Folfirinox chemotherapy prolongs stent patency in patients with malignant biliary obstruction due to unresectable pancreatic cancer
2021-01-07JinwooKngSngHyubLeeJinHoChoiWooHyunPikDongWonAhnJiBongJeongJiKonRyuYongTeKim
Jinwoo Kng , Sng Hyub Lee , Jin Ho Choi , Woo Hyun Pik , Dong-Won Ahn , b ,Ji Bong Jeong , Ji Kon Ryu , Yong-Te Kim
a Department of Internal Medicine and Liver Research Institute, Seoul National University Hospital, Seoul National University College of Medicine, Seoul,Korea
b Department of Internal Medicine, SMG-SNU Boramae Medical Center, Seoul, Korea
Keywords:Stent patency Malignant distal biliary obstruction Pancreatic cancer Folfirinox Chemotherapy
A B S T R A C T Background: Stent insertion for biliary decompression to relieve jaundice and subsequent biliary infection is necessary for patients with biliary obstruction caused by pancreatic cancer, and it is important to keep the stent patent as long as possible. However, few studies have compared stent patency in terms of chemotherapy in patients with pancreatic cancer. This study aimed to evaluate the differences in stent patency in terms of recently evolving chemotherapy.Methods: Between January 2015 and May 2017, 161 patients with pancreatic cancer who had undergone biliary stent insertion with a metal stent were retrospectively analyzed. The relationship between chemotherapy and stent patency was assessed. Additionally, overall survival according to the treatment,risk factors for stent patency, and long-term adverse events were evaluated.Results: Median stent patency was 42 days for patients with the best supportive care and 217 days for patients with chemotherapy (conventional gemcitabine-based chemotherapy and folfirinox) ( P < 0.001).Furthermore, the folfirinox group showed the longest median stent patency and overall survival, with 283 days and 466 days, respectively ( P < 0.001) despite higher adverse events rate. Patients who underwent folfirinox chemotherapy after stent insertion had better stent patency in multivariate analysis (HR = 0.26;95% CI: 0.12-0.60; P = 0.001).Conclusions: Compared with patients who received best supportive care only, patients who underwent chemotherapy after stent insertion had better stent patency. More prolonged stent patency can be expected for patients with folfirinox than conventional gemcitabine-based chemotherapy.
Introduction
Pancreatic cancer is a disease with a five-year survival rate of 8% [1] . The symptom of pancreatic cancer varies, but jaundice and subsequent biliary infection do matter, especially when a lesion is located in the pancreatic head. Biliary infection due to bile stasis correlates with the overall survival [2 , 3] . Therefore, stent insertion for malignant biliary obstruction (MBO) and keeping the stent patency as long as possible is important, not only for the quality of life but also for survival.
Many kinds of the stent have been developed and factors associated with stent patency have been scrutinized. However, few studies have compared stent patency according to chemotherapy. One study showed that chemotherapy could prolong selfexpandable metal stent (SEMS) patency by inhibition of tumor ingrowth [4] . However, recent studies could not confirm a significant difference in the overall duration of the stent according to the chemotherapy [3 , 5-7] . There are some reports that additional treatment modalities, such as photodynamic therapy (PDT) or radiofrequency ablation (RFA), have increased survival in patients with MBO [8 , 9] . But the stent patency was not fully evaluated even in these studies.
In a previous study of stent patency in patients with unresectable pancreatic cancer [3] , patency was associated only with the stage of cancer. At that time, overall survival was actually short because there was no effective palliative chemotherapy regimen. This suggests that the stent patency may not have been evaluated properly. The recent advent of palliative chemotherapy has increased overall survival more than previous gemcitabinebased chemotherapy did [10 , 11] . However, no studies have examined whether these recent chemotherapy regimens affect the patency of the biliary stent in the era of prolonged expected survival of patients with pancreatic cancer. In this study, we investigated the differences in stent patency in terms of chemotherapy.

Fig. 1. Flowchart of the study.
Methods
Patients
This study was approved by the Institutional Review Board of Seoul National University Hospital ( No. 1711-107-901). We retrospectively reviewed the medical records of patients who had undergone biliary stent placement with pancreatic cancer from January 2015, when folfirinox treatment was started in our hospital,to May 2017.
