placenta-derived MSCs on tendon-bone healing.
There are currently two principal types of clinically promising adult stem cells:Hematopoietic stem cells and MSCs. Several recent studies have shown that MSCs are obtainable from synovium[41], periosteum[42], and adipose tissues[43], which have been widely used in tendon-to-bone repair. Each source has its advantages,inconveniences, and capacity for differentiation. Bone marrow MSCs (BMSCs) can be collected from the anterior iliac crest, posterior superior iliac crest, tibial tubercle, or sternum. The harvesting method is invasive and requires local anesthesia, which can cause additional pain in patients. The study suggested that thein vitroexpansion possibilities of BMSCs were limited[44]. The tendon stem/progenitor cells (TSPCs),which have proliferated more colongenically than BMSCs[45], exhibited higher colongenicity. In addition, TSPCs have indicated higher tenogenic markers, such as scleraxis (Scx) and tenomodulin (Tnmd)[45]. The TSPCs, such as those in tendons of Achilles, patella tendons, supraspinatus seins, or hamstring tendons, may be harvested from waste tendon tissue during tendon and ligament surgery. However, sufficient TSPCs are required in thein vitrocell culture. Recently, more and more studies have uncovered the potential both for proliferation and for chondrogenesis in synoviumderived MSCs (SMSCs) rather than in BMSCs[46,47]. However, SMSCs require secondary surgery from the knee joints and shoulder. It requires a long duration ofin vitroexpansion to achieve sufficient stem cells. Adipose-derived stem cells (ADSCs)can be obtained in the hips and thighs, or around incisions, from the subcutaneous adipose tissue. Studies have demonstrated that adipose has significantly more MSCs than bone marrow, and the yield of ADSCs is higher than that of BMSCs. Periosteumderived periosteal stem cells (PSCs) can be harvested from the tibia or the humerus inferior to the tip of the greater tuberosity. An analysis found that the osteogenic,chondrogenic, and adipogenic capacities of rat PSCs were greater than those of BMSCs[48]. Table 1 indicates various differentiation capacities among MSCs.
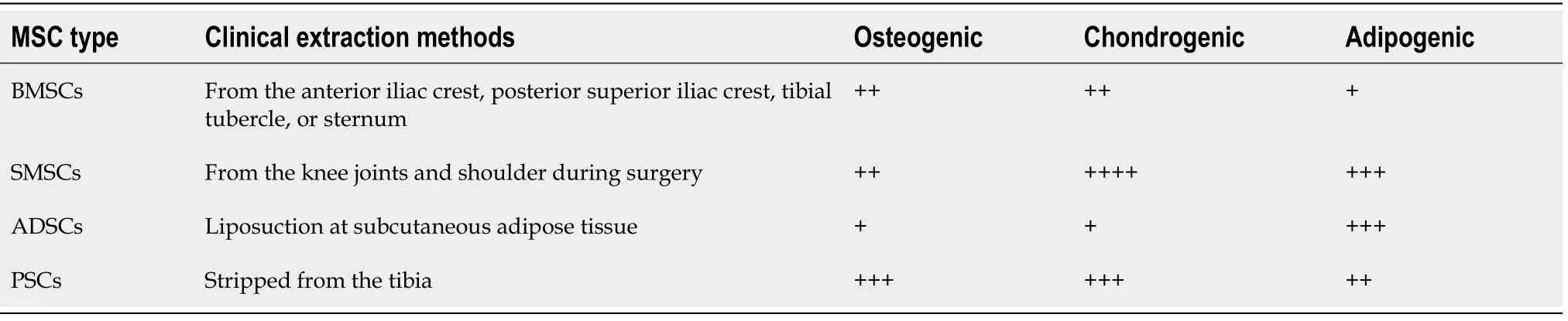
Table 1 Summary of differentiation capacities between different mesenchymal stem cell types
BMSCS
The use of biological agents to improve tendon bone healing is becoming increasingly relevant. Studies have proven the potential for better tendon-bone healing for a decade using bone morphogenic protein (BMP)-2[49] and a mixture of bone growth proteins[14]. BMSCs can be collected from the pelvic, femurs, tibias, and humeri. BMSCs are pluripotential cells that have been extensively studied in the treatment of tissue injury[50,51].
Pre-clinical studies
Limet al[52] and Ouyanget al[53] used BMSCs for the first time in the study of tendonbone healing. Limet al[52] investigated the impact of BMSCs grafting of a rabbit ACL on the rate and consistency of graft osteointegration. After 2 wk, the BMSCs group had large areas of cartilage cells at the tendon-bone junction. The BMSCs group had a mature cartilage zone after 8 wk, which stained strongly for collagen type II, blending a mature cartilage zone, and increased failure load and stiffness. They concluded that the coating of tendon grafts with BMSCs contributes to a cured cartilage zone close to regular ACL inserts instead of collagen fibers and scar tissues. This also helps in the treatment of the collagen fibers. A few years later, Lim and his colleagues[54] studied a rabbit ACL reconstruction model and found similar results, the effect of coating allografts with BMSCs on the consistency and rates of the osteointegration of the allograft tendon and bone interface. In 2019, Huret al[55] investigated the effects of BMSCs on tunnel widening in a rabbit ACL reconstruction model. The BMSCs group had a lower mean for the enlargement of the femoral tunnel and an extension of a tibial tunnel to the oblique sagittal image. Hypercellular architecture and compact collagen deposition were present in the BMSCs group. They showed that BMSCs appear to reduce the expansion of the tunnel in the reconstruction of ACL.
The effectiveness of using a large number of BMSCs to boost tendon-to-bone healing in a rabbit tendon-bone healing model was evaluated by Ouyanget al[53]. The BMSCs group exhibited more perpendicular forming of collagens and an increased growth in cartilage-like cells, which was indicated by positive collagen type-II immuno-staining of the tendon-bone interface. They argued that BMSCs could enhance the insertion of tendon healing to the bone through the formation of fibrocartilaginous attachment at an early stage. Seven years later, Liet al[56] investigated the effects of BMSCs on a model of rat tendon-bone healing. In the BMSCs group, at 4 and 8 wk after surgery,the maximum biomechanical production strength was significantly higher.
Some studies then compared the effects of various cells. In a rat model of degenerative enthesis reparation, Nourissatet al[57] assessed the impact of depositing BMSCs or chondrocytes. They developed a model based on the destruction of the Achilles tendons enthesis and found that rats with BMSC injections were arranged into the column of chondrocytes 45 d after surgery in a native enthesis. Kidaet al[16]analyzed the kinetics of BMSCs with bone marrow chimeric rats, which expressed green fluorescent protein (GFP) during the rotator cuff repair. An additional drilling procedure was performed at the greater tuberosity. They found that more GFPpositive cells and a higher rate of ultimate force-to-failure in the drilling group. After 3 years, Degenet al[58] assessed the capacity of human BMSCs to augment the healing of an acute small-to-medium-sized rotator cuff repair in a rat model. At the repair site,BMSCs increased the development of fibrocartilage, strengthened collagen orientation,and increased load failure and stiffness over 2 wk. In the histological and biomechanical findings, there were nevertheless no major variations in 4 wk. Luet al[59] then compared the effects on tendon-to-bone healing of the fresh autologous bone marrow and BMSCs with a novel rat model. The bone marrow group showed a relatively wellorganized and dense connecting tissue interface with an enhanced collagen fiber orientation, less M1 macrophages and more M2 interface macrophages. Biomechanical tests indicate that the bone marrow group exhibits considerably higher stiffness. They demonstrated that local delivery of fresh autologous bone marrow better improvestendon-to-bone healing more than BMSCs due to inflammatory modulations.
