Preservation of platelet function in patients with cirrhosis and thrombocytopenia undergoing esophageal variceal ligation
2021-01-07EvndrodeOliveirSouzlioAntnioAmiconiFloresRochCrolineMrcondesFerreirJulinMedeirosBtistLuizAugustoCrneiroAluquerqueFlirJosCrrilhoAlertoQueirozFris
Evndro de Oliveir Souz , Élio Antônio D’Amico , Tâni Rúi Flores d Roch ,Croline Mrcondes Ferreir , Julin Medeiros Btist , Luiz Augusto Crneiro D’Aluquerque , Flir José Crrilho , Alerto Queiroz Fris
a Division of Gastroenterology and Hepatology, University of Sao Paulo School of Medicine, Av. Dr. Eneas Carvalho de Aguiar, 255, 9th floor, office 9159, Sao Paulo, SP 05403-0 0 0, Brazil
b Hemostasis Laboratory, Hematology Service, University of Sao Paulo School of Medicine, Av. Dr. Eneas Carvalho de Aguiar, 255, 2nd floor, Sao Paulo, SP 05403-0 0 0, Brazil
Keywords:Cirrhosis Hemostasis Thrombocytopenia Platelet aggregation Endoscopy Hemorrage
A B S T R A C T Background: Thrombocytopenia is a possible risk factor for bleeding after band ligation of esophageal varices. However, elevated von Willebrand factor (VWF) in cirrhosis improves platelet function and could decrease this risk. Our objective was to assess platelet function in patients with cirrhosis undergoing esophageal variceal ligation (EVL).Methods: The assessment consisted of platelet count, antigen and activity of VWF and VWF-cleaving protease ADAMTS-13 activity, and a platelet adhesion and aggregation test simulating vascular flow in vivo (Impact-R R ○) prior to EVL.Results: Totally 111 patients were divided into three groups according to platelet count: (1) < 50 × 10 9 /L( n = 38, 34.2%); (2) 50 × 10 9 /L to 100 × 10 9 /L ( n = 47, 42.3%); and (3) > 100 × 10 9 /L ( n = 26, 23.4%). No statistically significant difference was found in the aggregate size of platelets [group 1: 41.0 (31.8-67.3)μm 2 ; group 2: 47.0 (33.8-71.3) μm 2 ; and group 3: 47.0 (34.0-66.0) μm 2 ; P = 0.60] and no significant correlation was found between aggregate size and platelet count (Spearman r = 0.07; P = 0.47). Surface coverage was 4.1% (2.8%-6.7%), 8.5% (4.0%-10.0%), and 9.0% (7.1%-12.0%) ( P < 0.001) in groups 1, 2 and 3, respectively and correlated with platelet count (Spearman r = 0.39; P < 0.0 0 01). There was no significant difference between groups in VWF or ADAMTS-13. Post-EVL bleeding occurred in six (5.4%) patients( n = 2 in group 1, n = 1 in group 2, and n = 3 in group 3; P = 0.32). Patients with bleeding had higher MELD scores [15.0 (11.3-20.3) versus 12.0 (10.0-15.0); P = 0.025], but no difference was demonstrated for platelet function parameters.Conclusion: Platelet function is preserved even in the presence of thrombocytopenia, including in the patients with post-EVL bleeding.
Introduction
Esophageal variceal ligation (EVL) is a front line therapeutic option in the management of esophageal varices [1] . However,post-EVL ulcers can bleed during the period between 3 and 7 days after the procedure in 5% to 10% of cases, with a mortality rate of up to 28% [2 , 3] .
Risk factors for post-EVL bleeding have been little explored in the literature. Data suggest that there is no clear relation between abnormalities in coagulation and the risk of bleeding [4 , 5] . Vieira da Rocha et al. used a variety of routine and expanded coagulation tests to assess post-EVL bleeding in patients with cirrhosis, and concluded that demonstrable abnormalities in coagulation tests had no effect on the frequency of bleeding [6] .Low platelet count, commonly found in cirrhosis, could be a predisposing and intensifying factor for bleeding. However, there is evidence that the functional capacity of platelets is relatively wellpreserved in patients with thrombocytopenia and cirrhosis [7] .
