Changes in thyroid function in patients with liver failure and their clinical significance: A clinical study of non-thyroidal illness syndrome in patients with liver failure
2021-01-07HongLingFengQianLiWuKuiCaoJiMingYang
Hong-Ling Feng, Qian Li , Wu-Kui Cao, Ji-Ming Yang
Intensive Care Unit, Tianjin Second People’s Hospital, Tianjin 300192, China
Keywords:Liver failure Non-thyroidal illness syndrome Free triiodothyronine Prognosis
A B S T R A C T Background: Non-thyroidal illness syndrome (NTIS) develops in a large proportion of critically ill patients and is associated with high risk for death. We aimed to investigate the correlation between NTIS and liver failure, and the short-term mortality of patients with these conditions.Methods: The clinical data of 87 patients with liver failure were collected retrospectively, 73 of them were randomly selected for an observational study and to establish prognostic models, and 14 for model validation. Another 73 sex- and age-matched patients with mild chronic hepatitis were randomly selected as a control group. Serum free triiodothyronine (FT3), free thyroxine (FT4), and thyroid-stimulating hormone(TSH) were measured. The clinical characteristics of patients with liver failure and NTIS were analyzed.The follow-up of patients lasted for 3 months. Additionally, the values for predicting short-term mortality of model for end-stage liver disease (MELD), Child-Turcotte-Pugh (CTP), chronic liver failure-sequential organ failure assessment (CLIF-SOFA) scores, FT3-MELD model, and FT3 were evaluated.Results: The observation group had significantly lower FT3 (2.79 ± 0.71 vs. 4.43 ± 0.75 pmol/L, P < 0.001)and TSH [0.618 (0.186-1.185) vs. 1.800 (1.570-2.590) mIU/L, P < 0.001], and higher FT4 (19.51 ± 6.26 vs.14.47 ± 2.19 pmol/L, P < 0.001) than the control group. NTIS was diagnosed in 49 of the patients with liver failure (67.12%). In the observation group, patients with NTIS had a higher mortality rate than those without (63.27% vs. 25.00%, P = 0.002). Across the whole cohort, the 3-month mortality was 50.68%. The international normalized ratios (INR) were 2.40 ± 1.41 in survivors and 3.53 ± 1.81 in deaths ( P = 0.004),the creatinine (Cr) concentrations were 73.27 ± 36.94 μmol/L and 117.08 ± 87.98 μmol/L ( P = 0.008),the FT3 concentrations were 3.13 ± 0.59 pmol/L and 2.47 ± 0.68 pmol/L ( P < 0.001), the MELD scores were 22.19 ± 6.64 and 29.57 ± 7.99 ( P < 0.001), the CTP scores were 10.67 ± 1.53 and 11.78 ± 1.25( P = 0.001), and the CLIF-SOFA scores were 8.42 ± 1.68 and 10.16 ± 2.03 ( P < 0.001), respectively.FT3 was negatively correlated with MELD score ( r = -0.430, P < 0.001). An FT3-MELD model was established by subjecting FT3 concentration and MELD score to logistic regression analysis using the following formula: Logit( P ) = -1.337 × FT3 + 0.114 × MELD + 0.880. The area under the receiver operating characteristic (ROC) curve was 0.827 and the optimal cut-off value was 0.4523. The corresponding sensitivity and specificity were 67.6% and 91.7%. The areas under the ROC curve for FT3 concentration,MELD score, CTP score, and CLIF-SOFA score were 0.809, 0.779, 0.699, and 0.737, respectively.Conclusions: Patients with liver failure often develop NTIS. FT3-MELD score perform better than CTP and CLIF-SOFA scores in predicting mortality in patients with liver failure. Thus, the FT3-MELD model could be of great value for the evaluation of the short-term mortality of such patients.