On the contrary, Gulottaet al[60] determined the effect of BMSCs in a rat rotator cuff healing model. Histological and biomechanical evaluations between groups did not vary at any given time. The study concluded that adding BMSCs to the insertion site of the healing rotator cuff did not change the site's structure, composition, or strength.Similarly, a study by Kanazawaet al[61] concluded that the use of BMSCs alone in a reconstruction model of rabbit ACL with no tibial bone tunnel was unable to enhance the tendon-to-bone healing to a sufficient extent (Table 2).
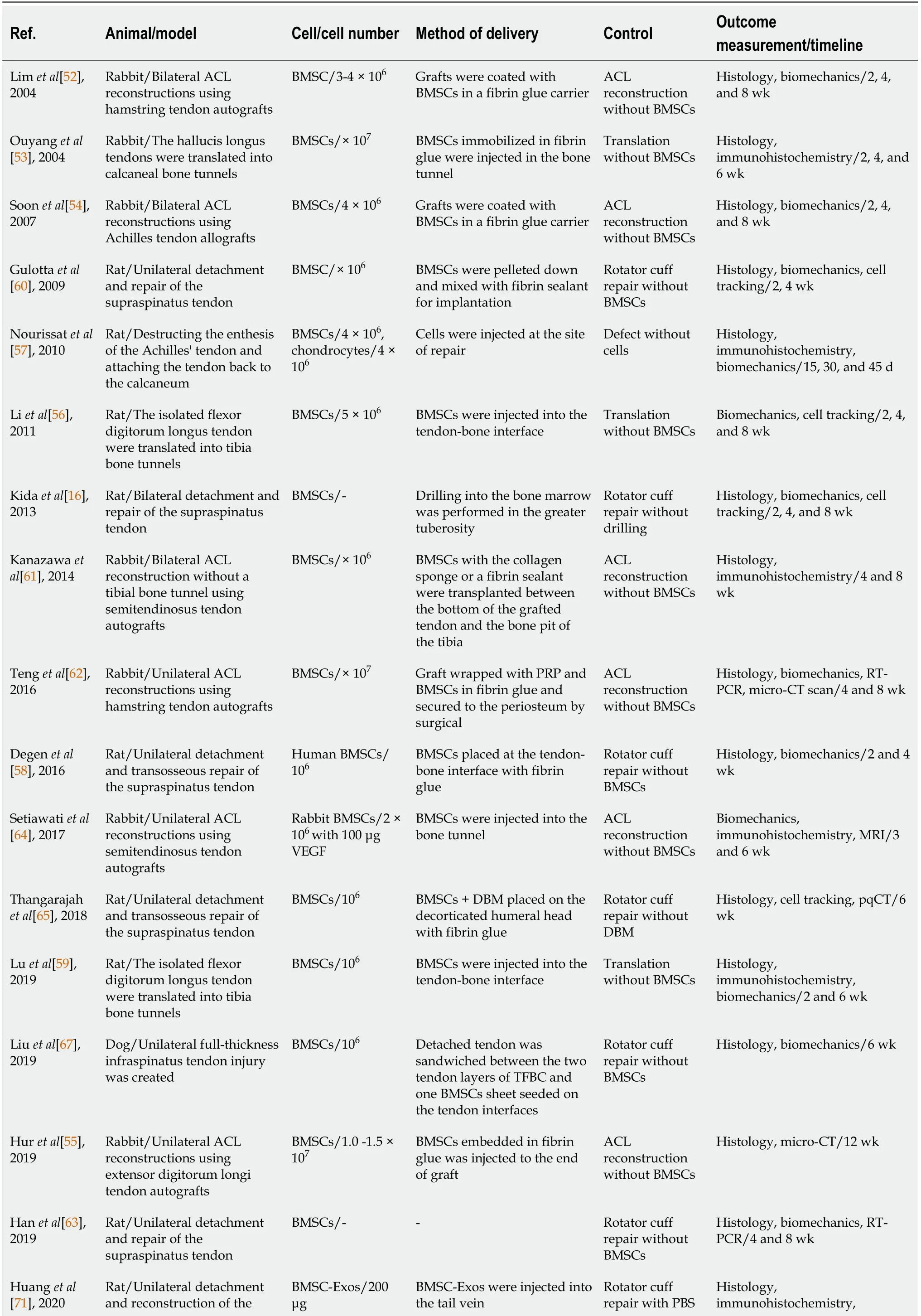
Table 2 Summary of pre-clinical studies using bone marrow mesenchymal stem cells
BMSC: Bone marrow mesenchymal stem cell; ACL: Anterior cruciate ligament; MRI: Magnetic resonance imaging; pqCT: Peripheral quantitative computed tomography; DBM: Demineralized bone matrix; RT-PCR: Reverse transcription polymerase chain reaction; RT-qPCR: Reverse transcription quantitative polymerase chain reaction; TFBC: Tendon-fibrocartilage-bone composite; Exos: Exosomes; PBS: Phosphate-buffered saline.
Stimulating factors
Above all, the results of using BMSCs in tendon-bone healing are inconsistent. Many researchers believe that different stimulating factors with BMSCs may enhance tendon-bone healing. In 2016, Tenget al[62] investigated the potency of PRP combined with BMSCs to advance tendon-bone healing in a rabbit ACL reconstruction model. A more mature interface with aligned chondrocytes and a higher failure load was observed in the BMSC + PRP group. They concluded that the combination of PRP and BMSCs promoted tendon-bone healing. Hanet al[63] found similar histological and biomechanical findings regarding the treatment of tendon-bone injuries after rotator cuff injuries a couple of years later. They proved that the combination of BMSCs and PRP synergistically stimulates tendon bone healing through stronger signals associated with angiogenesis, bone formation, andin situtendon generation. Setiawatiet al[64] then tested whether injecting BMSCs and vascular endothelial growth factor(VEGF) into the bone tunnel of rabbits after ACL reconstruction would improve the early healing process of a tendon graft. They found a higher mean collagen type III score, a higher value for the final tensile strength, as well as improved signal intensity for magnetic resonance imaging (MRI) in the group BMSCs + VEGF. They also demonstrated that BMSC and VEGF injections of intra-tunnels improved the graft tunnel healing after ACL reconstruction.
