Non-operative management of pancreatic trauma in adults
2021-01-07NdiMtisSnthlingmJegtheeswrnVinothNdrjhAliSheenSurbhJmdrAjithSiriwrden
Ndi Mtis , Snthlingm Jegtheeswrn , Vinoth Ndrjh , b , Ali J. Sheen , c , d ,Surbh Jmdr , c , Ajith K. Siriwrden , c , *
a Regional Hepato-Pancreato-Biliary Surgery Unit, Manchester Royal Infirmary, Oxford Road, Manchester M13 9WL, UK
b Department of Radiology, Manchester Royal Infirmary, Manchester, UK
c Faculty of Biology, Medicine and Health, University of Manchester, Manchester, UK
d Manchester Metropolitan University, Manchester, UK
TotheEditor:
Pancreatic trauma accounts for 0.4% - 2.0% of all trauma-related injuries worldwide [1-3] . The American Association for the Surgery of Trauma (AAST) categorizes pancreatic injury according to the severity [4] . Pancreatic injury involving transection of the gland(grades III to V) typically requires surgical management [4] . However, pancreatic trauma, especially in children and young adults,can be managed without surgery [5] . This study reports the outcome of a policy of preferential non-operative management of pancreatic trauma in adults.
Between 2015 and 2019, patients presenting with pancreatic trauma to a specialist Hepato-Pancreato-Biliary (HPB) centre were identified from hospital databases. Patients were admitted with a spectrum of civilian trauma injuries to a centre serving an industrialized conurbation of 3.2 million people. This study takes the form of a retrospective analysis of a case cohort. Chart review (including review of computed tomography images) was undertaken to assess the severity of injury, management and outcome. The study was registered as an audit with Manchester University National Health Service Foundation Trust (audit number 7161).
There were 20 patients with pancreatic trauma during this study period. Thirteen (65%) were male. The median (range) age was 22 (2-65) years. Ten (50%) patients were children below 18 years of age. Sixteen (80%) sustained blunt trauma while four(20%) had penetrating trauma. AAST grade of pancreatic injury is presented in Table 1 together with information on associated extra-pancreatic injuries. Overall, 13 (65%) were managed nonoperatively. One of the 7 patients with grade I pancreatic injury required surgery for non-pancreatic injuries ( Table 2 ). Three (15%)underwent pancreatectomy and all of these patients had either grade III or IV injuries. Three further patients required laparotomy and intervention for non-pancreatic injury in the presence of grade III or IV pancreatic injury respectively. Late endoscopic interven-tion either for bleeding or for pancreatic collection was required in 3 (15%) and 3 patients (15%) required radiological intervention.There were no in-hospital or 90-day deaths. As with other singleinstitution datasets this is a small series of patients but the findings add to the body of evidence on non-surgical management of pancreatic injury. The results demonstrate that overall, a selective non-operative policy of management of pancreatic trauma is associated with acceptable outcomes. Patients with grade I and II injury can generally be managed without surgery. When there is transection of the gland (grade III) and above, non-operative management may be feasible in hemodynamically stable patients but accepting a likely requirement for subsequent radiological or endoscopic intervention. As the severity of pancreatic injury increases,so does the likelihood of associated extra-pancreatic injury, and the chance of surgery.