Patients were included if the following conditions were met. Patients had undergone biliary drainage for the first time with SEMS after being diagnosed with pancreatic adenocarcinoma pathologically and had at least a locally advanced stage confirmed by computed tomography (CT), magnetic resonance imaging (MRI), or endoscopic ultrasonography (EUS). Patients were excluded if they had been surgically treated within one month after stent insertion,had less than one month of follow-up, or had a plastic stent inserted. Patients with more than 2 of Cooperative Oncology Group Performance Status (ECOG-PS) were excluded ( Fig. 1 ). Patients were divided first into the best supportive care group and the chemotherapy group. The chemotherapy group was divided into subgroups by chemotherapy regimen: the folfirinox group and conventional gemcitabine-based group. The conventional gemcitabinebased group consisted of gemcitabine alone and gemcitabine plus erlotinib chemotherapy, mostly the latter. Gemcitabine + nabpaclitaxel (Gem/Abraxane) regimen was excluded in the analysis due to the national insurance standards for pancreatic cancer treatment in Korea. At the time of study, relatively few patients were treated by gemcitabine/abraxane regimen because it was not within the coverage of national insurance program. The patient’s chemotherapy was selected after full consideration between the patient and medical staff within the national insurance standards.Patients in the chemotherapy group started treatment as soon as possible after liver function abnormalities had improved enough for chemotherapy by biliary decompression.
The dates of cancer diagnosis, first stent placement, stent revision, and final follow-up or death of each patient were collected.Adverse events and management after stent insertion and cause of stent revision were examined. Total bilirubin level at the time of stent placement, at one week, and at one month after the procedure were also evaluated.
Endoscopic procedure
Endoscopic retrograde cholangiopancreatography (ERCP) was performed with a side-viewing duodenoscope (JF-260 V, TJF-260 V;Olympus Co., Tokyo, Japan) by four experienced endoscopists(>500 ERCPs/year). After selective cannulation of the bile duct, endoscopic sphincterotomy was performed. An appropriate stent was selected according to the location and length of biliary stricture.SEMS used in this study were as follows:(Standard Sci-Tech, Seoul, Korea), Niti-STMstent (Taewoong Medical,Seoul, Korea), WallFlexTM(Boston Scientific, Natick, MA, USA) and(CGbio, Seoul, Korea).
Study outcomes
The primary study outcome was the overall duration of stent patency during treatment. Stent patency was defined as the time from stent placement to stent dysfunction requiring premature stent exchange or operation. Stent dysfunction was defined as signs of cholangitis or when the total serum bilirubin level increased at least two-fold above the baseline level after biliary stent insertion. Secondary outcomes included overall survival according to the chemotherapy regimen, and risk factors for stent patency. Pa-tients were followed up at intervals of 1-2 weeks from the time of stent insertion. The time when the patient died or no longer visited the planned outpatient clinic was set as the end of the followup. Cut-off date was 31st December 2017.

Table 1 Baseline characteristics of patients.
Statistical analysis
Data are shown as a percentage for categorical variables and as the mean ± standard deviation or the median (range) for continuous variables. The significance of differences in clinical parameters between groups was assessed by the Analysis of Variance test and Mann-Whitney test as post-hoc analysis or Chi-square test,if needed. Median duration of overall survival and stent patency were estimated by the Kaplan-Meier method and compared using the log-rank test. Data from patients without stent revision (stent patency) or alive at the time of study (overall survival) were censored. A multivariable Cox proportional hazards model was used to identify the independent predictors of stent patency. Factors with 0.1 levels of significance from the univariate analysis were considered in the multivariate analysis. Results were expressed as hazard ratios (HRs) and 95% confidence interval (95% CI). Statistical significance was assumed at a confidence level of 0.05. Statistical analyses were performed using SPSS 23.0 (SPSS, Chicago, IL, USA).
Results
Baseline characteristics
Between January 2015 and May 2017, 261 patients underwent biliary stent insertion for the first time after diagnosis with pancreatic cancer in our hospital. Of these, 28 patients underwent surgery about one month after the procedure, 38 patients lost their followup within one month after the procedure, and 22 plastic stents were inserted. Among the 173 patients who received a metal stent,12 patients with more than 2 of ECOG-PS were further excluded.Finally, the medical records of 161 patients were analyzed ( Fig. 1 ).Among them, 137 were treated with chemotherapy for more than one month after stent insertion, and 24 were treated with supportive care alone. Of the chemotherapy-treated patients, 72 received folfirinox and 65 received gemcitabine-based chemotherapy.
The comparison of baseline characteristics is shown in Table 1.The best supportive care group was significantly older than the chemotherapy group, and the folfirinox group and gemcitabinebased group showed no difference in age. There were statistical differences among treatment groups in patients’ sex, more male patients included in the gemcitabine-based group. Patients in the folfirinox group tended to have a lower stage of cancer at the time of stent placement. Inserted stent type and complication due to stent insertion were not statistically different among the treatment group. The difference in ECOG-PS distribution according to the treatment was found. All of the patients in the folfirinox group had ECOG-PS of 0 or 1. On the other hand, more than 60% of patients in the supportive care group and the gemcitabine-based group had ECOG-PS of 2. During the clinical course, stent revision was performed for 76 patients. The stent revision rate of the folfirinox group was significantly lower than that in other groups(P<0.001).