Introduction
Non-thyroidal illness syndrome (NTIS) is characterized by metabolic disorders affecting thyroid hormones and causing nonthyroidal dysfunction. About 44%-70% of critically ill patients have associated NTIS [1] . NTIS is closely associated with the prognosis of many critical illnesses and chronic diseases, such as certain tumors [2] , sepsis [3 , 4] , end-stage renal disease [5 , 6] , and refractory heart failure [7 , 8] . The liver is an important target organ of thyroid hormones, and is involved in the production, excretion, and peripheral deiodination of thyroid hormones, and in the synthesis of thyroxine-binding globulin (TBG). It is thus important for the metabolism and function of thyroid hormones.When liver function is severely impaired, thyroid hormone concentrations change to varying degrees [9] . For example, Israel et al.reported that T3 concentration inversely correlates with the severity of viral hepatitis and alcoholic liver disease [10] . Furthermore,abnormal thyroid hormone concentrations are reportedly associated with greater mortality in patients with type A hepatic encephalopathy [11] . Finally, Mansour-Ghanaei et al.reported that serum total T3 concentration is lower in patients with cirrhosis who died within 3 months than in long-term survivors [12] . Collectively, these studies show that the incidence of NTIS is significantly higher in patients with chronic liver diseases of various causes,including cirrhosis and end-stage liver disease, and that thyroid hormone concentration is associated with the severity of liver disease.
Liver failure denotes serious impairment of liver function that can be caused by a variety of factors. It is associated with serious disorders or decompensation of liver functions, such as synthesis, detoxification, excretion, and biotransformation. This leads to the development of a series of clinical syndromes, mainly characterized by coagulopathy disorders, jaundice, hepatic encephalopathy, and ascites [13-15] . In patients with liver failure, damage to the hepatic parenchyma causes disordered thyroid hormone deiodination, lower synthesis of TBG, and secondary hypothalamicpituitary-thyroid axis dysfunction, leading to changes in the concentrations of thyroid hormones and their metabolites, which together constitute NTIS.
Up to now, few published studies have addressed the clinical significance of NTIS in patients with liver failure. In the present study, we aimed to identify differences in thyroid function-related indicators in patients with liver failure and to analyze their ability to predict mortality.
Methods
Case selection
The clinical data of patients with liver failure who had been hospitalized in the Intensive Care Unit of Tianjin Second People’s Hospital between January 2013 and December 2017 were collected retrospectively. The diagnostic criteria for liver failure comprised severe gastrointestinal symptoms, hyperbilirubinemia, abnormal blood coagulation (international normalized ratio [INR] ≥1.5), hepatic encephalopathy, and other serious symptoms and signs associated with liver disease. Diagnoses of liver failure were made on the basis of the diagnostic and treatment guidelines for liver failure(2012 version) [16] . The initial study cohort comprised 195 patients for whom complete sets of data were available. The exclusion criteria were as follows: presence of 1) received liver transplantation;2) chronic liver failure (CLF); 3) primary thyroid disease or positive serum thyroglobulin antibody (TgAb) and/or thyroid peroxidase antibody (TPoAb); 4) major disease in other organs, active infection,liver cancer, and/or other advanced malignant tumor; 5) renal dysfunction caused by underlying renal disease; and 6) severe cardiac and cerebrovascular disease, such as coronary heart disease,heart failure, or cerebral infarction. In accordance with these criteria, 108 patients were excluded and the data from the remaining 87 patients with liver failure were analyzed. These patients comprised 66 men and 21 women, aged 52.00 (38.00-60.00) years, 16 of whom had acute liver failure (ALF), 20 subacute liver failure(SALF), and 51 acute-on-chronic liver failure (ACLF). The causes of liver failure were hepatitis B (n= 57), hepatitis C (n= 2), hepatitis E (n= 14), autoimmune liver disease (n= 4), alcoholic hepatitis(n= 4), and undetermined causes (n= 6).
Principal measures
Relevant clinical data were collected including thyroid, liver,and renal function; blood coagulation markers; PaO 2 /FiO 2 ; and other data collected within 24 h of diagnosis. Survival and mortality were recorded in the third month.
Serum thyroid function tests were examined. Thyroid function was assessed using a Cobas e411 electrochemiluminescence automatic immunoassay analyzer (Roche Diagnostics, Tokyo, Japan).FT3, FT4, thyroid-stimulating hormone (TSH), TgAb, and TPoAb were determined by electrochemiluminescence (ECL) (Roche Diagnostics). The reference ranges for the thyroid function tests were:FT3, 3.1-6.8 pmol/L; FT4, 12-22 pmol/L; TSH, 0.27-4.20 mIU/L;TgAb, 0-115 IU/mL; and TPoAb, 0-34 IU/mL.
Model for end-stage liver disease (MELD) score was calculated using the following formula: MELD = 3.8 × ln(TBil[mg/dL]) +11.2 × ln(INR) + 9.6 × ln(creatinine [Cr; mg/dL] + 6.4 × cause(cause: cholestasis or alcohol, 0; others, 1). The final result was stated as an integer [17] .
