纳布啡预防性镇痛对妇科腹腔镜手术患者术后早期疼痛的影响
2021-03-24王慧珊贺翠莲
王慧珊 贺翠莲


【摘要】 目的:研究不同剂量纳布啡预防性镇痛在妇科腹腔镜手术中应用对术后早期疼痛的影响。方法:选择2019年7月-2020年10月包头市中心医院120例行妇科腹腔镜手术的患者。采用随机数字表法将其分为NS组、N1组、N2组、N3组,每组30例。术毕前30 min,NS组、N1组、N2组、N3组分别静脉注射0.9%氯化钠溶液、0.1 mg/kg纳布啡、0.2 mg/kg纳布啡、0.3 mg/kg纳布啡。比较四组呼吸恢复、苏醒和拔管时间及不良反应发生情况,比较四组舒芬太尼泵入容量和PCIA泵按压次数,比较四组MAP、HR、SpO2、Glu、Cor及VAS评分。结果:T0时,四组MAP、HR、Glu、Cor和SpO2比較,差异均无统计学意义(P>0.05)。T1时,NS组、N1组的MAP、HR、Glu、Cor较T0时升高,差异均有统计学意义(P<0.05)。N2组、N3组T0与T1时的MAP、HR、Glu、Cor比较,差异均无统计学意义(P>0.05)。T1时,四组SpO2低于T0时,差异有统计学意义(P<0.05),均大于98%。T1时,四组MAP、HR、Glu、Cor比较,差异均有统计学意义(P<0.05);NS组、N1组的MAP、HR和Glu均高于N2组、N3组,Cor为NS组>N1组>N2组、N3组,差异均有统计学意义(P<0.05)。T1时,四组SpO2比较,差异无统计学意义(P>0.05)。T2~T5时,四组VAS评分比较,差异均有统计学意义(P<0.05)。T2、T3时NS组VAS评分均高于N1组、N2组、N3组,差异均有统计学意义(P<0.05)。T4、T5时,NS组、N1组VAS评分均高于N2组、N3组,差异均有统计学意义(P<0.05)。T4时,NS组VAS评分高于T2时;T5时,NS组VAS评分高于T2、T3时,差异均有统计学意义(P<0.05)。N1组VAS评分比较为T4、T5时>T3时>T2时,差异均有统计学意义(P<0.05)。T2~T5时,N2组、N3组VAS评分比较,差异均无统计学意义(P>0.05)。四组舒芬太尼泵入容量和PCIA泵按压次数比较,差异均有统计学意义(P<0.05),且NS组、N1组均高于N2和N3组,差异均有统计学意义(P<0.05)。四组患者呼吸恢复、苏醒和拔管时间比较,差异均无统计学意义(P>0.05)。四组均未出现皮肤瘙痒和呼吸抑制。四组恶心呕吐、寒战发生率比较,差异均无统计学意义(P>0.05)。结论:妇科腹腔镜手术结束前30 min给予纳布啡0.2~0.3 mg/kg不延长呼吸恢复时间、苏醒时间及拔管时间,血流动力学和应激化验指标更平稳,提高了患者麻醉苏醒质量,提供了完善的术后早期镇痛且不增加不良反应。
【关键词】 纳布啡 腹腔镜手术 苏醒期 镇痛
[Abstract] Objective: To study the effect of different doses of Nalbuphine preventive analgesia on early postoperative pain in patients underwent gynecological laparoscopic surgery. Method: A total of 120 patients underwent gynecological laparoscopic surgery in Baotou Central Hospital from July 2019 to October 2020 were selected, they were randomly divided into NS group, N1 group, N2 group and N3 group according to random number table method, 30 cases in each group. 