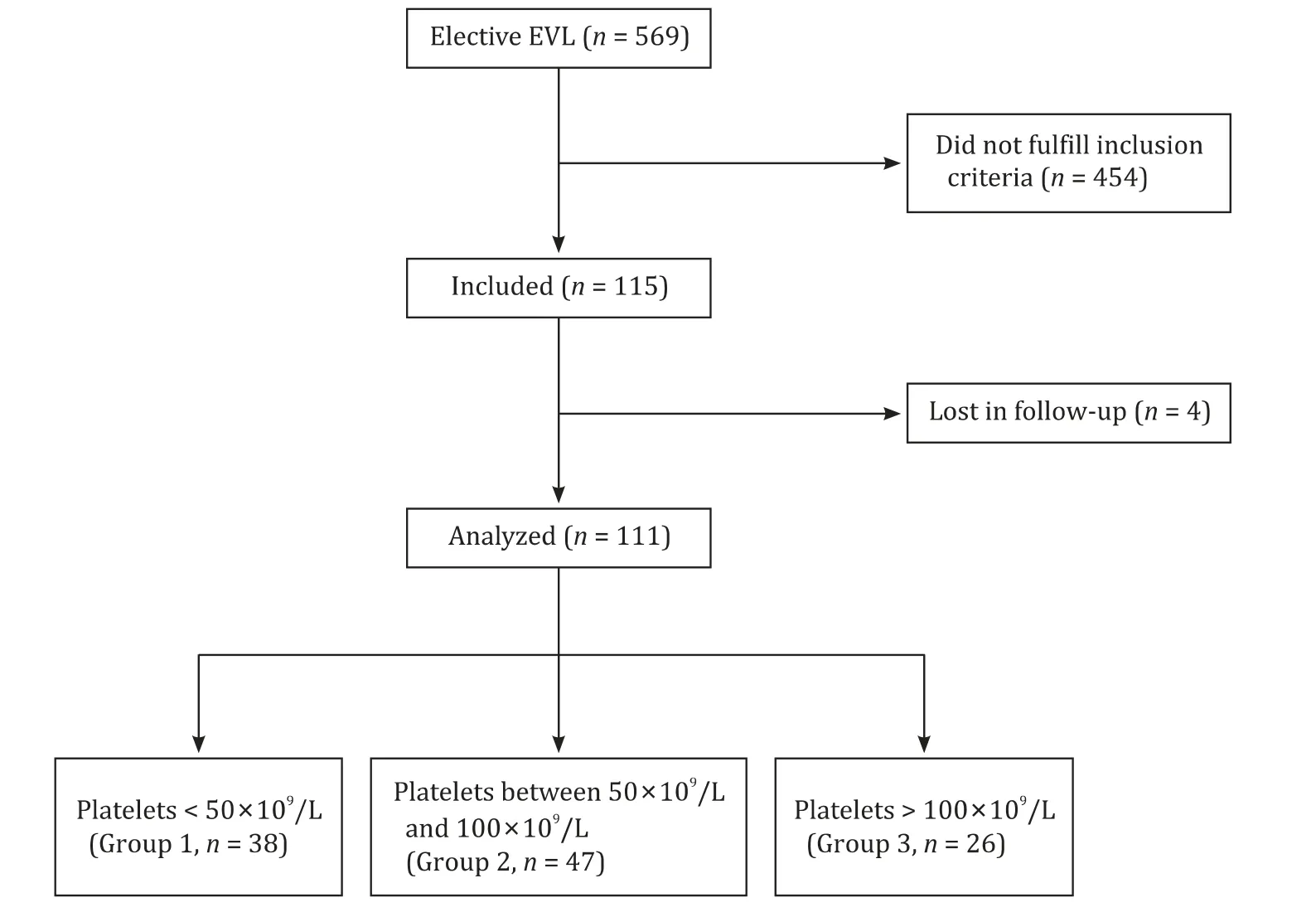
Fig. 1. Inclusion flow chart. EVL: esophageal variceal ligation.