Child-Turcotte-Pugh (CTP) score was calculated according to the severity of hepatic encephalopathy and ascites, and the bilirubin,INR, and albumin values [18] .
Chronic liver failure-sequential organ failure assessment (CLIFSOFA) score was calculated according to the cumulative damage present in six organ systems: the lungs, coagulation, liver, circulation, kidneys, and brain [19] .
Patient groups
The 87 patients with liver failure were randomly allocated to two groups at a ratio of 5:1; 73 were selected for an observational study and to establish prognostic models [observation group; 55 men and 18 women, aged 52.0 0 (37.0 0-61.50) years] and the other 14 patients were reserved for model validation [validation group;11 men and three women, aged 51.50 (40.25-57.50) years]. The selection of the two groups followed the same guidelines [16] . Furthermore, another 73 sex- and age-matched patients [55 men and 18 women, aged 52.00 (35.00-60.00) years] with mild chronic hepatitis were randomly selected to form a control group: 58 of them had hepatitis B, 12 hepatitis C, and three both hepatitis B and hepatitis C. These diagnoses were made on the basis of the Chinese guidelines for the prevention and treatment for chronic hepatitis B(2015 edition) and the Chinese guidelines for the prevention and treatment of hepatitis C (2015 edition) [20 , 21] .
The follow-up of patients lasted for 3 months. The patients who had been discharged were followed up by telephone. There were 36 survivors (49.32%) and 37 deaths (50.68%) in the observation group. More specifically, 10 of 14 patients with ALF, 6 of 18 with SALF, and 21 of 41 with ACLF died, yielding mortality rates of 71.43%, 33.33%, and 51.22%, respectively.
Statistical analysis
Statistical analysis was performed using SPSS 20.0 software.Normally distributed measurement data were described as mean ± standard deviation (SD) and analyzed using Student’sttest, and non-normally distributed data described as median[interquartile range (IQR)]) and using the Mann-WhitneyUtest.Numerical data were described as number (N) and analyzed using the Chi-square test. Kaplan-Meier survival curves were used topredict the mortality of patients with and without NTIS in the observation group. In addition, Pearson correlations were calculated,and logistic regression analysis was used to establish a prognostic model. The value of each prognostic masker in predicting mortality of patients with liver failure was determined using the area under the receiver operating characteristic (ROC) curve. AP<0.05 was considered statistically significant.
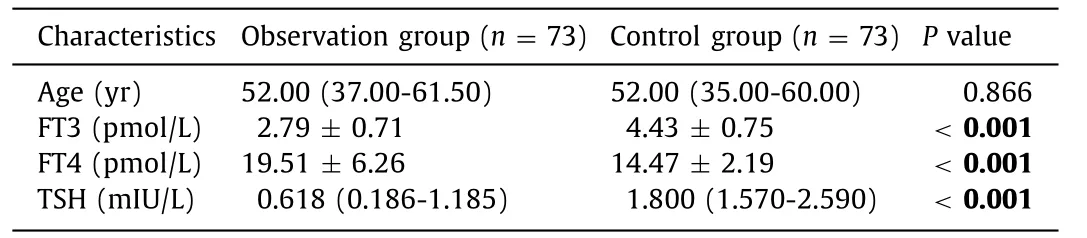
Table 1 Comparison of thyroid-related hormone concentrations between the observation and control groups
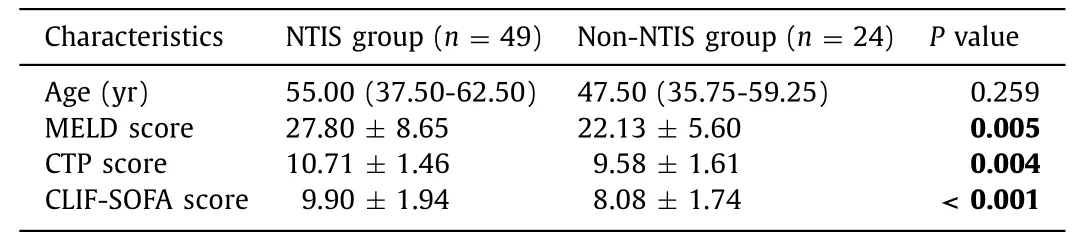
Table 2 Comparison of the clinical features of patients with liver failure, classified according to their NTIS status
Results
Differences in serum markers of thyroid function between the observation and control groups
The thyroid-related hormone concentrations in the observation and control groups are listed in Table 1 . The serum FT3 and TSH concentrations in the observation group were 2.79 ± 0.71 pmol/L and 0.618 (0.186-1.185) mIU/L, respectively, which were lower than those in the control group [4.43 ± 0.75 pmol/L and 1.800 (1.570-2.590) mIU/L,P<0.001 for both measures]. The serum FT4 concentration in the observation group was higher than that in the control group (19.51 ± 6.26 vs. 14.47 ± 2.19 pmol/L,P<0.001).