30 min before the surgery, NS group, N1 group, N2 group and N3 group were injected intravenously with 0.9% Sodium Chloride Solution, 0.1 mg/kg Nalbuphine, 0.2 mg/kg Nalbuphine and 0.3 mg/kg Nalbuphine, respectively. The time of respiratory recovery, recovery and extubation and the occurrence of adverse reactions were compared among the four groups. The pumping capacity of Sufentanil and the number of pump compressions of PCIA were compared among the four groups, the MAP, HR, SpO2, Glu, Cor and VAS scores were compared among four groups. Result: At T0, there were no significant differences in MAP, HR, Glu, Cor and SpO2 among four groups (P>0.05). At T1, MAP, HR, Glu and Cor in the NS group and N1 group were higher than those at T0, the differences were statistically significant (P<0.05). There were no significant differences in MAP, HR, Glu and Cor between T0 and T1 in the N2 group and N3 group (P>0.05). At T1, SpO2 in the four groups were lower than those at T0, and the differences were statistically significant (P<0.05), and all of them were greater than 98%. At T1, there were significant differences in MAP, HR, Glu and Cor among four groups (P<0.05); MAP, HR and Glu in the NS group and N1 group were higher than those in the N2 group and N3 group, and Cor was NS group > N1 group > N2 group and N3 group, the differences were statistically significant (P<0.05). At T1, there was no significant difference in SpO2 among four groups (P>0.05). T2~T5, there were significant differences in VAS scores among four groups (P<0.05). At T2 and T3, VAS scores in the NS group were higher than those