This is because of the imbalance of increased von Willebrand factor (VWF) and reduced levels of its cleaving protease, a disintegrin and metalloprotease with thrombospondin type motifs 13(ADAMTS-13) [8 -10] . This compensatory mechanism could,theoretically, contribute to a reduction in the risk of hemorrhagic complications following invasive procedures. There are, however,few studies evaluating the relationship between platelet function and the occurrence of bleeding following invasive procedures [9] .In this regard, given the lack of a consensus management guideline, low platelet count may be regarded as a cause for concern,leading to liberal transfusion policy prior to invasive procedures.In a survey of one tertiary academic hospital in the USA, liver disease patients accounted for around 8% of the total admissions,but consumed a disproportionate 32.4% of the units of plasma,mostly administered as prophylaxis, and 13% of the total units of platelets transfused [11] .
The objective of this study was to assess platelet function in patients with cirrhosis and its relationship to the frequency of bleeding following EVL. Our hypothesis was that even patients with thrombocytopenia had preserved platelet function, and risk of bleeding comparable to patients within the normal range of platelet count.
Methods
Study design, setting and ethics
This prospective study was conducted from February 2013 to May 2015 in the University of Sao Paulo School of Medicine. The study was performed in accordance with the principles ofHelsinki Declaration, after approval of the protocol by the ethics committee of the institution. Written informed consent was obtained from all patients.
Inclusion and exclusion criteria
Consecutive patients with cirrhosis and referral for elective EVL attending the outpatient clinic were invited to participate. The inclusion criteria were: over 18 years of age, diagnosis of cirrhosis(based on the combination of clinical findings, imaging methods,presence of esophageal varices and/or biopsy-proven cirrhosis when available) and eligibility for endoscopy. Exclusion criteria were: treatment with drugs that interfere with coagulation (i.e.antagonists of vitamin K, antiaggregant drugs, heparins), advanced hepatocellular carcinoma (beyond the Milan criteria), uremia or active bacterial infection. Fig. 1 shows the flowchart of inclusions.
Clinical and laboratory tests
All patients underwent a stringent protocol that included history collection and chart review, and physical examination with venous blood sample taken immediately prior to endoscopy.Platelet count was determined by an automated method; VWF antigen and activity were assessed by an automated immunoassay using the kit(Instrumentation Laboratory Company, Lexington, Massachusetts, USA); ADAMTS-13 activity was tested by enzyme-linked immunosorbent assay (ELISA), with theADAMTS-13 activity kit, purchased from Technoclone(Vienna, Austria). Platelet function was assessed using cone and platelet analyzer technology, which assesses the percentage of surface covered by aggregates as an index of adhesion and the average size of the aggregates in simulated conditions of vascular flow test (Impact-, Diamed, Cressier, Switzerland).
EVL protocol
EVL was performed every 2-4 weeks until esophageal varices were eradicated, using the ligature kit from Cook Medical Company (Bloomington, Indiana, USA). Patients were monitored for 4 weeks after ligation. Post-EVL ulcer bleeding was confirmed by upper digestive endoscopy.
Statistical analysis
Student’sttest and Wilcoxon-Mann-Whitney test were used for continuous variables and Chi-square test for categorical variables.Correlation between aggregate size, surface coverage and platelet count was calculated using the Spearman correlation test. Because of the shape of our data, results were shown as median and interquartile range (IQR). Calculations were performed using the software GraphPad InStat 3.06 and GraphPad Prism 4.0 (GraphPad Software, Inc, La Jolla, California, USA). APvalue of<0.05 was considered statistically significant.