Clinical features of patients with NTIS and liver failure
NTIS, which manifests as low serum FT3 and normal or low TSH concentration, was diagnosed in 49 of the 73 patients with liver failure (67.12%). Thirty-one of the 49 patients with liver failure and NTIS had normal FT4 concentrations, 17 of whom died (54.84%);11 had high FT4 concentrations, nine of whom died (81.82%); and seven had low FT4 concentrations, five of whom died (71.43%). TSH was normal in 32 patients and low in 17; 17 of the 32 patients with normal TSH died (53.13%), as did 14 of the 17 with low TSH(82.35%) (P= 0.043).
Comparison of the clinical features of patients with and without NTIS in the observation group
The clinical features of the patients, classified according to study group, are listed in Table 2 . The MELD, CTP, and CLIF-SOFA scores were significantly different between patients with and without NTIS (P<0.05), whereas there was no significant difference between these groups with regard to age (P>0.05).

Fig. 1. Survival curves for patients with and without NTIS.

Table 3 Comparison of the clinical features of patients with liver failure, classified according to outcome
In the observation group, patients with NTIS had a higher mortality than those without (63.27% vs. 25.00%,P= 0.002, Fig. 1 ).
Comparison of the clinical features of patients with different outcomes
The clinical features of the patients, classified according to outcomes, are listed in Table 3 . The INR, Cr and FT3 concentrations,MELD, CTP, and CLIF-SOFA scores were significantly different between the survivors and deaths (P<0.01), whereas there were no significant differences with regard to age, TBil, albumin (ALB), FT4,or TSH (P>0.05).
Correlation between FT3 and MELD scores
There was a negative correlation between FT3 and MELD score in patients with liver failure (r= -0.430,P<0.001, Fig. 2 ).
Establishment of a prognostic model
After the FT3 and MELD scores had been subjected to logistic regression analysis, forward logistic regression was used to establish an FT3-MELD model. The equation created for determining prognosis was as follows: Logit(P) = ln(P/[1 -P]),P= 1/(1 + e-Logit(P) ), Logit(P) = -1.337 × FT3 + 0.114 × MELD +0.880.

Fig. 2. Correlation between free triiodothyronine (FT3) and model for end-stage liver disease (MELD) score ( r = -0.430, P < 0.001).
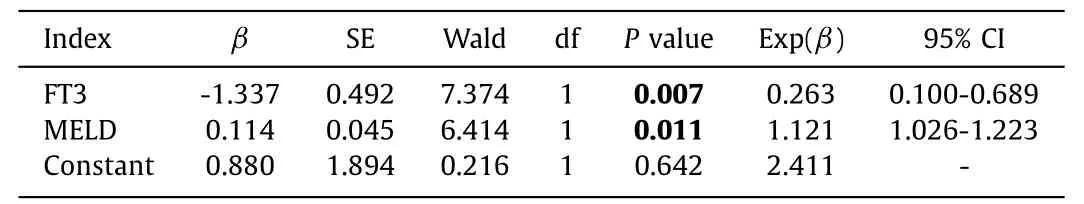
Table 4 Regression coefficients and statistical tests for the FT3-MELD model
Finally, all the regression coefficients for each indicator in the FT3-MELD model were validated ( Table 4 ).
Evaluation of the prognostic value of the candidate predictors of liver failure
The areas under the ROC curves (AUCs) of the candidate predictors of mortality in patients with liver failure were: FT3-MELD model>FT3>MELD score>CLIF-SOFA score>CTP score. The 95% confidence interval, cut-off value, Youden index, sensitivity,and specificity of each are shown in Table 5 and Fig. 3 . The FT3-MELD model was validated using the 14 patients in the validation group, the sensitivity, specificity and accuracy were 80.0% (8/10),85.7% (6/7) and 82.4% (14/17), respectively.