in the N1 group, N2 group and N3 group, the differences were statistically significant (P<0.05). At T4 and T5, VAS scores in the NS group and N1 group were higher than those in the N2 group and N3 group, the differences were statistically significant (P<0.05). At T4, VAS score in the NS group was higher than that at T2; VAS score of NS group at T5 was higher than those at T2 and T3, and the differences were statistically significant (P<0.05). VAS scores in the N1 group were compared as T4, T5 > T3 > T2, the differences were statistically significant (P<0.05). T2-T5, there were no significant differences in VAS scores between N2 group and N3 group (P>0.05). There were statistically significant differences in pumping capacity of Sufentanil and the number of pump compressions among four groups (P<0.05), and those in the NS group and N1 group were higher than those in the N2 group and N3 group, and the differences were statistically significant (P<0.05). There were no significant differences in respiratory recovery, recovery and extubation time among four groups (P>0.05). Skin pruritus and respiratory depression were not found in four groups. There were no significant differences in the incidence of nausea, vomiting and chills among four groups (P>0.05). Conclusion: The administration of Nalbuphine 0.2-0.3 mg/kg 30 min before the end of gynecological laparoscopic surgery do not prolong the respiratory recovery time, recovery time and extubation time, the hemodynamics and stress test indexes are more stable, the quality of anesthesia recovery is improved, and the early postoperative analgesia is provided without increasing adverse reactions.