Tissue engineering
Stem cell tissue engineering is becoming more commonly used in tendon-bone cure due to the rapid advancement of tissue technology. In 2018, Thangarajahet al[65]investigated the potential of a demineralized bone matrix (DBM) improved with BMSCs, when used in a degenerative rotator cuff tear model, to enhance tendon bone healing. A DBM consists of a network of collagen fibers that provide a sustained release of growth factors such as BMPs[66]. All groups showed that the tendon-bone gap closure was observed with fibrocartilaginous entheses and the DBM + BMSCs group reached not significantly lower than non-operative checks in bone mineral densities. They concluded that the biological increase in the DBM and MSC rotator cuff repair will minimize the incidence of re-tear. In a canine non-weight-bearing model of acute, full-thickness tendon injury, Liuet al[67] examined the effects of an engineered tendon-fibrocartilage-bone composite (TFBC) combined with BMSCs sheet on rotator cuff healing. The TFBC includes native fibrocartilage enthesis focused on more durable tendon-to-tendon and bone-to-bone homogeneous tissue cure, as well as a multilayered cell seeding structure close to the collagen-cell composition of the native tendon[68]. The TFBC + BMSCs group had increased formation of new fibrocartilage and collagen fiber organization at the interface of the tendon bone and the ultimate failure and stress. They evidenced that the application of an engineered TFBC and BMSCs can enhance rotator cuff healing.
Exosomes
As major mediators of intercellular communication, exosomes emerge to regulate a range of biological processes by means of the transmission of biological signs between cells. Exosomes are highly biomass-free and can remove the barrier of the tissue.Exosomes are beginning to be investigated in relation to diseases, including cancer,infectious disorders, and neurodegenerative disorders[69]. But in the process of tendon-bone healing, there is a lack of research on the mechanism of exosomes. In 2020, Shiet al[70] investigated the effects of BMSC-derived exosomes (BMSC-Exos) on tendon-bone healing. In the BMSC-Exos group, more fibrocartilage, higher maximum force, higher intensity, higher elastic modulus, higher M2 macrophage numbers, and more anti-inflammatory and chondrogenic factors were observed. They demonstrated that by enhancing M2 macrophage polarization in tendon-to-bone healing, BMSC-Exos promote the formation of fibrocartilage. Subsequently, Huanget al[71] explored the role of BMSC-Exos in a rat rotator cuff reconstruction model. BMSC-Exos stimulated angiogenesis across the interface of the tendon bone and prevented M1 macrophages from releasing associated inflammatory factors. After rotator cuff repair, BMSC-Exos improved the breaking load and stiffness. They concluded that BMSC-Exos facilitate tendon-bone healing by encouraging angiogenesis and suppressing inflammationviathe VEGF and Hippo signaling pathways.
Gene therapy
Many scientists believed that BMSCs alone are not adequate to improve tendon-bone healing, and they hypothesized that BMSCs need a signal to increase their effectiveness, such as a growth factor or transcription factor[72]. Hence, in tendon-bone healing studies, gene-modified BMSCs are commonly used.
In 2010, Gulottaet al[72] examined whether BMSCs transduced with adenoviral membrane type 1 matrix metalloproteinase (Ad-MT1-MMP) could enhance healing following the repair of rotator cuffs when applied to the tendon-to-bone insertion site.MT1-MMP is a membrane-bound matrix of metalloproteinase, which plays a role in the embryological formation of musculoskeletal tissues[73,74]. MT1-MMP is induced by promoting the dissolution of the anlagen cartilage and the production of mineralizing cartilage[73] to guide the process of endochondral ossification. In any outcome variable, there were no variations after 2 wk. The Ad-MT1-MMP group had more fibrocartilage, increased ultimate failure load, ultimate failure tension, and higher stiffness values after 4 wk. It was concluded that genetically modified BMSCs would stimulate rotary cuff healing by increasing the amount of fibrocartilage at insertion and by improving bio-mechanical strength by overexpressing developmental geneMT1-MMPafter 4 wk. Then they applied BMSCs transduced with adenoviralmediated Scx, a basic helix-loop-helix transcription factor that is believed to direct tendon development during embryogenesis[75], in a rat rotator cuff repair model[76];they found similar results. However, they found negative results when using BMSCs transfected with BMP-13 in a rat rotator cuff model in the same year[77]. They concluded that applications to overexpress MT1-MMP or Scx of genetically modified MSCs can enhance the early treatment of rotator cuff.
Several years later, Donget al[78] investigated the efficacy of a rabbit reconstruction model of BMSCs with BMP-2 for tendon-bone healing. Higher maximum loading and stiffness and increased proliferation of cartilage-like cells and fibrocartilage-like tissue were observed for the BMSCs + Lv-BMP-2 group. After 5 years, Wanget al[79]explored the role of transforming growth factor-beta (TGF-β) in tendon-bone healing after ACL reconstruction. BMSCs were infected with TGF-β. There were more fibroblasts, a tighter tendon-bone interface, and an increasing number of cells and fibrochondrocytes close to chondrocytes and other collagen-fibers, in the overexpression group. Due to maximum load and stiffness, the bone tunnel and bone tunnel margin computed tomography values in the overexpression group were substantially up-regulated. It was shown to promote tendon-to-bone healing by up-regulating TGFβ expression in BMSCs after ACL reconstruction by adjusting the signal pathway TGFβ/MAPK. The effect of platelet-derived growth factor subunit B (PDGF-B) on tendonbone healing after rotator cuff injury repair by modifying BMSCs was then investigated by Wanget al[80]. BMSCs were transfected with recombinant lentiviral vectorencoded PDGF-B shRNA, overexpressed Pc-DNA PDGF-B, and irrelevant plasmid.They found that PDGF-B could promote viability, osteogenic differentiation, and adipogenic differentiation. The ultimate load and stiffness of the tendon tissue can be improved by PDGF-B. They evidenced that overexpressed PDGF-B could act to enhance tendon-bone healing after rotator cuff injury repair (Table 3).