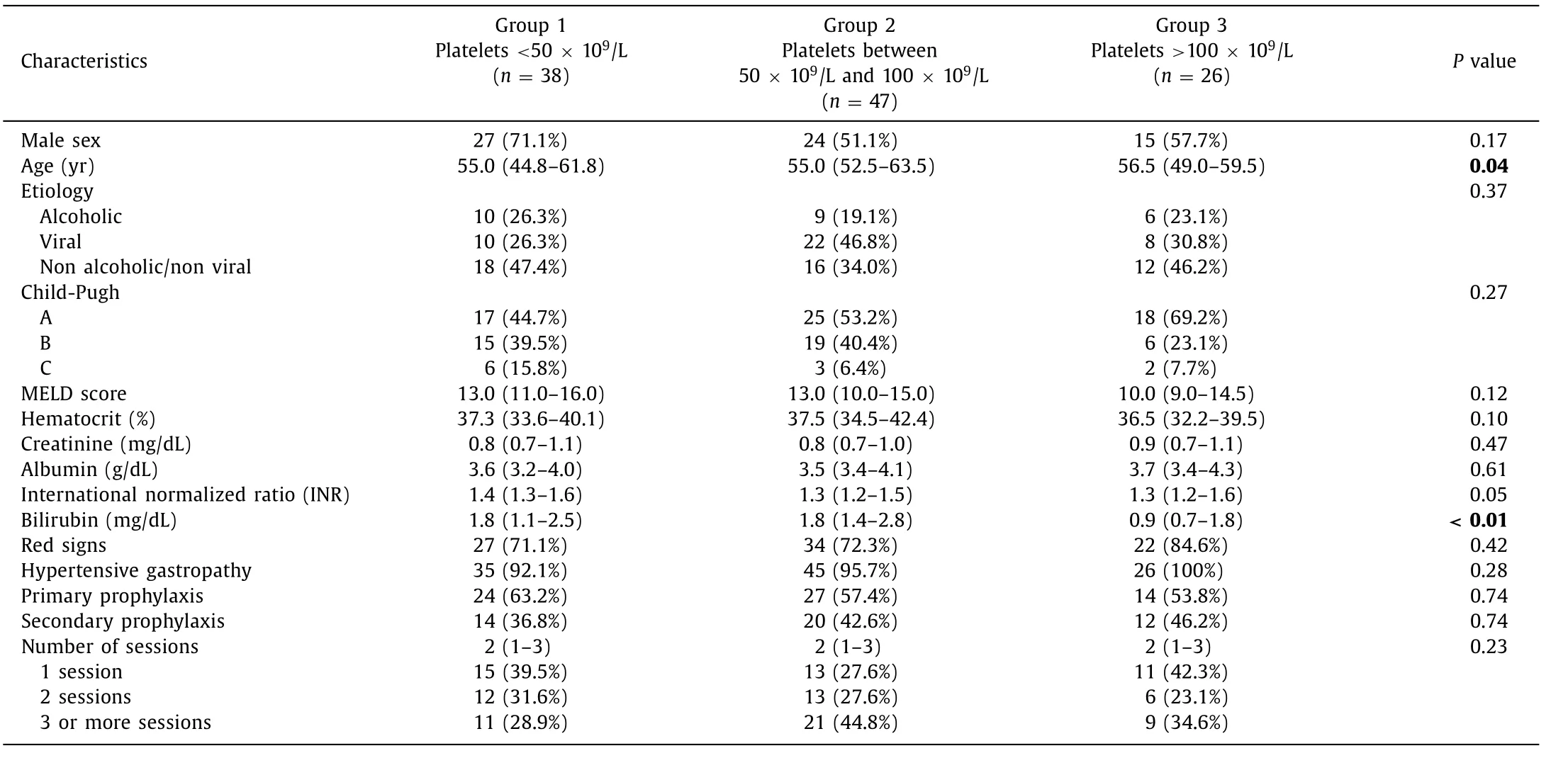
Table 1 Baseline characteristics of included patients
Results
Groups and baseline characteristics
Totally 111 patients were included and divided into three groups according to platelet count values: group 1 (patient with platelet count<50 × 109/L;n= 38, 34.2%); group 2 (patients with platelet count between 50 × 109/L and 100 × 109/L;n= 47,42.3%); and group 3 (patients with platelet count>100 × 109/L;n= 26, 23.4%). Baseline clinical, laboratory and endoscopic characteristics of the patients are shown in Table 1 . The distribution of the etiology of cirrhosis was as follows: hepatitis C infection(n= 34, 30.6%), cryptogenic (n= 32, 28.8%), alcoholic liver disease (n= 25, 22.5%), non-alcoholic steatohepatitis (n= 7, 6.3%),hepatitis B infection (n= 4, 3.6%), secondary biliary cirrhosis(n= 3, 2.7%), hepatitis B and C coinfection (n= 2, 1.8%), primary biliary cholangitis (n= 2, 1.8%), primary sclerosing cholangitis(n= 1, 0.9%) and autoimmune hepatitis (n= 1, 0.9%). Sixty (54.1%)patients were classified Child-Pugh A; 40 (36.0%) Child-Pugh B and 11 (9.9%) Child-Pugh C. The majority of patients (58.6%) underwent band ligation for primary prophylaxis of variceal bleeding. Red signs were found in 74.8%, and hypertensive gastropathy was seen in 95.5% of patients.