[Key words] Nalbuphine Laparoscopic surgery Recovery period Analgesia
First-author’s address: Central Clinical Medical College of Baotou Medical College, Baotou 014040, China
doi:10.3969/j.issn.1674-4985.2021.25.005
全麻蘇醒质量不佳直接影响患者的生命安全、能否安全平稳地过渡,是影响手术及预后的关键。围术期的特殊因素都会促成术后疼痛的发生,因此,最好的方法是阻断从组织创伤到伤口愈合整个过程中疼痛信号的传递。超前镇痛不应只强调手术前干预治疗,而应包括整个伤害性刺激过程,预防性镇痛是近年来提出的一种新型镇痛概念[1-2]。纳布啡是一种廉价的、非控制性的阿片类止痛剂,已在临床上使用了数十年。作为κ阿片受体激动剂和µ阿片受体部分拮抗剂,纳布啡比其他阿片类止痛药产生的不良反应更少,可改善躯体和内脏疼痛[3]。本课题主要针对手术中(妇科腹腔镜手术术毕前30 min)予以静脉注射不同剂量的纳布啡,进而观察其对术后早期疼痛的影响。
1 资料与方法
1.1 一般资料 选择2019年7月-2020年10月包头市中心医院妇科腹腔镜手术患者120例。纳入标准:(1)拟择期腹部妇科腔镜手术;(2)ASA分级Ⅰ、Ⅱ级;(3)年龄18~65岁;(4)体重指数(BMI)18~25 kg/m2;(5)术前无贫血。排除标准:(1)上气道解剖异常;(2)肺功能障碍;(3)已确诊的OSAHS;(4)合并肝肾疾病、心脑血管病;(5)术前有慢性疼痛病史或长期服用镇痛药(阿片类药物、非甾体抗炎药、镇静药或抗抑郁药等);(6)术前合并神经系统疾病、精神病史;(7)术前48 h内服用过镇静镇痛药;(8)对研究药物过敏。采用随机数字表法将患者分为NS组、N1组、N2组和N3组,每组30例。本研究为随机对照双盲设计,经医院伦理委员会批准并和患者签署知情同意书。
1.2 方法 四组患者麻醉前均未用术前药,均禁食8 h,禁水6 h,入室后建立静脉通路,无创监测BP、HR、ECG、SpO2。静脉注射咪达唑仑0.04 mg/kg(生产厂家:江苏恩华药业股份有限公司,批准文号:国药准字H10980025,规格:2 mL∶10 mg),舒芬太尼0.4 μg/kg(生产厂家:宜昌人福药业有限责任公司,批准文号:国药准字H20054171,规格:1 mL∶50 μg),丙泊酚1.5 mg/kg(生产厂家:西安立邦制药有限公司,批准文号:国药准字H19990282,规格:20 mL∶0.2 g),罗库溴铵0.6 mg/kg(生产厂家:浙江仙琚制药股份有限公司,批准文号:国药准字H20093186,规格:5 mL∶50 mg)麻醉诱导,待麻醉诱导效果满意直视下插入气管导管,并进行机械通气。VT 8 mL/kg,维持呼气末二氧化碳分压(PetCO2 35~45 mmHg),腹腔镜手术期间腹腔人工气压维持在13 mmHg(1 mmHg=0.133 kPa),以丙泊酚4~6 mg/(kg·h)、瑞芬太尼0.1~0.2 μg/(kg·min)(生产厂家:宜昌人福药业有限责任公司,批准文号:国药准字H20030197,规格:1 mg)持续泵入维持麻醉,维持生命体征平稳,根据手术进程必要时给予罗库溴铵0.15 mg/kg。NS组、N1组、N2组、N3组,术毕前30 min分别静脉注射0.9%氯化钠溶液、0.1 mg/kg纳布啡、0.2 mg/kg纳布啡、0.3 mg/kg纳布啡。纳布啡(生产厂家:宜昌人福药业有限责任公司生产,批准文号:国药准字H20130127,规格:2 mL∶20 mg)。缝合皮肤前对患者停止使用麻醉药。予以新斯的明0.04 mg/kg(生产厂家:河南润弘制药股份有限公司,批准文号:国药准字H41022269,规格:1 mL∶0.5 mg),阿托品0.02 mg/kg(生产厂家:天津金耀药业有限公司生产,批准文号:国药准字H12020382,规格:1 mL∶0.5 mg)拮抗肌松,待患者自然苏醒,达到拔管指征拔除气管导管。送PACU观察30 min,记录不良反应发生情况,予以PCIA泵,配药2 μg/kg舒芬太尼加生理盐水至100 mL,输注背景设置为输注速度2 mL/h,单次给药量0.5 mL,锁时10 min。若生命体征平稳,送回妇科术后病房。