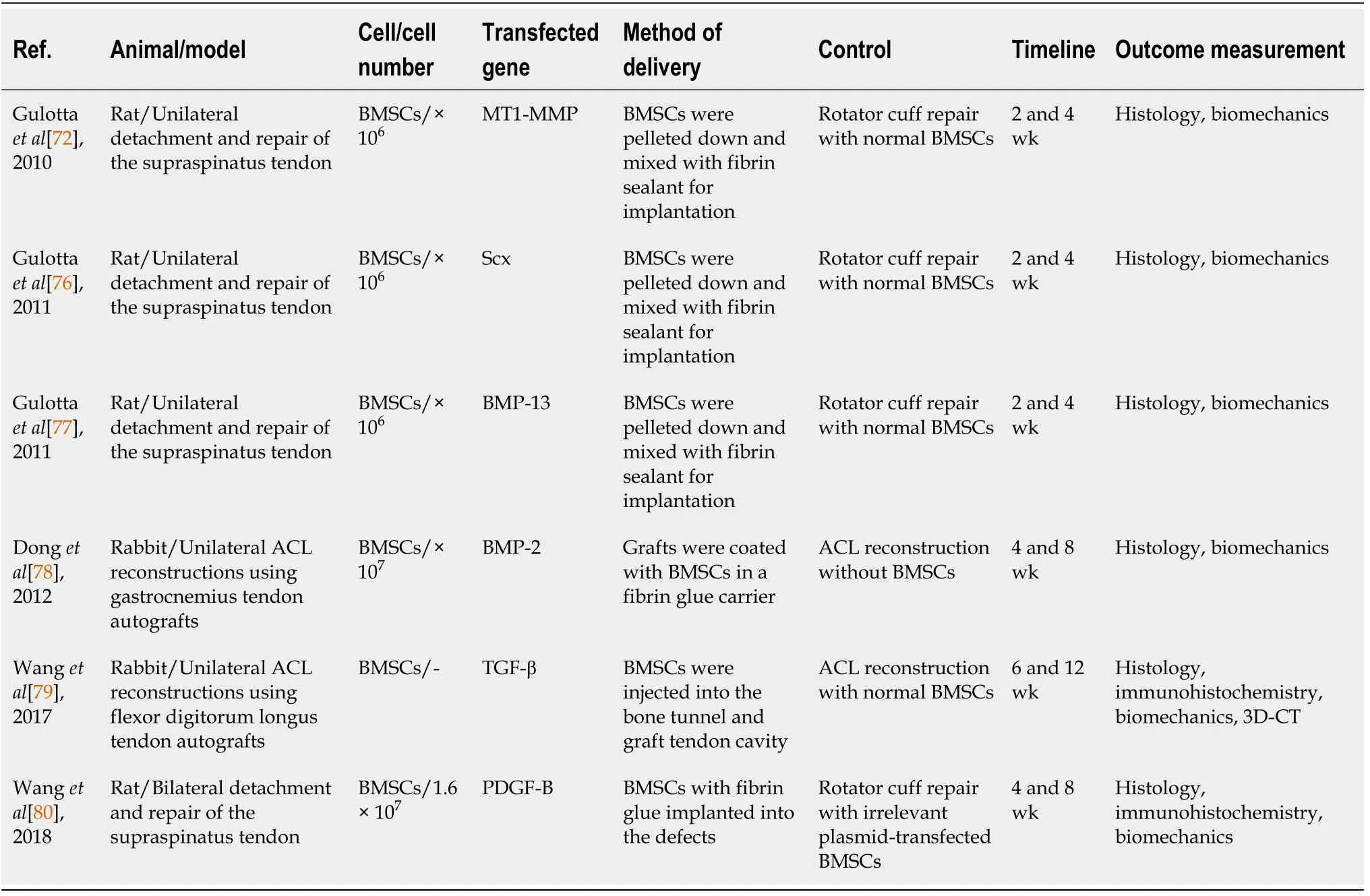
Table 3 Summary of pre-clinical studies using gene-modified bone marrow mesenchymal stem cells
Clinical studies
The clinical use of BMSCs was discussed in many orthopedic fields as a means to improve tissue regeneration. Recently, researchers have demonstrated that BMSCs cross holes drilled in the humerus footprint, penetrated the repaired rotator cuff, and contributed to the healing of the postsurgical rotator cuff[16]. Multiple channeling technology is a simple and straightforward procedure which allows BMSCs to travel from the cavity of bone marrow to the repair site of the rotator cuff tendon in the greater tuberosity of the proximal humerus[81].
The impact of BMSCs on the clinical and structural findings regarding arthroscopic rotator cuff repair was first investigated by Joet al[82]. Among 124 patients, 57 underwent multichannel arthroscopic rotator cuff repair. They followed the patients for at least 2 years. Outcome measures included the visual analog scale (VAS) for pain,range of motion (ROM), MRI, computed tomography arthrography, and commonly used functional scores such as the American Shoulder and Elbow Surgeonsscale, the Constant score, the University of California, Los Angeles (UCLA) scale, the Disabilities of the Arm, Shoulder and Hand scale, the Simple Shoulder Test, and the Shoulder Pain and Disability Index scale. In terms of VAS, ROM, pain, strength, and functional scores, there was no statistical difference between the multiple channel group and conventional group. However, the re-tear rate was 22.2% in the multiple channel group, slightly lower than that of the conventional channel group. They concluded that the extravasation of bone marrow containing MSCs from the proximal humerus to the repair site was caused by multiple channeling, and the re-tear rate decreased significantly after the repair of arthroscopic rotator cuffs. Similarly, Taniguchiet al[83]investigated the effect of BMSCs on cuff repair integrity after arthroscopic surfaceholding (ASH) repair using multiple channeling in 111 patients. Sugaya’s classification was used to evaluate cuff integrityviapostoperative MRI. The re-tear rate for largescale tears was significantly higher in the non-BMSCs group (28.6%) than in the BMSCs group (4.5%). They showed that the application of BMSCs to the footprint during ASH repair results in an improved integrity of the cuff repair particularly in massive tears. Among 90 patients who underwent arthroscopic rotator cuff repair involving injecting cells into the interface, Hernigouet al[84] assessed the efficiency of biological augmentation of rotator cuff repair with BMSCs. They used MRI and ultrasound at least 10 years later to confirm healing or re-tearing of the rotator cuff.They found that 87% of patients in the BMSCs group had intact rotator cuffs, but only 44% patients in the control group. In conclusion, during rotator cuff repair, the injection of BMSCs as a form of adjunctive therapy increased the healing rate and improved the consistency of the repaired surface, as determined by ultrasound and MRI.
In comparison, Silvaet al[85] concluded that in 43 patients, adult non-cultivated BMSCs do not tend to accelerate graft-to-bone healing in ACL reconstruction by MRI.No difference was observed between the BMSCs and control groups in the signal-tonoise ratio of the MRI interzone. In their study, bone marrow was harvested from the anterior iliac crest with the syringe in the MarrowStim Concentration System kit(Table 4).