Platelet adhesion and aggregation
The overall median value of surface coverage was 10.0%(8.0%-12.0%) (normal value>7.5%) with a statistically significant difference between groups (P<0.001). The surface coverage was 4.1% (2.8%-6.7%), 8.5% (4.0%-10.0%) and 9.0% (7.1%-12.0%)in groups 1, 2, and 3, respectively, and correlated with platelet count (Spearmanr= 0.39;P<0.0 0 01). For the whole series,the median value of aggregate size was 46.0 (33.0-68.0) μm2(normal>25 μm ²), without significant difference between groups[group 1: 41.0 (31.8-67.3) μm2; group 2: 47.0 (33.8-71.3) μm2;group 3: 47.0 (34.0-66.0) μm2]. Even the group of patients with severe thrombocytopenia had high aggregate size median values,which did not correlate with platelet count (Spearmanr= 0.07;P= 0.47). The distribution of values of the surface coverage and aggregate size according to platelet count are shown in Table 2 .
VWF and ADAMTS-13
VWF antigen values were 346.5% (282.0%-417.8%) in group 1,348.0% (301.0%-432.0%) in group 2 and 354.0% (248.0%-504.0%)in group 3 (P= 0.93) (normal range: 38.0%-176.0%). The results for VWF activity were 328.5% (233.3%-384.5%) in group 1, 326.0%(248.0%-388.0%) in group 2 and 364.0% (224.0%-466.0%) in group 3 (P= 0.87) (normal range: 40.0%-157.0%). ADAMTS-13 values were 72.3% (44.0%-82.4%) in group 1, 82.0% (67.3%-89.9%) in group 2 and 66.9% (48.3%-86.7%) in group 3 (P= 0.08) (normal range: 40.0%—130.0%). There was no significant difference between groups in VWF or ADAMTS-13 values as shown in Table 2 .
Post-EVL ulcer bleeding
Post-EVL bleeding occurred in six (5.4%) patients (2 patients in group 1; 1 in group 2, and 3 in group 3;P= 0.32). MELD score was significantly higher in patients with bleeding [15.0 (11.3-20.3)in group with bleeding versus 12.0 (10.0-15.0) in group without;P= 0.025]. There was no significant difference in the functional assessment of platelet parameters in patients with or without bleeding for any of the parameters shown in Table 3 .
Discussion
In this prospective study we assessed markers related to platelet function in patients with cirrhosis undergoing electiveEVL. In this setting the risk of bleeding is typically related to the combination of liver function impairment, magnitude of portal hypertension and presence of coagulopathy. We characterized the capacity for platelet adhesion and aggregation in conditions simulating vascular blood flow.

Table 2 Results of platelet function assessment
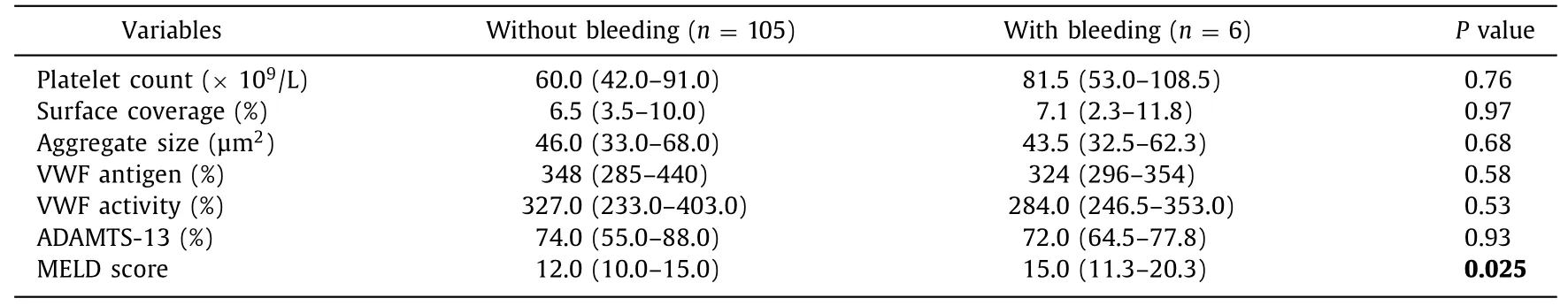
Table 3 Comparison of platelet function test results and MELD score in patients with or without bleeding
We found that the values of aggregated platelet size were within normal range and did not correlate with platelet count.Even patients with platelet count<50 × 109/L were found to have normal values of platelet aggregate size. Furthermore, there was no significant difference in platelet adhesion and aggregation between patients with bleeding and those without. Collectively,these results indicate that compensatory mechanisms maintain platelet adhesion and aggregation in cirrhosis despite thrombocytopenia. There was a linear correlation between platelet surface coverage and platelet count. These results were expected, given that surface coverage represents platelet adhesion and values are directly related to platelet count.