Stent patency
When overall stent patency was compared between the chemotherapy group and the best supportive care group, there was a significant difference between the groups: 217 days (95% CI: 141-293 days) in the chemotherapy group and 42 days (95% CI: 12-72 days) in the best supportive care group ( Fig. 2 A;P<0.001)
Stent patency was analyzed after patients with chemotherapy were divided into two groups as folfirinox and traditional gemcitabine-based. Statistically significant longer median patency was found in the folfirinox group, 283 days (95% CI: 232-335 days)in the folfirinox group and 144 days (95% CI: 97-191 days) in the gemcitabine-based chemotherapy group ( Fig. 2 B;P<0.001).
Stent patency was further analyzed by stratifying each treatment group into 2 subgroups, better performance (ECOG-PS of 0 or 1) and poor performance (ECOG-PS of 2) group. In the supportive care group, there was no significant difference in median stent patency according to the performance status (61 days in the better performance group vs. 42 days in the poor performance group,P= 0.488). There was no significant difference between two subgroups among patients with gemcitabine-based chemotherapy(153 days in better performance group vs. 112 days in the poor performance group,P= 0.333), either.

Fig. 2. The stent patency according to the treatment. A: The median patency was 217 days in the chemotherapy group and 42 days in the best supportive care group( P < 0.001, log rank test); B: The median patency was 283 days in the folfirinox group and 144 days in the gemcitabine-based group ( P < 0.001, log rank test). C: The cumulative time to stent dysfunction or patient death was significantly longer in the folfirinox group than in other groups (218 days vs. 135 days vs. 42 days, P < 0.001).BSC: best supportive care.
We also analyzed stent patency by setting patients who died without stent dysfunction as having stent dysfunction. In that case,the median time to stent dysfunction or death without stent dysfunction was also significantly different according to treatment( Fig. 2 C; BSC, 42 days; folfirinox, 218 days; gemcitabine-based, 135 days;P<0.001).
There was no statistically significant difference in median time to stent dysfunction or death without stent dysfunction according to the performance status in both treatment groups (supportive care group: 61 days in better performance group vs. 42 days in poor performance group,P= 0.709; gemcitabine-based group: 193 days in better performance group vs. 108 days in poor performance group,P= 0.072).
Overall survival
Overall survival according to chemotherapy was also evaluated.The best supportive care group had the shortest survival outcome,with a median survival of 142 days (95% CI: 105-179 days). The folfirinox group outlived the other groups, with a median survival of 466 days (95% CI: 392-540 days). The median overall survival of the gemcitabine-based chemotherapy group was 316 days (95% CI:281-351 days) ( Fig. 3 ;P<0.001).
Overall survival was also assessed for each treatment group based on ECOG-PS. In both treatment groups, there were no statistically significant differences in median overall survival according to the performance status (supportive group: 157 days in better performance group vs. 132 days in the poor performance group,P= 0.582; gemcitabine-based group: 316 days in better performance group vs. 288 days in the poor performance group,P= 0.265).
Risk factors for stent patency
Univariate analysis was first performed on the stent patency for demographic, disease, and treatment-related factors of the study population. The analysis showed that old age and poor performance were associated with poor stent patency, and chemotherapy was associated with longer overall patency. In the chemotherapy regimen-based analysis, folfirinox was associated with longer pa-tency than gemcitabine-based chemotherapy. When the multivariate analysis was performed based on these factors, chemotherapy was associated with longer stent patency. Specifically, the folfirinox regimen (HR = 0.26; 95% CI: 0.12-0.60,P= 0.001) was associated with longer stent patency ( Table 2 ).