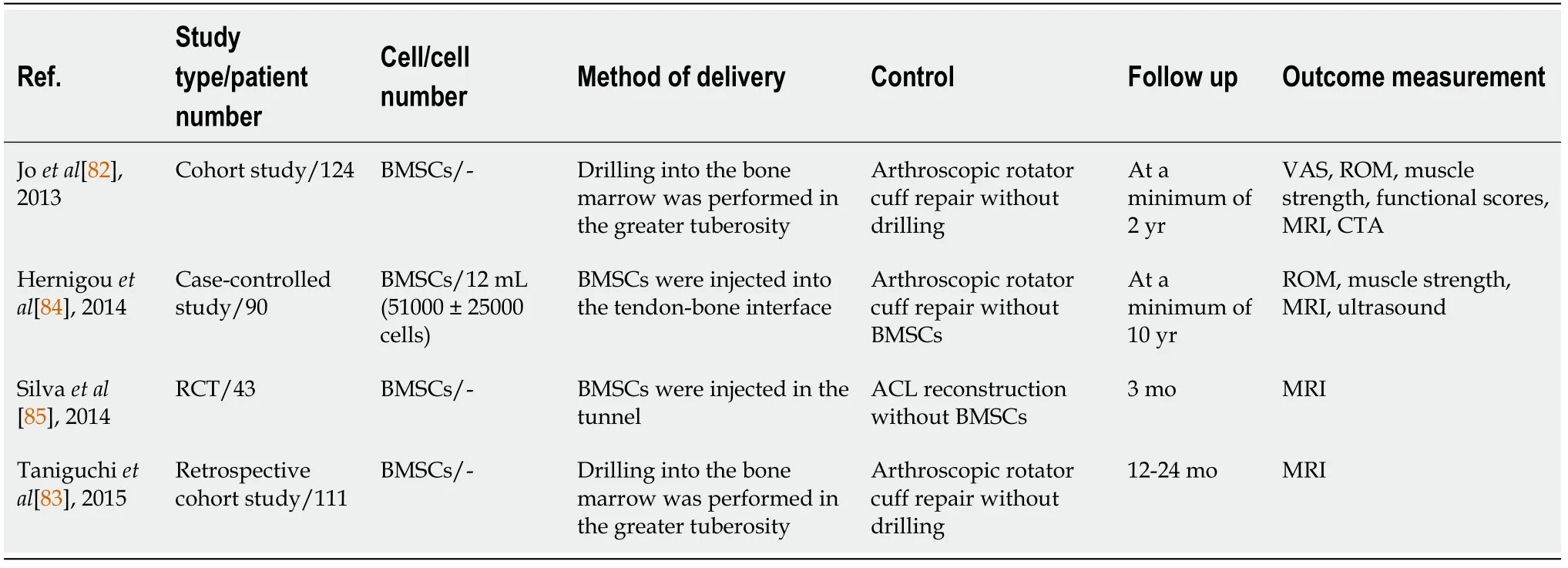
Table 4 Summary of clinical studies using bone marrow mesenchymal stem cells
BMSCs can be acquired clinically from the anterior iliac crest, posterior superior iliac crest, tibial tubercle, or sternum. A second surgery is required to obtain sufficient BMSCs, leading to further trauma and suffering. While several studies have shown promising BMSCs for the repair of human rotator cuffs, clinical trials appear to have been scarce in the recent past. These studies have some limitations, including the limited sample group, the short follow-up duration, the lack of objective measurement methods, and the lack of randomization. More randomized, large-sample, long-term trials would be needed in potential clinical studies. To determine minor changes in histology in the tendon-to-bone interface, further evaluation methods will be necessary. Furthermore, there has been no identification of the number and quality ofthe recruited BMSCs and no clarity on the mechanism. In addition, tissue engineering with BMSCs has not been reported in clinical research, and further research is needed.Recently, Vosset al[86] designed a PRP fibrin clot, a scaffold for stem cell delivery. The technique used in the clinic was associated with a lack of clinical outcomes, however,the fibrin scaffold will retain the viability of BMSCs for lengthy periods (> 4 wk).
TSPCS
Remarkable progress has been made in the identification of human and mouse TSPCs with universal stem cell characteristics, including clonogenicity, multipotency, and self-renewal capacity[87]. Then, TSPCs have been identified in rabbits and rats[88,89].de Moset al[90] also demonstrated the multi-differentiation potential of explanted human tendon cells. Not only do these cells have universal stem cell properties similar to BMSCs, but they are also strongly characterized by tendon-connected genes and proteins, including collagen I, tenascin C, Scx, and Tnmd[87]. Although MSCs are commonly used in tendon-bone interconnection repairs isolated from various tissues,the use of tendon stem cells for the reparation of the tendon-bone interconnection may be beneficial in the light of the fact that the tendon environment is ideal and familiar to facilitate grafting and differentiation between transplanted cells[91]. More researches have recently examined the effectiveness of TSPCs in the context of tendon-bone injury.
Tissue engineering has been shown to be promising for tendon-bone junction repair by means of stem cell therapy. In the promotion of rotator cuff regeneration in a rabbit model, Shenet al[17] investigated the effectiveness of TSPCs seeded knitted silkcollagen sponge scaffold. The implantation of TSPCs allogenous scaffolds 4 and 8 wk post-operation increased fibroblastic cell growth and decreased lymphocyte infiltration at implantation locations. The allogenous TSPCs group exhibited improving structural and biomechanical properties at 12 wk after surgery. They showed that by differentiating into tenocytes and secreting anti-inflammatory cytokines, the allogenous TSPCs knitted silk-collagen sponge scaffold improved the efficacy of rotator cuff tendon regeneration. For cell transmission, cell sheets do not need external scaffolds. TSPCs form a cell sheet that displays greater tenogenicity and retains a high expression level of the chondroosteogenic gene by TSPCs. Luiet al[91] used a TSPCs sheet in a rat ACL reconstruction model. In the TSPCs group, bone volume and total volume were considerably higher after 2 and 6 wk. Semiquantitative image analysis showed improved graft osteointegration and higher intra-articular graft integrity with lower cellularity and vascularity, better cell alignment, and increased collagen birefringence in the TSPCs group. The TSPCs group displayed better results than the control group under biomechanical analysis. They concluded that after restoration of the ACL, the TSPCs sheet enhanced early graft healing. Cell sheets of human rotator cuff-derived cells were used in a rat rotator cuff injury model by Yoshifumiet al[92].Proteoglycan was found to be positive for more type II collagen and isolectin-B4 cells in the sheet group,VEGFand type II collagen gene expression was higher, and tenomodulin gene expression was lower in the sheet group than in the control group.The sheet group displayed a considerably higher ultimate failure load in mechanical testing at 8 wk than the control group. Their results indicated that the rotator-cuff derived cell sheet could promote cartilage regeneration and angiogenesis at the enthesis, with superior mechanical strength. Although the studies support TSPCs in the repair of tendon and tendon bone insertion as an alternative cell source, no clinical research has addressed repair of following TBI.
Research concerning the mechanism by which TSPCs improve tendon-bone healing is scarce. Chenget al[93] investigated the role of TNF-alpha-stimulated gene/protein 6(TSG-6) in the treatment of rotator cuff healing with TSPCs. It was concluded that TSG-6, a therapeutic protein manufactured by TSPCs to respond to injury signals,prevented the formation of fibro-vascular tissue in the tendon-to-bone interfaceviainflammation suppression. The other mechanism is still unknown, and the actual mechanisms must be researched further.
Autologous tendon stem cells are difficult to acquire without inducing site morbidity or second stage surgery for the donor. Researchers have now shown that tendon stem cells have been immune-privileged and can be used for the transplantation of allogenes[91]. TSPCs could be easily isolated from the waste tendon tissue during tendon/ligament surgery, such as with the residual tendon graft tissue in ACL reconstruction and the waste tendon tissue in total knee replacement[91]. The study using TSPCs on tendon-bone junction injury is still in its infancy. Further research is needed to test the effectiveness of TSPCs application in a large-animal model and identify the efficacy of thisin vivo.
SMSCS
Recently, SMSCs are becoming increasingly popular and are widely used in cell-based tissue repair[94-96]. It has been reported that MSCs from the synovium have a higher chondrogenic potential than those from infrapatellar fat pad, adipose tissue, and bone marrow[97,98]. Therefore, SMSCs were introduced in recent years to accelerate tendon bone healing.