Discussion
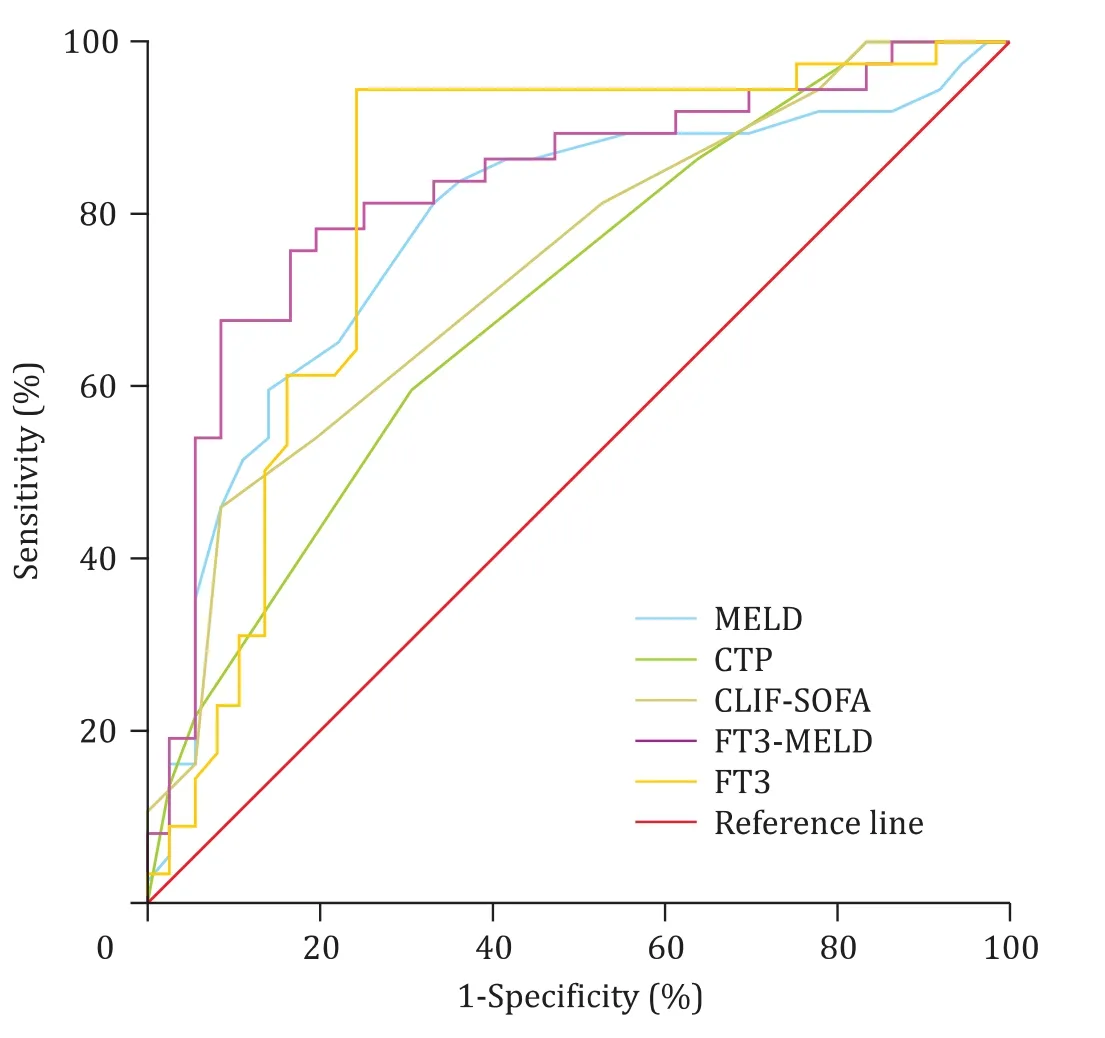
Fig. 3. Receiver operating characteristic curves for the potential prognostic indicators.