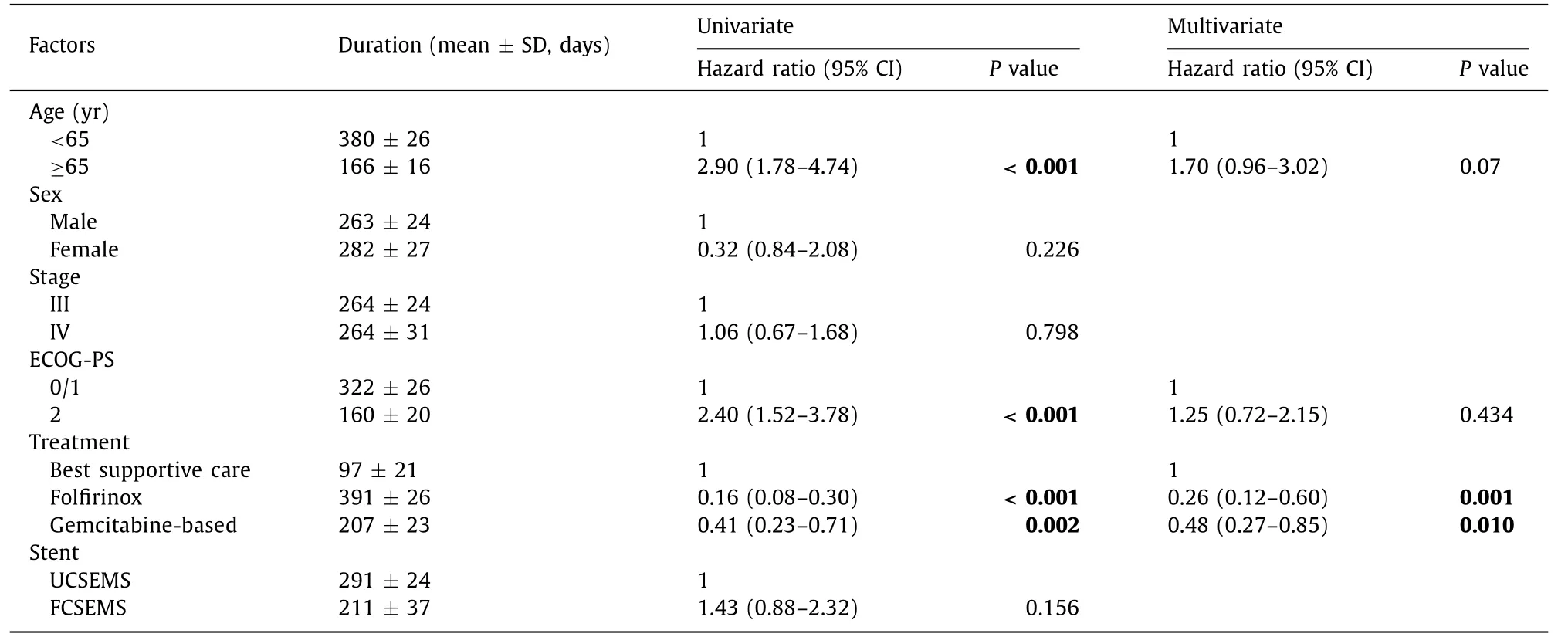
Table 2 Analysis of overall stent patency according to risk factors.

Fig. 3. The overall survival according to the treatment. The median survival was 466 days in the folfirinox group, 316 days in the gemcitabine-based group, and 142 days in the best supportive group ( P < 0.001, log rank test). BSC: best supportive care.
Discussion
The effect of chemotherapy on the patency of SEMS in patients with advanced pancreatic cancer has not been fully evaluated because of the absence of effective palliative chemotherapy.Recently, the folfirinox regimen improved survival outcomes significantly compared to the gemcitabine-based chemotherapy [10] .Thus, we assessed the effect of chemotherapy on stent patency and found that chemotherapy, especially folfirinox, increased stent patency in patients with MBO caused by pancreatic cancer.
In this study, we could confirm longer median patency of stent in the chemotherapy group than in the supportive care group. A gemcitabine-based regimen was the mainstay of the chemotherapy in previous studies [7 , 12 , 13] . That could be the main reason of the different result from our study. More effective response by folfirinox would have affected overall survival but also stent patency.The recent clinical success rate and its related factors after SEMS insertion have been evaluated in patients with malignant colorectal obstruction from peritoneal carcinomatosis [14] . The success rate was significantly lower in patients with more severe carcinomatosis. This suggests that tumor burden matters for the relief of obstruction and longer stent patency. Effective control of the tumor burden is critical for maintaining stent patency as long as possible.
When the revision rate was compared among the treatment groups, more than half of the patients with best supportive care and gemcitabine-based chemotherapy group experienced stent malfunction. Conversely, only about one fourth of patients with folfirinox had stent malfunction. The tumor ingrowth rate was much lower while the stent dislocation rate was higher in the folfirinox group than that in the gemcitabine-based group. Reduced tumor burden by chemotherapy can lead to dislocation of stent as external compression relief. The significantly lower rate of stent malfunction by tumor ingrowth and slightly higher rate of stent dislocation in the folfirinox group reflects the effect of chemotherapy.