Juet al[99] excised bilateral knee joint rat synovial membrane to provide a single-cell suspension of SMSCs and labeled it with CM-DiI. Atelocollagen gel with or without rat SMSCs was injected into the interface of bone and tendon during surgery. The interface was full of abundant DiI-labeled SMSCs at week 1, and the amount of collagen fibers in the interface had increased significantly. After 2 wk, Sharpey’s fibers seemed to be slightly higher in the proportion of oblique collagen fibers between the tendon graft and bone tunnel. The tendon-bone interface tissue vanished after 4 wk,and the inserted tendon tended to connect directly to the bone. At this time, DiIlabeled cells can no longer be detected. They proposed that implanted SMSCs could differentiate into fibroblasts and accelerate early remodeling of tendon-bone healing,although they cannot regenerate a stable insertion of fibrocartilage. In conclusion,SMSCs can enhance tendon-bone healing effectively by accelerating fibrous structure formation.
Knee and shoulder joints can be used to generate SMSCs. Recently, several studies have indicated that the subacromial bursa is an effective candidate for the source of SMSCs in rotator cuff tears[98,100]. However, the use of SMSCs for clinical research is still scarce. The acquisition and cultivation of SMSCs require secondary surgery, which will burden patients financially, making it difficult to perform clinical trials. In the future, further biomechanical research for the tendon-bone complex should be conducted to assess whether the SMSC truly biomechanically improves early tendonbone healing. This will also entail more scientific studies involving large animals.Furthermore, to investigate the therapeutic effectiveness of SMSCs, more clinical trials should be performed.
ADSCS
As a potential source of undifferentiated MSCs, adipose tissue has recently been garnering interest. The stem cell derived from adipose is a progenitor cell that can proliferate and differentiate into various types of mesenchymal cells, such as tenocytes or myocytes, and release growth factors and cytokines locally[101,102]. Since ADSCs can easily be obtained in large quantities from subcutaneous adipose tissue without the need for culture and expansion, they have been widely used in research in recent years.
Pre-clinical studies
Several animal studies have shown that the local repair and regeneration of adipose tissue, muscle, endothelial tissue, and bone can be improved by ADSCs[102-104]. In a rabbit rotator cuff tear model, Ohet al[105] injected ADSCs to verify the effects of tendon-bone healing. In terms of electromyographic assessment, the ADSCs group exhibited a larger compound muscle action potential area and higher load-to-failure result. They concluded that local administration of ADSCs could enhance tendon bone healing. However, only the biomechanical pullout strength was calculated with no histological assessment of tendon-bone healing. Moraet al[106] reported that using ADSCs in a rotator cuff repair rat model did not enhance tendon-to-bone healing biomechanical properties, but ADSCs were able to inhibit inflammatory reaction,which could result in more elastic and less scarred repair. With a diminished presence of oedema and neutrophils in the ADSCs group, histological analysis revealed less acute inflammation. But the orientation of collagen fibers and biomechanical variables in each group did not vary after 2 and 4 wk. Similar findings have been yielded by Barcoet al[107].
Kosakaet al[108] evaluated the therapeutic effect of ADSCs administration on tendon-bone healing in a rabbit ACL reconstruction model. The size and type of chondroide cells and Sharpey-like fibers were more orderly and consistently; they were previously seen in the ADSC treatment group. In the ADSCs-treated group, the final failure load and stiffness were higher. They concluded that at the tendon-bone junction, local administration of ADSCs facilitated the early healing process.
Stem cell injection causes massive cell loss and a low rate of survival; the supply of MSCs in a hydrogel or scaffold will improve their productivity and help overcome these disadvantages. Lipneret al[109] used an aligned nanofibrous poly lactic coglycolic acid scaffold with a gradient in mineral content; this was seeded with ADSCs transduced with osteogenic factor BMP2 and implanted at the repair site of a rat rotator cuff model. They found that cells transmitted with BMP2 resulted in impaired healing and that this growth factor should not be used in the tendon-to-bone repair setting. Rothrauffet al[110] investigated the effect of ADSCs and TGF-β3 delivered in hydrogels on enthesis healing after rotator cuff tear repair in rats. They concluded that supplementing ADSCs with TGF-β3 had no added benefit. In a rat chronic rotator cuff injury model, Kaizawaet al[111] injected ADSCs-seeded tendon hydrogel, which is a type I collagen-rich gel derived from human tendons, at the repair site. They concluded that in a chronic rotator cuff injury model, tendon hydrogel augmentation with ADSCs does not substantially stimulate tendon bone interface healing. Shinet al[112] evaluated the effects of an ADSCs sheet for tendon-to-bone healing of a chronic rotator cuff tear in rats. Their laboratory research provides evidence that ADSCs are successful in repairing rotator cuff tears and that a clinically feasible stem cell delivery method for rotator cuff repair is engineered stem cells.
Although ADSCs have been effective in tendon-bone healing in many studies, the exact mechanism remains unclear. First, there are assumptions that ADSCs are capable not only of self-differentiation but also of promoting the differentiation of other endogenous stem cells by stimulating their recruitment along the appropriate lineage path[113]. Second, ADSCs can regulate biological processes such as cell proliferation,migration, differentiation, and deposition of the extracellular matrix, which can also be an important part of tendon healing through growth factors and cytokines. In addition, ADSCs can supply the isochemical site with antioxidant chemicals or freeradical scavengers to help remove toxic substances from torn tendons and musculoskeletal tissues and to promote cell recovery.
Clinical studies
Kimet al[114] determined the effect of an injection of ADSCs loaded in fibrin glue during arthroscopic rotator cuff repair on clinical outcomes. Among the 182 patients,35 underwent arthroscopic rotator cuff repairviathe injection of ADSCs loaded fibrin glue. Outcomes were measured using the VAS for pain, ROM, and functional measurements of the Constant score and UCLA shoulder rating scale. The repaired structural integrity of the tendon was assessed using MRI. The mean clinical follow-up period was 28 mo. The findings indicated that there were no significant differences between the groups at the final follow-up of the VAS score, the internal rotation at the back, the Constant score, and UCLA score. Forward flexion and external side rotation substantially improved in the final follow-up in both groups. In the control group,MRI showed a re-tear rate of 28.5% and 14.3% in the injection group. This study showed a major improvement for structural effects with respect to the re-tear rate when injecting ADSCs loaded fibrin glue during rotator cuff repair. However, there were no clinical differences in the 28-mo follow-up period. Eduardet al[115] then compared the healing and clinical effects of ACL reconstruction between patients with or without intraoperative ADSCs administration. They followed 20 soccer players who underwent ACL reconstruction using a bone-patellar tendon-bone autograft infiltrated with ADSCs. Outcomes were collected at baseline and 6 and 12 mo postoperatively for the International Knee Documentation Committee (IKDC) score, Lysholm knee score,VAS, and MRI. All patients had better outcomes and returned to playing sports after surgery. They concluded that it is not justified to improve cure or accelerate the functions after the reconstruction of ACL through the intraoperative administration of ADSCs at this point.
Currently, ADSCs are still rarely used for clinical research. The number of patients was relatively small, and the duration of follow-up was limited. There was no randomized controlled trial. To confirm the effect of using ADSCs in the reconstruction of ACL and rotator cuff healing, future studies with larger sample sizes will be necessary at different times.