The preservation of platelet aggregation capacity and the dynamic relation between VWF and ADAMTS-13 was demonstrated by Lisman et al. in a study designed to assess the influence of plasma on platelet aggregation under flow conditions in patients with a variety of etiologies and severity of end-stage liver disease [12] . It was found that VWF antigen levels were very high,high-molecular-weight VWF multimers were reduced and the relative collagen binding activity and ristocetin cofactor activity were low, indicating loss of function. However, adhesion of either normal or patient platelets to a collagen surface was increased when these platelets were resuspended in plasma of patients with cirrhosis. This result indicates that high levels of VWF compensate for reduced functional properties expected from low platelet count in cirrhosis [12] .
Debernardi Venon et al. [13] assessed platelet function using three different methods: whole-blood impedance aggregometry(platelet aggregation induced by arachidonic acid and ristocetin),light transmission aggregometry (ADP, collagen, arachidonic acidand ristocetin used as inductors) and the platelet function test PFA-100 (platelet adhesion induced by collagen, epinephrine and ADP). Platelet adhesion/aggregation abnormalities were observed in 94% of patients, but bleeding events occurred in only 13%.
Platelets from patients with cirrhosis can adequately generate thrombin, provided the platelet count is sufficient. Tripodi et al.used an assay for endogenous thrombin generation, modified to account for the contribution of platelets. They demonstrated that thrombin generation correlated with platelet count. Platelet count of 56 × 109/L was a critical cut-off pointinvitro, representing the 10th percentile of the distribution of values of the controls for thrombin generation [7] . However, the optimal values of platelet count for adequate thrombin generationinvivohave yet to be determined. These translational findings might support platelet transfusion for management of bleeding, or the use of thrombopoetin receptor agonists before invasive procedures in patients with low platelet counts. This is despite the preservation in platelet function, as demonstrated by the current study.
Our results showed that both antigen and activity of VWF were elevated in all three groups of patients, without significant difference among them, demonstrating that this compensatory mechanism is uniformly present even in patients with low platelet count. This result corroborates previous studies of raised VWF in patients with cirrhosis. Ferro et al. demonstrated the relationship between increased VWF levels and the endotoxemia found in patients with cirrhosis. This is attributed to endothelial disturbances related to end-stage liver disease and probably to bacterial infections [14] .
Mean values of ADAMTS-13 activity were within normal range in all groups. ADAMTS-13 levels are often reduced in cirrhosis due to the loss of liver function. Other postulated mechanisms include reduced clearance by the cirrhotic liver or release of ADAMTS-13 from hepatic stellate cells or even platelets. The latter is as a result of the activation of platelets due to disseminated intravascular coagulation, commonly found in cirrhosis [15 -17] . Results of ADAMTS-13 varied widely between individual patients; many had very low or very high values. Patients with moderate thrombocytopenia (group B) were found to have higher VWF values when compared to groups A and C [16] . While there is no clear explanatory factor for this, it was also observed in the Lisman’s study. That study attributed this finding to technical difficulty in ADAMTS-13 measurements due to the large coefficient of variation of values, especially in cases with mildly or moderately reduced levels, therefore explaining the poor correlation between different assays [10 , 12] .
Our study controlled for red signs and hypertensive gastropathy as they were present across the three groups defined by platelet count, the difference in bleeding could not be attributed to these variables.