In previous studies, shorter overall survival may have been a confounder on the stent patency [3 , 15 , 16] . Another crucial finding of this study is that the overall survival of patients with pancreatic cancer was sufficiently prolonged to evaluate stent patency more precisely. To minimize the confounding effect of overall survival on the stent patency, we analyzed stent patency by setting death without stent dysfunction as a competing risk. There was a significant difference in the cumulative time to stent dysfunction or patient death according to treatment options. This result also suggests the effect of folfirinox on the maintenance of the patency.
In multivariate analysis, only chemotherapy showed significant effect on stent patency. Stage would have a crucial effect when the tumor was poorly controlled by chemotherapy. However, as the efficacy of chemotherapy has improved, it is likely that the impact of the initial stage decreased.
In terms of the type of stent, there was no statistical difference between uncovered self-expandable metal stent (UCSEMS)and fully-covered self-expandable metal stent (FCSEMS) but HR showed slightly higher in FCSEMS. This may be because of more frequent unexpected stent revision caused by migration in the covered stent cases. Previous studies comparing FCSEMS and UCSEMS in malignant distal biliary obstruction from pancreatic carcinoma showed conflicting results [15 , 17] . To evaluate patency according to the type of stent, more sophisticated randomized controlled trials are needed.
Older age may be one of the factors that adversely affects stent patency despite not being statistically significant. The increasing tendency of biliary sludge formation and relatively poorer control of the tumor burden related to less aggressive treatment than in the younger age group may affect shorter stent patency in older age. The imbalance in the age distribution of included patients may have caused the lack of statistical significance.
Local antitumor therapies, such as RFA, PDT, or a drug-eluting metal stent, have been studied for the prolongation of stent patency in malignant bile duct obstruction [8 , 18-20] . Although some of the previously published studies have shown an increase in stent patency by local treatment, those studies included patients with bile duct cancer. Unlike bile duct cancer, extrinsic compression is the main reason for biliary obstruction in patients with pancreatic cancer. In a study with drug-eluting stents, there was a difference in tumor size or infiltration according to the type of stent only in patients with bile duct cancer [19] . The local trial does not seem helpful without aid by systemic chemotherapy in malignant biliary obstruction from pancreatic cancer.
There are several limitations to this study. First, baseline characteristics were not balanced among the treatment groups. Second,patients treated with Gem/Abraxane chemotherapy were not included. At the time of this study, a small amount of patients were treated by Gem/Abraxane because it was not within the coverage of the National Health Insurance (NHI) in Korea. Gem/Abraxane was mostly used as second-line chemotherapy after failure of the folfirinox in Korea, while it has become used worldwidely as first-line chemotherapy. Further studies including Gem/Abraxane chemotherapy are needed. Third, patients with ECOG-PS 3 or more were excluded because the poor performance status may affect overall survival and stent patency was unlikely to be assessed properly.
In conclusion, compared with patients who had received best supportive care only, patients who underwent chemotherapy after stent insertion had better stent patency. More prolonged stent patency can be expected for patients with folfirinox chemotherapy than with conventional gemcitabine-based chemotherapy. If patients with MBO from pancreatic cancer are treated by appropriate chemotherapy with best supportive care, stent patency can be maintained sufficiently long that it may lead to improvement of the patients’ quality of life eventually.
Acknowledgments
None.
CRediT authorship contribution statement
Jinwoo Kang:Conceptualization, Data curation, Formal analysis,Writing - original draft.Sang Hyub Lee:Conceptualization, Formal analysis, Writing - review & editing.Jin Ho Choi:Formal analysis, Writing - review & editing.Woo Hyun Paik:Writing - review& editing.Dong-Won Ahn:Writing - review & editing.Ji Bong Jeong:Writing - review & editing.Ji Kon Ryu:Writing - review& editing.Yong-Tae Kim:Writing - review & editing.
Funding
None.
Ethical approval
This study was approved by the Institutional Review Board of Seoul National University Hospital (No.1711-107-901).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Non-operative management of pancreatic trauma in adults
- Serum non-high-density lipoprotein cholesterol level is increased in Chinese patients with nonalcoholic fatty liver disease
- Increased CMTM4 mRNA expression predicts a poor prognosis in patients with hepatocellular carcinoma
- Role of phosphorylated Smad3 signal components in intraductal papillary mucinous neoplasm of pancreas ✩
- Diagnostic accuracy of administrative database for bile duct cancer by ICD-10 code in a tertiary institute in Korea
- Long noncoding RNA HAND2-AS1 re duce d the viability of hepatocellular carcinoma via targeting microRNA-300/SOCS5 axis