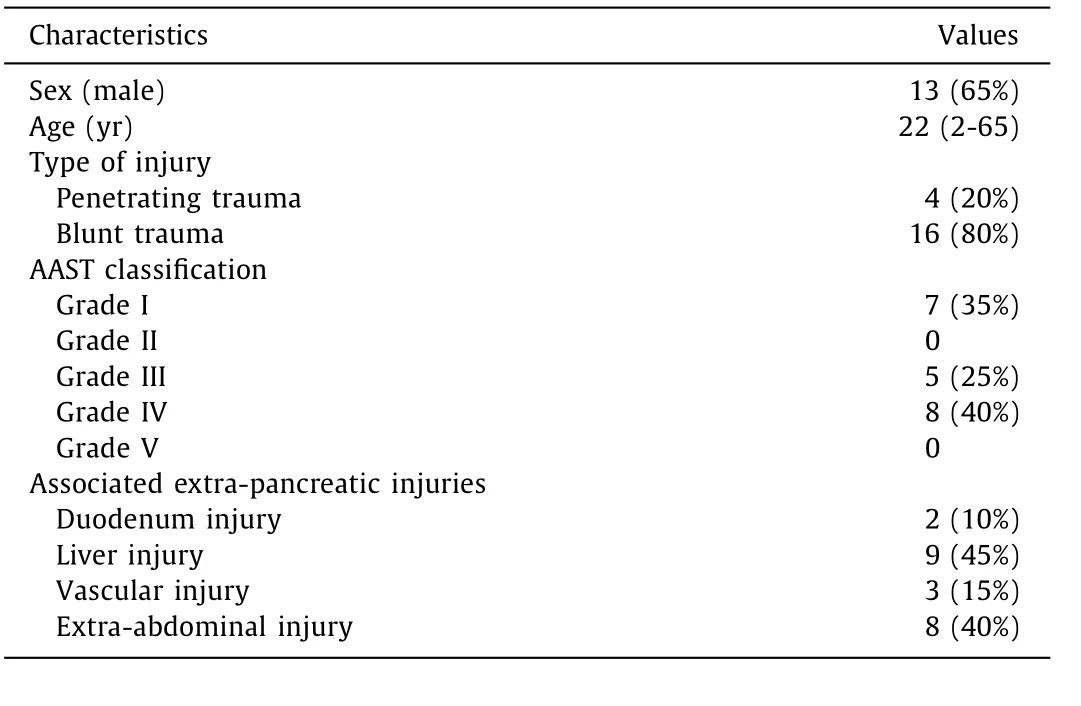
Table 1 Demographic and injury profile ( n = 20)
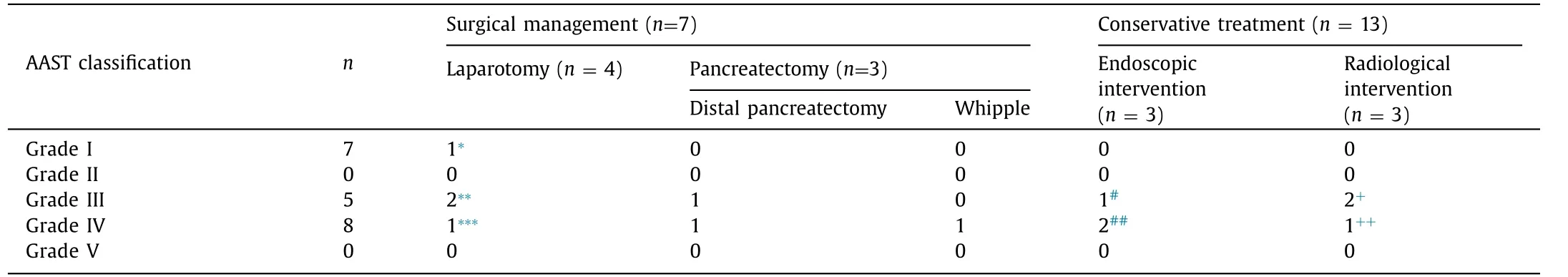
Table 2 Management of pancreatic trauma.
Acknowledgments
None.
CRediT authorship contribution statement
Nadia Matias:Data curation, Formal analysis, Writing - original draft.Santhalingam Jegatheeswaran:Methodology, Formal analysis, Writing - original draft.Vinotha Nadarajah:Data curation, Formal analysis.Aali J. Sheen:Conceptualization, Writing - review &editing.Saurabh Jamdar:Supervision, Formal analysis, Writing -review & editing.Ajith K. Siriwardena:Conceptualization, Supervision, Writing - review & editing.
Funding
None.
Ethical approval
This study was registered as an audit with Manchester University National Health Service Foundation Trust (audit number 7161).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Serum non-high-density lipoprotein cholesterol level is increased in Chinese patients with nonalcoholic fatty liver disease
- Increased CMTM4 mRNA expression predicts a poor prognosis in patients with hepatocellular carcinoma
- Folfirinox chemotherapy prolongs stent patency in patients with malignant biliary obstruction due to unresectable pancreatic cancer
- Role of phosphorylated Smad3 signal components in intraductal papillary mucinous neoplasm of pancreas ✩
- Diagnostic accuracy of administrative database for bile duct cancer by ICD-10 code in a tertiary institute in Korea
- Long noncoding RNA HAND2-AS1 re duce d the viability of hepatocellular carcinoma via targeting microRNA-300/SOCS5 axis