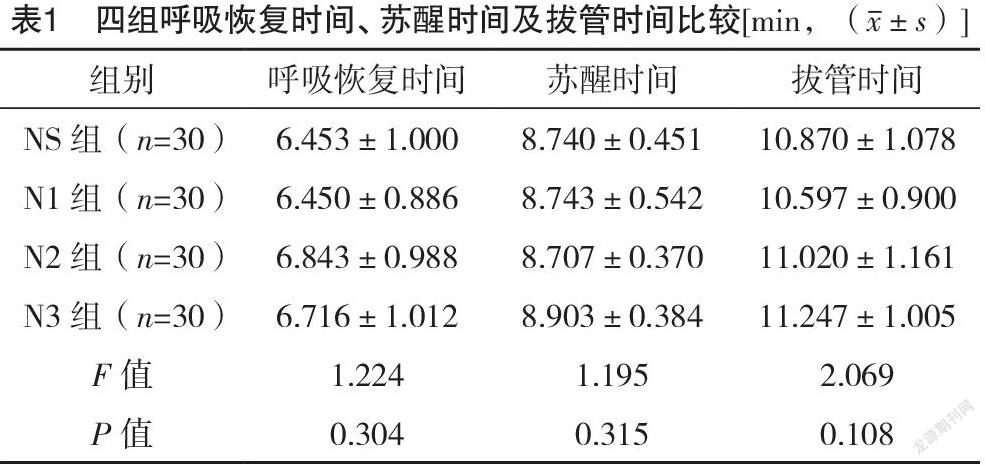
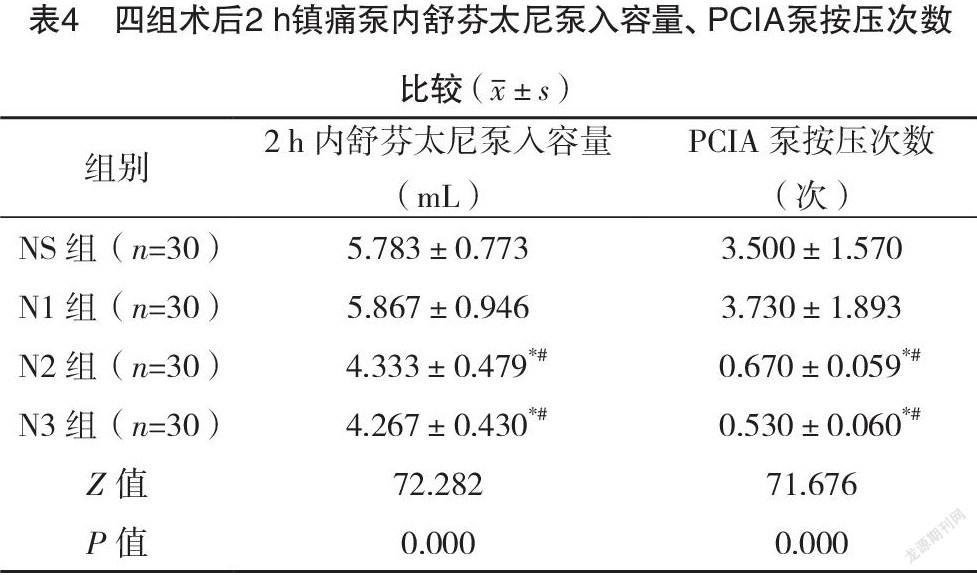
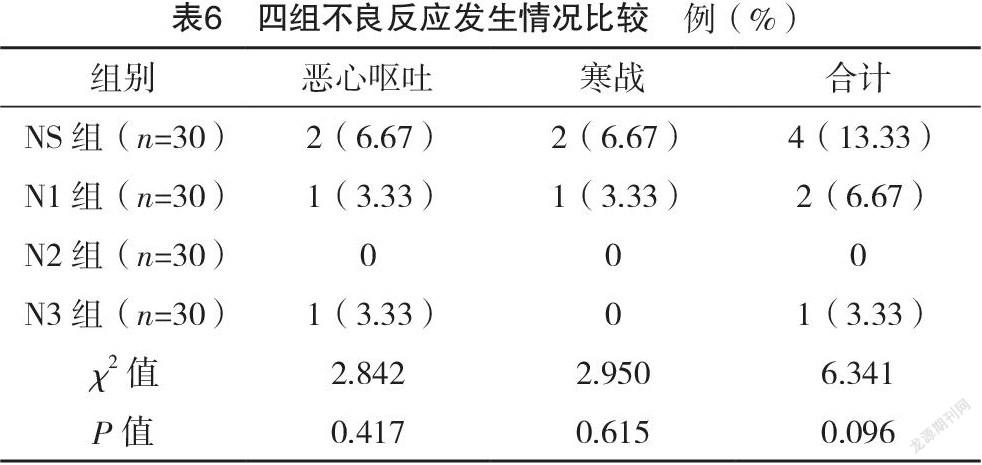
1.3 观察指标 (1)比较四组呼吸恢复时间、苏醒时间、拔管时间。(2)比较四组给药前(T0)、拔管后5 min(T1)时的HR、MAP、SpO2。(3)比较四组应激化验指标。T0、T1时血糖(Glu)、皮质醇(Cor)。(4)比较四组术后2 h的舒芬太尼泵入容量、PCIA泵按压次数。(5)比较四组术后15 min(T2)、术后30 min(T3)、术后1 h(T4)、术后2 h(T5)时VAS评分;(6)比较四组不良反应发生情况。包括呼吸抑制、恶心呕吐、寒战、皮肤瘙痒。
1.4 统计学处理 采用SPSS 26.0软件对所得数据进行统计分析,计量资料用(x±s)表示,组内比较采用配对t检验,多组间比较采用F检验,组间两两比较用独立样本t检验;计数资料以率(%)表示,比较采用字2检验。以P<0.05为差异有统计学意义。
2 结果
2.1 四组一般资料比较 NS组年龄27~60岁,平均(50.6±8.7)岁;BMI(22.2±2.2)kg/m2;ASAⅠ级8例,Ⅱ级22例。N1组年龄24~64岁,平均(46.8±10.7)岁;BMI(21.9±2.4)kg/m2;ASAⅠ级6例,Ⅱ级24例。N2组年龄32~62岁,平均(48.8±7.6)岁;BMI(21.8±2.3)kg/m2;ASAⅠ级5例,Ⅱ级25例。N3组年龄28~65岁,平均(47.9±8.0)岁;BMI(21.8±2.3)kg/m2;ASAⅠ级10例,Ⅱ级20例。四组一般资料比较,差异均无统计学意义(P>0.05),具有可比性。
2.2 四组呼吸恢复时间、苏醒时间及拔管时间比较 四组呼吸恢复时间、苏醒时间、拔管时间比较,差异均无统计学意义(P>0.05),见表1。
2.3 四组T0、T1时MAP、HR、SpO2比较 T1时,NS组、N1组的MAP、HR均高于T0时,差异均有统计学意义(P<0.05)。T1时,N2组、N3组的MAP、HR与T0比较,差异均无统计学意义(P>0.05)。T1时,四组SpO2均低于T0时,差异均有统计学意义(P<0.05),均大于98%。T0时,四组MAP、HR、SpO2比较,差异均无统计学意义(P>0.05)。T1时,四组MAP、HR比较,差异均有统计学意义(P<0.05);NS组、N1组的MAP、HR均高于N2组、N3组,差异均有统计学意义(P<0.05)。T1时,四组SpO2比较,差异均无统计学意义(F=0.052,P=0.984)。见表2。
2.4 四组T0、T1时Glu、Cor比较 T0时,四组Glu、Cor比较,差异均无统计学意义(P>0.05)。T1时,NS组、N1组的Glu、Cor均高于T0时,差异均有统计学意义(P<0.05)。T1时,N2、N3组的Glu、Cor与T0比较,差异均无统计学意义(P>0.05)。T1时,N2、N3组的Glu、Cor低于对照NS、N1组;NS组的Cor>N1组>N2、N3组,差异均有统计学意义(P<0.05)。见表3。