NTIS usually manifests as low serum FT3 and TT3, high reverse T3 (rT3), normal or mildly increased FT4 and total thyroxine(TT4), and normal or low TSH concentrations. In severe cases, the TT4 and FT4 concentrations may be low and that of TSH normal;this is known as low T3-T4 syndrome. Changes in thyroid function are often thought to be as an adaptive response to disease [9 , 22] .Because the prevalence of NTIS increases with age and is much higher in women, we randomly selected sex- and age-matched patients with mild chronic hepatitis to form a control group, in an attempt to rule out the impacts of age and sex on our research findings [1 , 9] . In addition, the thyroid autoantibodies TgAb and TPoAb are risk factors for autoimmune thyroid disease, and to some extent reflect the degree of thyroid tissue damage [9 , 22] . Therefore,in the present study, we excluded patients with liver failure and positive serum TgAb or TPoAb. The free thyroid hormones FT3 and FT4 are the active forms, and their concentrations are not affected by the change of serum TBG concentration. We therefore chose FT3 and FT4 as the markers to assess in the present study. In our cohort of patients with liver failure, the incidence of NTIS was 67.12%.We found that the serum FT3 and TSH concentrations were significantly lower and that of FT4 higher in the liver failure group than in the control group, which confirms the effect of liver failure on thyroid hormone concentration reported by Wu et al. [23] .The possible mechanisms for this include: a) impaired thyroid hormone deiodination in patients with liver failure, which causes abnormal deiodination of T4 in peripheral tissues; b) lower TBG synthesis in the liver; c) higher concentrations of cytokines, such as interleukin-1 (IL-1), IL-6, tumor necrosis factor (TNF)-α, and hormones metabolized by the liver, leading to hypothalamic-pituitary dysfunction; and/or d) nutritional disorders, electrolyte metabolism disorders, high blood ammonia, low dopamine, a high-stress state,and/or other factors associated with liver failure [9 , 22] .
Liver failure is a common complication of severe liver disease.Accurate assessment of liver failure is essential for the prompt selection of appropriate treatments (e.g., the maintenance of current medical treatment or liver transplantation). Previous studies have demonstrated that liver transplantation is the most effective salvage treatment for chronic liver failure. However, because we wish to facilitate early disease identification and intervention,we excluded patients with chronic liver failure from the present study [24] . CTP scoring has been widely used to assess reserve liver function and predict the mortality of severe liver disease [18] .In the present study, the predictive power of CTP score was only 0.699 and its accuracy was poor, such that when we used CTP score to predict the mortality of liver failure, the range of scores was narrow and the discriminating power was poor. The severity of liver disease may differ between critically ill patients with the same score; therefore, this score could not be used to further categorize such patients. The CLIF-SOFA scoring system was first developed in a prospective European cohort study of patients with acute decompensated alcoholic cirrhosis and includes multiple indicators relating to liver, brain, kidney, circulation, coagulation, and lung function. In contrast with the Chinese diagnostic criteria for liver failure, which are based on the causes of hepatic dysfunction and of liver failure, the CLIF-SOFA scoring system is based on the extrahepatic causes of liver failure and the failure of extrahepaticorgans [19] . In the present study, the accuracy of the CLIF-SOFA score as a predictor of mortality in patients with liver failure was still poor, with the AUC being 0.737 and the specificity being 91.7%,but the sensitivity was low (only 45.9%), suggesting that patients with high CLIF-SOFA scores usually have more severe disease and that CLIF-SOFA scores are not helpful in guiding early identification and intervention. The MELD model has been shown to be a useful tool for the prediction of case mortality and to allocate liver grafts in patients with cirrhosis, liver cancer, and various types of liver failure [15 , 17] . In the present study, the MELD scores were much higher in the group of patients that died from liver failure than that in the survival group. The MELD score having an AUC of 0.779 had higher ability to predict mortality in patients with liver failure.This finding is consistent with those of previous reports [15 , 17] .