When comparing patients with or without bleeding following EVL, we found a statistically significant difference in the MELD score, suggesting that the severity of end-stage liver disease has an impact on the risk of post-EVL bleeding. It is uncontroversial that the severity of cirrhosis increases the risk of variceal bleeding [18 , 19] . However, it is unclear whether or not patients with more advanced liver disease are more prone to post-EVL ulcer bleeding. Findings on this in the literature are scarce. In 2015, Sinclair et al. found that among patients who underwent EVL as prophylaxis, MELD and gastroesophageal reflux disease could be associated with increased bleeding risk [2] .
We found a rate of bleeding following EVL comparable to others reported in the literature [2 , 20] . Half of the bleeding episodes occurred in the group with platelet count above 100 × 109/L,contrary to the expectation that less severe thrombocytopenia protects the patient from bleeding. The impact of other coagulation abnormalities on post-EVL bleeding has been explored in a prospective study aimed to assess conventional and expanded coagulation indexes. Levels of factor V, fibrinogen, D-dimer, protein C and protein S, VWF, and thromboelastography parameters could not predict bleeding. The only predictive factor was the decline of the liver function (Child-Pugh C status) [6] . Thus, it is likely that factors unrelated to platelets were pivotal, such as higher MELD scores, in patients with bleeding.
Taken collectively, the results of this study call into attention that the status of the liver function (MELD score) may be predictive of bleeding. This has implications for clinical practice.For patients with a deteriorated liver function and candidates for primary prophylaxis of variceal bleeding, one could speculate that beta-blocker therapy should be preferred. However, to date, no study was specifically performed to compare EVL and beta-blockers in patients with severe coagulopathy. This study has limitations that should be acknowledged. We assessed patients undergoing elective EVL. Thus the conclusions may not be generalized to all patients that could benefit from EVL with other complications of cirrhosis such as renal failure, infection and anemia, not assessed in this study. Patients with cirrhosis and renal failure have demonstrable abnormalities in platelet function leading to defects in adhesion to the wall vessel. Anemia reduces platelet adhesion and increases bleeding time. Bacterial infection in patients with cirrhosis are associated with the release of endogenous heparinoids, which produce demonstrable abnormalities in coagulation and could theoretically interfere with thrombin generation [21 , 22] . Since the MELD score was significantly higher in patients with bleeding, future studies should aim to correlate this finding with portal hypertension or liver function. It should be mentioned that the results of the current study are preliminary and need to be confirmed in larger future studies.
In summary, this study showed that platelet function is preserved in cirrhosis even in the presence of thrombocytopenia.This could explain why we could not demonstrate the relationship between low platelet count and post-EVL ulcer bleeding in the elective setting. The only factor associated with bleeding following EVL is higher MELD score.
Acknowledgments
None.
CRediT authorship contribution statement
Evandro de Oliveira Souza:Data curation, Investigation, Formal analysis, Writing - original draft.Élbio Antônio D’Amico:Conceptualization, Supervision, Writing - review & editing.Tânia Rúbia Flores da Rocha:Investigation, Methodology, Project administration, Writing - original draft.Caroline Marcondes Ferreira:Investigation, Project administration, Writing - original draft.Juliana Medeiros Batista:Investigation, Project administration, Writing -original draft.Luiz Augusto Carneiro D’Albuquerque:Supervision,Writing - review & editing.Flair José Carrilho:Supervision, Writing - review & editing.Alberto Queiroz Farias:Conceptualization,Supervision, Formal analysis, Writing - review & editing.
Funding
None.
Ethical approval
The study was performed in accordance with the principles ofHelsinkiDeclaration, after approval of the protocol by the ethics committee of the institution.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Non-operative management of pancreatic trauma in adults
- Hepatocellular carcinoma incidence post direct-acting antivirals in hepatitis C-related advanced fibrosis/cirrhosis patients in Australia
- Efficacy and cost-effectiveness of antiviral regimens for entecavir-resistant hepatitis B: A systematic review and network meta-analysis
- Combined hepatocellular-cholangiocarcinoma: An update on epidemiology, classification, diagnosis and management
- Hepatobiliary&Pancreatic Diseases International
- Safety and efficacy of an integrated endovascular treatment strategy for early hepatic artery occlusion after liver transplantation