PERIOSTEUM-DERIVED PSCS
Numerous studies have shown that the periosteum contains multipotent stem cells called periosteum-derived PSCs to differentiate osteogenic and chondrogenic tissues[116,117]. In 1930, Burmanet al[118] used a periosteal autograft to enhance bone formation around a tendon graft. The periosteum consists of two layers, the outer layer mainly includes fibroblasts with collagen fiber, and the inner layer contains mostly undifferentiated granular matrix precursor cells. Therefore, depending on whether the cambium side is positioned towards the bone or towards the tendon,when a periosteum patch is transplanted into the tendon-bone interface, the outcome will vary. In the last several years, multiple researchers have investigated whether a free periosteal graft would improve tendon healing in a bone tunnel, and whether periosteal fiber and enhancements can induce progress in tendon-bone healing.
Pre-clinical studies
Karaogluet al[119] compared the effect of enhancing the tendon-bone attachment between the periosteum and BMSCs and found that periosteum had a positive effect after 6 wk, whereas bone marrow was more effective after 12 wk. Younet al[120] tested the different efficacy levels between periosteal graft with the fibrous layer facing the bone and the cambium layer facing the bone wrapped around the tendon. Biomechanical testing demonstrated that the fresh cambium layer facing toward the bone group had a higher ultimate failure load than any other groups. A fluorescent histological assessment showed that the fresh cambium layer facing the bone group had the most organized and significant bone formation around the bone tunnel. They concluded that a periosteal augmentation of a tendon graft could enhance the structural integrity of the tendon-bone interface, when the periosteum is placed between the tendon and bone interface with the cambium layer facing toward the bone. In an extra-articular rabbit-bone tunnel model, Chenet al[121] examined the effect of the periosteum-enveloping tendon on tendon-bone healing. The findings revealed a fibrous layer that developed in the periosteum between the tendon and the bone. After 4 wk, the cancellous bone lining of the bone tunnel was interdigitized with the fibrous interface tissue. Progressive new bone grew into the interface fibrous layer after 8 wk. At 12 wk, collagen fibers had become anchored between the tendon and the bone and organized with the formation of fibrocartilage. In the periosteum-enveloped group, biomechanical tests have indicated a higher maximum pullout strength at all times. Their studies suggested that the periosteum sutured on the tendon transplanted into the bone tunnel in a superior healing process and better healing strength. Using a clinically relevant rabbit model of rotator cuff tear, then they[122] investigated the effect of the periosteum on the healing of the infraspinatus tendon and bone.Histological analysis showed that during the healing process, the cambium layer of the periosteum could be a potent interface layer which is progressively mature and structured, resulting in the formation of fiber cartilage and the eventual absorption of the disrupted tendon into the bone. The biomechanical tests showed that the attachment strength had improved gradually, demonstrating the progressive integration of tendon-bone.
Recently, tissue-engineered solutions to facilitate the integration of the tendon graft into the bone tunnel have been promising. Chenet al[123] injected photopolymerizable hydrogel based on poly(ethylene glycol) diacrylate (PEGDA) with hyaluronic acidtethered BMP-2 and PSCs into an extra-articular bone tunnel rabbit model. An interface fibrocartilage and new bone formed after 6 wk was examined histologically.At 3 and 6 wk after tendon transplantation, biomechanical studies revealed a greater maximum pullout strength and stiffness. Then they[124] used this injectable hydrogel made with PSCs and PEGDA tethered with BMP-2 in a rabbit model of rotator cuff tear. This study found that the tendon-bone interface had an expanded fibrocartilage and bone layer, with a maximum pull-out load at 4 and 8 wk. These studies demonstrated that PSC and PEGDA along with BMP-2, have a high inductive potential for healing between the tendon and the bone. Subsequently, they[125]developed a scaffold-free method using polymerized fibrin-coated dishes to make functional PSCs sheets. They evaluated the effect of bioengineered PSCs sheets in an extra-articular bone tunnel rabbit model. Histological staining showed that the tendonbone junction was formed with higher fibrocartilage at 4 wk. Matured fibrocartilage and dense collagen fiber were formed at the tendon-bone interface at 8 wk. At the same time, they[126] compared the effects of a PSCs sheet and acellular collagen sheet on tendon-bone healing in a rabbit ACL reconstruction model. After 8 wk, the PSCs sheet group had a higher collagen and glycosaminoglycan deposition at the tendon bone junction, with fibrocartilage formation. In addition, in comparison with the group of cellular collagen sheets, the PSCs sheet group exhibited significantly better mechanical performance. These two studies have concluded that the PSCs sheet has a high inductive potential for tendon and bone healing.
Although numerous studies have found that PSCs can improve tendon-bone healing, they have not recognized the impact of synovial fluid and physiological loading in their animal model of the extraarticular tendon-bone healing model.
Clinical studies
As the periosteum may represent a novel treatment modality for enhancing tendon–bone healing, this technique may be used in clinical practice for ACL reconstruction or rotator cuff repair to improve tendon graft healing inside the tunnel.Chenet al[127] used periosteum-enveloping hamstring tendon grafts in 62 patients who underwent ACL reconstruction. They were followed for a minimal of 2 years.Clinical assessments included the Lysholm knee scores, IKDC scores, KT-1000 instrumented testing, thigh muscle assessment, and radiographic evaluation. All patients showed a higher Lysholm knee score at the end of follow-up; 92% of patients had a normal or almost normal IKDC score; 6% of patients were found to have grade 2 or more ligament laxity. Forty-six patients achieved recovery of the extensor muscle strength in the reconstructed knee to 90% or more of normal knee strength.Radiographic evaluation found that a rise of more than 1 mm was identified in three(5%) femoral tunnels and four (6%) tibial tunnels in five of 62 patients. After reconstruction, 81% of patients were able to return to moderate or strenuous activity.A few years later, this group[128] used single-bundle ACL reconstruction with periosteum-enveloping hamstring tendon grafts on 368 patients. Those patients were followed for an average of 4.6 years. There have been similar findings which led to the conclusion that the periosteum-enveloping hamstring tendon graft in ACL rebuilding would achieve a satisfactory outcome.
The clinical and radiological outcomes of open rotator cuff reconstruction were then examined by Scheibelet al[129] in 23 patients with a mean follow-up period of 14.4 mo,using an autologous periosteal flap augmentation technique. The Constant-Score rose dramatically and a significant positive result was yielded by the Simple Shoulder test.In postoperative MRI, only four (20%) patients displayed a re-tear of the tendon. They concluded that the autologous periosteal flap in the open rotator cuff repair has a high patient level of satisfaction with low re-rupture rates.
Although these studies have achieved satisfactory results, they were performed as prospective studies with fewer samples and a shorter follow-up time. In the future, it will be necessary to compare and further evaluate the potential benefits of periosteal improvements in ACL or rotator cuff healing in clinical prospective randomized trials with large samples.
STEM CELLS DERIVED FROM ACL TISSUES
The existence of MSC–like cells in human ACL tissues has been discovered recently.Matsumotoet al[130] first isolated vascular stem cells with characteristic expression of CD34 in the injured ACL tissues in 2012. They demonstrated that ACL ruptured tissue contained abundant CD34-positive cells (44.3%) compared with intact ACL tissue(8.3%), and CD34-positive cells exhibited multilineage differentiation capacities,including the ability to undergo chondrogenesis, osteogenesis, adipogenesis, and endotheliogenesis. The canine ACL reconstruction model was then used to demonstrate that ACL injured tissue has the therapeutic potential to foster a suitable environment for tendon-to-bone healing in bone tunnels of ACL reconstruction[131].