2.5 术后2 h镇痛泵内舒芬太尼泵入容量、镇痛泵按压次数比较 四组舒芬太尼泵入容量和PCIA泵按压次数比较,差异均有统计学意义(P<0.05),且NS组、N1组均高于N2和N3组,差异均有统计学意义(P<0.05)。见表4。
2.6 四组VAS评分比较 T2~T5时,四组VAS评分比较,差异均有统计学意义(P<0.05)。T2、T3时,NS组VAS评分均高于N1、N2、N3组,差异均有统计学意义(P<0.05)。T3时,N1组VAS评分高于T2时,差异有统计学意义(P<0.05)。T4、T5时,NS组、N1组VAS评分均高于N2组、N3组,差异均有统计学意义(P<0.05)。T5时,NS组VAS评分高于T2、T3时;T4时高于T2时,差异均有统计学意义(P<0.05)。N1组VAS评分T4、T5时>T3时>T2时,差异均有统计学意义(P<0.05)。T2~T5时,N2组、N3組VAS评分比较,差异均无统计学意义(P>0.05)。见表5。
2.7 四组不良反应发生情况比较 四组均未出现皮肤瘙痒和呼吸抑制。四组恶心呕吐、寒战发生率比较,差异均无统计学意义(P>0.05)。见表6。
3 讨论
全麻苏醒期是患者由麻醉减浅向清醒过渡的关键时期,受手术麻醉等多方面因素的共同影响,血流动力学剧烈波动、通气不足、应激、躁动等都是苏醒期可能发生的并发症,疼痛是引起以上并发症的主要原因[4-5]。瑞芬太尼由于其对剂量的控制效果较好,现广泛用于麻醉维持[6]。但停药后镇痛作用消除快可能诱发痛觉过敏,引起爆发性疼痛,手术结束前给予阿片类药物往往被用来解决此问题[7-8]。然而关于瑞芬太尼所致痛敏的确切易感患者群体,预防或给药策略依然无确凿证据,且应用亚麻醉剂量的长效阿片类药物最常见的不良反应是延迟性呼吸抑制,很大程度上限制了此种方法的使用[9-10]。纳布啡作为κ阿片受体激动剂和部分µ阿片受体拮抗剂,尽管它可导致呼吸抑制,但具有天花板效应,且由于其对µ阿片受体的拮抗作用,它可以拮抗其他阿片类药物的呼吸抑制作用,同时增加这些药物的镇痛活性[11-14]。在刘菊等[14]的研究中,证实在妇科腹腔镜手术术毕静脉注射纳布啡可减少阿片类药物引起的呼吸抑制。纳布啡静脉注射后起效时间为2~3 min,药效达峰时间为30 min,作用时间为3~6 h[15-16]。需要在临床用药时把握好用药时机、用药剂量。本研究是在理论基础上,手术结束前30 min静脉予以不同剂量的纳布啡,探讨其是否可以作为瑞芬太尼衔接性用药,使镇痛效益最大化,同时在不引起呼吸抑制的基础上可否具有更平稳的血流动力学、减少应激和不良反应,平稳安全度过苏醒期是本课题研究的初衷。
本研究示,手术结束前给予0.1、0.2、0.3 mg/kg纳布啡均不延长呼吸恢复时间、苏醒时间及拔管时间,0.2、0.3 mg/kg血流动力学和应激化验指标在拔管后5 min较生理盐水和0.1 mg/kg更平稳,0.1、0.2、0.3 mg/kg术后15、30 min较对照组镇痛效果更好,但从术后1、2 h的VAS评分及舒芬太尼总用量和PCIA泵按压次数上来看,0.2、0.3 mg/kg更能够减少术后早期疼痛且不增加不良反应,较0.1 mg/kg效果更佳。
但值得注意的是文献[17-18]研究还证明纳布啡的镇痛有性别偏向性,对于女性的镇痛作用强于男性。一项荟萃分析结果表明,男性和女性对阿片类药物止痛的反应可能不同,但这些差异和相似之处明显受到多方面因素的影响,混合作用阿片类药物作用的性别差异可能是由于µ受体或κ受体活性不同所致[19-20]。本课题为妇科腹腔镜手术患者均为女性,可能存在性别偏倚影响。
综上所述,妇科腹腔镜手术结束前30 min给予纳布啡0.2~0.3 mg/kg不延长呼吸恢复时间、苏醒时间及拔管时间,血流动力学和应激化验指标更平稳,提高了患者麻醉苏醒质量,提供了完善的术后早期镇痛且不增加不良反应。
参考文献
[1]张倩,尤浩军.“超前镇痛”研究进展及麻醉中应用[J].中国疼痛医学杂志,2016,22(4):241-244.