Table 5 Values of each potential prognostic indicator
In recent years, the clinical value of NTIS as a predictor of mortality in patients with liver failure has been increasingly recognized. Anastasiou et al. showed that the incidence of NTIS was significantly higher in patients who did not recover spontaneously [25] . In the present study, the mortality of patients with liver failure and NTIS was higher than that of patients with liver failure who did not have NTIS, suggesting that the combination of liver failure and NTIS is a critical condition with a poor outcome. Agiasotelli et al. reported that low FT3 is associated with early death from ACLF [26] . In the present study, the FT3 concentration was significantly lower in patients who died than in those who survived, and the AUC for FT3 for its use as a predictor of mortality in patients with liver failure was 0.809 with a sensitivity of 94.4% and a specificity of 75.7%, which was higher than that of the MELD score (0.779), suggesting that FT3 concentration may be a useful predictor of mortality. Further analysis showed that the survival rate was highest (14/31, 45.16%) in patients with low FT3 alone and normal FT4. The mortality was 81.82% (n= 9) in 11 patients with low FT3 and high FT4, possibly reflecting the extensive death of parenchymal cells in the liver and the resulting reduction in peripheral conversion of T4 to T3, which is consistent with these patients being in a critical condition. Both the FT3 and FT4 concentrations were low in seven of our patients, and five of them(5/7, 71.43%) died. Given that FT3 and FT4 decrease with increasing severity of liver failure, it has been speculated that metabolism is actively reduced to facilitate energy balance and alleviate injuries in such patients, thus maximizing the function of vital organs. Therefore, patients with liver failure and low T3-T4 syndrome tend to have poor outcome, and early intensive interventions may help to improve their outcomes. In the present study, we found that mortality tended to be higher in patients with liver failure plus NTIS and abnormal FT4 than in those with normal FT4 [77.78%(14/18) vs. 54.84% (17/31)]; however, this difference was not statistically significant (P= 0.108), which may be attributable to the small sample size. Thus, the clinical utility of FT4 as a predictor of mortality in patients with liver failure plus NTIS needs to be further explored in larger studies [27] . In the present study, TSH concentration was related to the mortality rate of patients with liver failure and NTIS.
In recent years, the role of systemic inflammatory responses in the pathogenesis of liver failure has been well recognized [28] .During liver failure, neuroendocrine system stress disorder and the excessive release of systemic inflammatory mediators occur,which often lead to hormone metabolism disorders, characterized by abnormalities in the pituitary-thyroid axis, namely NTIS. Thus,thyroid hormone concentrations are metabolism-related indicators that can reflect the severity of systemic inflammatory responses. In the present study, FT3 negatively correlated with MELD score. FT3 reflects the status of the systemic inflammatory response, whereas MELD score quantifies the pathophysiological changes, such as coagulation disorders, hyperbilirubinemia, and renal failure, in patients with severe impairments of liver function. The use of a combination of these two indicators could help to improve the performance of predicting mortality in patients with liver failure. After subjecting FT3 and MELD score to logistic regression analysis, we established the FT3-MELD model, which had an AUC of 0.827, a sensitivity of 67.60%, and a specificity of 91.70%, as a short-term predictor of mortality in patients with liver failure. This model was validated using the reserve cases, because it yielded high sensitivity, specificity and accuracy and performed significantly better than FT3 or the MELD score alone, suggesting that the FT3-MELD model is preferable as a prognostic marker predicting mortality in patients with liver failure.
Although the manifestations of NTIS may differ between clinical settings, thyroid hormone concentrations can still be used as prognostic factors of liver failure. In the present study, both FT3 and MELD score were shown to predict short-term mortality in patients with liver failure. The FT3-MELD model we developed has an AUC of 0.827 for use as a short-term mortality factor and therefore could be used for this purpose in Chinese patients. However,the present study was limited by its single-center design and small sample size. Therefore, the clinical significance of thyroid hormone concentrations in patients with liver failure and their reliability as a prognostic marker predicting mortality should be further investigated in large, prospective, multi-center studies.
Acknowledgments
None.
CRediT authorship contribution statement
Hong-Ling Feng:Data curation, Project administration, Writing - original draft, Writing - review & editing.Qian Li:Investigation, Project administration, Funding acquisition, Writing - review& editing.Wu-Kui Cao:Data curation, Supervision.Ji-Ming Yang:Data curation.
Funding
This study was supported by a grant from the National Science and Technology Major Project of China (2018ZX10725506-002).
Ethical approval
This study was approved by the Ethics Committee of Tianjin Second People’s Hospital.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Non-operative management of pancreatic trauma in adults
- Hepatocellular carcinoma incidence post direct-acting antivirals in hepatitis C-related advanced fibrosis/cirrhosis patients in Australia
- Efficacy and cost-effectiveness of antiviral regimens for entecavir-resistant hepatitis B: A systematic review and network meta-analysis
- Combined hepatocellular-cholangiocarcinoma: An update on epidemiology, classification, diagnosis and management
- Hepatobiliary&Pancreatic Diseases International
- Safety and efficacy of an integrated endovascular treatment strategy for early hepatic artery occlusion after liver transplantation