Mifuneet al[132] injected CD34+ stem cells derived from adult human ACL into the articular cavity in nude rats after ACL reconstruction in the same year. A greater area of collagen fiber formation and more collagen type II expression in the CD34+ group were revealed by a histological evaluation. The immunostaining study showed that CD34+ stem cells derived from ACL had a greater capacity to differentiate into endothelial cells and osteoblasts. After the treatment of CD34+ cells, the biomechanical test showed the failure load to exhibit almost the same strength as the uninjured ACL.Subsequently, they advanced the study by using a cell sheet wrapped graft with ACLderived CD34+ cells in a nude rat ACL reconstruction model, which also exhibited promising healing potential[133].
Although some studies have already proven that ACL-derived CD34-positive cells contribute to tendon-bone healing after ACL reconstruction, the relationship between the healing potential of ACL-derived cells and the patient’s age or elapsed time after injury remains uncertain. Nakanoet al[134] injected ACL-derived CD34+ stem cells from patients aged 10 to 19 years (younger group) or patients aged 30 to 39 years(older group) into the ACL reconstruction model of immunodeficient rats. A significantly higher ultimate load to failure rate and a greater ability of differentiation into endothelial cells and osteoblasts were observed in the younger group. They also demonstrated that in the immunodeficient rat model of ACL reconstruction, ACLderived cells from young patients would have a greater effect on the maturation of tendon-bone integration compared to cells from older patients. A few years later,Inokuchiet al[135] harvested ACL-derived CD34+ stem cells from two groups of patients, namely, an early group (≤ 3 mo after injury) and a chronic group (≥ 3 mo after injury), based on the time that elapsed between injury and surgery. They then tested the influence of elapsed time after injury on the healing process in an immunodeficient rat model of ACL reconstruction; they concluded that cells obtained during the early phase after injury have a higher tendon-bone healing potential compared to human ACL-derived cells obtained during the chronic phase.
Recent studies have conducted the genetic modification of stem cells derived from ACL. A cell sheet-wrapped graft with ACL-derived CD34+ cells expressing either VEGF or soluble FLT-1 was used by Takayamaet al[136] in the ACL reconstruction model of nude rats. It was concluded that the indigenous expression of VEGF in the CD34+ cells improved tendon graft maturation and biomechanical strength, but that the overexpression of VEGF prevented improvements in biomechanical strength.Kawakamiet al[137] used adult human ACL-derived CD34+ cells transduced with BMP-2 in a rat model, and demonstrated that ACL-derived CD34+ cells transduced with BMP-2 accelerated graft-bone integration after ACL reconstruction, as evidenced by the enhanced histological appearance and graft-bone interface biology along with tensile load to failure.
Although current research has shown that ACL-derived CD34+ cells contributed to the tendon-bone healing after ACL reconstruction by enhancing angiogenesis and osteogenesis after ACL reconstruction, which also enhances biomechanical strength[132,133], clinical trials are not yet available, and some limitations remain. First, rats have a higher healing ability than humans, so the grafting progress of tendon healing in rats is likely to advance faster than in humans. Second, current studies have not indicated whether stem cells derived from ACL could differentiate into fibroblasts to directly contribute to the graft tendon healing[132]. Second-step arthroscopic surgery is inevitable due to the need for cell isolation, cell culture, and cell expansion when cell therapy is applied for ACL reconstruction, thereby affecting the clinical viability of CD34+ cell transplantation[131]. More experiments are necessary to confirm its clinical viability and the actual mechanisms of this application in a larger animal model must be further investigated.
LIMITATIONS OF STEM CELL THERAPY AND DIRECTIONS FOR FUTURE RESEARCH
Despite the promising consequences of stem cell therapy, there are quite a few limitations. The most widely used methods to move stem cells into the bone tunnel are direct intra-articular injection; thus cell leakage is inevitable. In tendon and bone healing implant MSCs, the biological process is unclear and needs to be further clarified. For gene therapy, one of the key drawbacks is the decline in gene expression after several weeks, which could result in the loss of the desired product. Moreover,there is no guarantee regarding the safety of gene therapy, as mutagenesis,malignancy, and other side-effects may occur. Based on animal research, the shortterm impact of stem cell therapy has been reasonably successful. However, there is still no long-term impact or confirmation based on human studies.
Regarding the clinical applications, the dosage and duration of stem cell therapy have not been achieved to ensure the best result. A two-stage arthroscopic surgery is inevitable for a sufficient number of autologous stem cells, which will result in unnecessary pain and costs. It is important to develop a more effective and cheaper surgical strategy. Most stem cell therapy trials are focused on small animal models,which have a higher rate of tendon-bone healing than in human patients. To prove its clinical viability, further studies to test the efficacy of this application in large animal models are needed. In addition to the effectiveness of repair and regeneration of stem cells, it is important to properly assess possible hazards or adverse events, such as carcinogenesis, prior to clinical use.
CONCLUSION
MSCs may be particularly useful for stem cell-based therapies for several reasons.First, MSCs of different mesenchymal tissues have been insulated, including bone marrow, muscle, circulatory blood, blood vessels, and fat[138]. Second, MSCs can be differentiated into various cell types, such as osteoblasts, chondrocytes, and adipocytes[139]. This indicates that relative to other adult stem cells, MSCs could have broader therapeutic applications. Third, implanted BMSCs extend into ligament fibroblast and cell fibrocartilage, which leads to fibrocartilage accumulation. Forth, MSCs exert strong paracrine effects, boosting the ability of tissue damage to self-repair.
Moreover, the fibrocartilage interface is also derivative of local cells, and injected MSCs can secrete various growth factors to promote local fibroblast and fibro-cartilage cell activation and recruitment.
In conclusion, the acceleration of tendon-bone healing has proven to be successful for many types of stem cells. MSCs, due to their high rate of proliferation, multipower,and relative ease of separation from diverse tissues, are highly appealing for the promotion of tendon-bone junction healing. However, these findings were yielded under restricted conditions and clinical evidence. In future trials, numerous issues,including application requirements and technological and safety problems, must be addressed prior to clinical application. Meanwhile, research on the biological healing mechanism of the stem cells implanted for tendon-to-bone healing is also required.
杂志排行
World Journal of Stem Cells的其它文章
- Epigenetic modulators for brain cancer stem cells: Implications for anticancer treatment
- Mechanisms involved in selecting and maintaining neuroblastoma cancer stem cell populations, and perspectives for therapeutic targeting
- Roles of mitochondrial unfolded protein response in mammalian stem cells
- Exosomal microRNAs from mesenchymal stem/stromal cells:Biology and applications in neuroprotection
- Immunotherapy against programmed death-1/programmed death ligand 1 in hepatocellular carcinoma: Importance of molecular variations, cellular heterogeneity, and cancer stem cells
- Bone marrow mononuclear cells for joint therapy: The role of macrophages in inflammation resolution and tissue repair