[2] Luo J,Min S.Postoperative pain management in the postanesthesia care unit:an update[J].Pain Res,2017,10:2687-2698.
[3]於桥,陈春.盐酸纳布啡的特点及临床应用现状[J].中国医药导报,2017,14(28):38-41.
[4]廖礼平,王曙红.全身麻醉术后患者苏醒期并发症发生情况调查分析[J].护理学杂志,2016,31(2):61-63.
[5]耿武军,唐红丽,黄乐丹,等.地佐辛注射液对全麻苏醒期躁动及疼痛的影响[J].解放军医学杂志,2012,37(5):508-510.
[6] Cristina S,Alberto N,Claudia C,et al.Remifentanil-induced postoperative hyperalgesia:Current perspectives on mechanisms and therapeutic strategies[J].Local & Regional Anesthesia,2018,11:15-23.
[7]邓立琴,张丽华,辛婧媛.丁丙诺啡超前镇痛对瑞芬太尼诱发大鼠炎性痛觉过敏的影响[J].中国疼痛医学杂志,2013,19(11):675-678.
[8]卢钊楷,谭素云,王智钧.不同剂量右美托咪定联合帕瑞昔布钠在瑞芬太尼诱发术后痛觉过敏的预防研究[J].中国医学创新,2020,17(19):59-64.
[9] Yu E H,Tran D H,Lam S W,et al.Remifentanil tolerance and hyperalgesia:short-term gain,long-term pain?[J].Anaesthesia,2016,71(11):1347-1362.
[10]梁晓南.芬太尼致呼吸抑制的可能机制研究[D].北京:军事科学院,2019.
[11] Deng C,Wang X,Zhu Q,et al.Comparison of nalbuphine and sufentanil for colonoscopy:a randomized controlled trial[J/OL].PLoS One,2017,12(12):e0188901.
[12] Schmidt W K,Tam S W,Shotzberger G S,et al.Nalbuphine[J].Drug & Alcohol Dependence,1985,14(3):339-362.
[13]鄧煜锋,袁天柱.纳布啡多模式镇痛在胸腔镜肺叶切除术中的镇痛研究进展[J/OL].中西医结合心血管病电子杂志,2018,6(29):135-136.
[14]刘菊,郭鹏,王刚.不同剂量纳布啡联合舒芬太尼对妇科腹腔镜手术患者呼吸及镇痛的影响[J].医学综述,2020,26(5):1021-1026.
[15] Chmielnicki Z.Nalbuphine-properties and clinical use[J].Wiad Lek,1993,46(3-4):139-142.
[16]张振,罗辉宇,刘颖.纳布啡对老年患者全麻苏醒期应激反应和躁动的影响[J].中国新药与临床杂志,2017,36(12):740-743.
[17] Gear R W,Miaskowski C,Gordon N C,et al.Kappa-opioids produce significantly greater analgesia in women than in men[J].Nature Medicine,1996,2(11):1248-1250.
[18] Gear R W,Gordon N C,Hossaini-Zadeh M,et al.A Subanalgesic Dose of Morphine Eliminates Nalbuphine Anti-Analgesia in Postoperative Pain[J].Journal of Pain,2008,9(4):337-341.
[19] Claudia Pisanu,Flavia Franconi,Gian Luigi Gessa,et al.Sex differences in the response to opioids for pain relief:A systematic review and meta-analysis[J].Pharmacological Research,2019,148:104447.
[20] Craft R M,Mcniel D M.Agonist/antagonist properties of nalbuphine, butorphanol and (-)-pentazocine in male vs. female rats[J].Pharmacol Biochem Behav,2003,75(1):235-245.
(收稿日期:2020-12-14) (本文编辑:张明澜)