慢性阻塞性肺疾病急性加重合并Ⅱ型呼吸衰竭有创机械通气治疗预后因素分析
2020-12-14莫琼娅董年潘俊杰楼雅芳
莫琼娅 董年 潘俊杰 楼雅芳

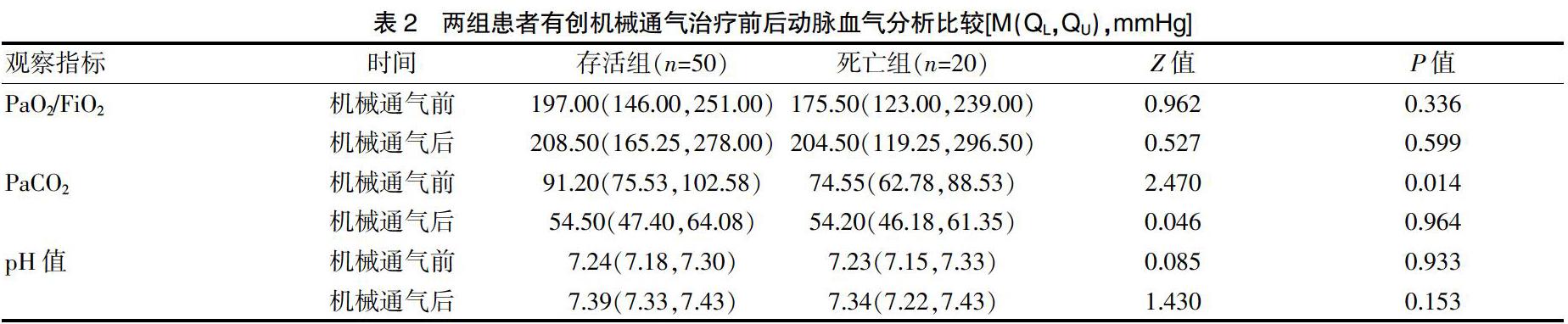
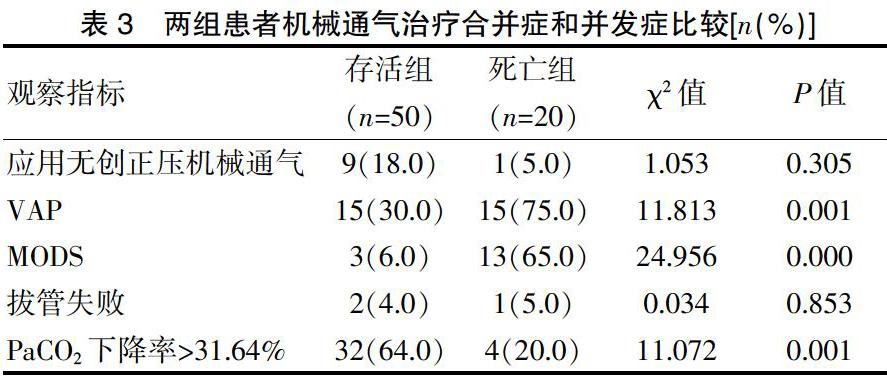
[摘要] 目的 探討分析影响慢性阻塞性肺疾病急性加重(AECOPD)合并Ⅱ型呼吸衰竭行有创机械通气治疗患者的预后因素。 方法 选择2013年10月~2015年4月收治的慢性阻塞性肺疾病急性加重合并Ⅱ型呼吸衰竭有创机械通气治疗患者的临床资料(包括年龄、性别、实验室指标、并发症及合并症等),根据此次住院的临床结局将研究对象分为存活组和死亡组,分析研究对象的各项临床资料,通过单因素和多因素Logistic回归分析,探讨影响其预后的独立因素。 结果 ①入院后两组血红蛋白、血尿素氮、血清清蛋白、有创机械通气后PaCO2下降率是否大于31.64%、并发呼吸机相关性肺炎、并发多脏器功能不全综合征比较,差异有统计学意义(P<0.05)。②有创机械通气后PaCO2下降率是否大于31.64%、并发呼吸机相关性肺炎、并发多脏器功能不全综合征是预后的独立影响因素,PaCO2下降率是其保护因素。 结论 AECOPD合并Ⅱ型呼吸衰竭行有创机械通气患者并发多脏器功能不全综合征、呼吸机相关性肺炎是预后不良的独立危险因素,而PaCO2下降率>31.64%则是保护因素。
[关键词] 慢性阻塞性肺疾病急性加重;Ⅱ型呼吸衰竭;有创机械通气;预后因素
[中图分类号] R563 [文献标识码] B [文章编号] 1673-9701(2020)28-0105-05
Analysis of prognostic factors of invasive mechanical ventilation in the treatment of acute exacerbation of chronic obstructive pulmonary disease complicated with type Ⅱ respiratory failure
MO Qiongya1 DONG Nian2 PAN Junjie1 LOU Yafang3
1.Department of Pulmonary and Critical Care Medicine, Hangzhou Dingqiao Hospital (Hangzhou Hospital of Traditional Chinese Medicine, Dingqiao Branch Hospital), Hangzhou 310000, China; 2.Department of Pulmonary and Critical Care Medicine, the First Affiliated Hospital of Wenzhou Medical University, Wenzhou 325015, China; 3.Department of Pulmonary and Critical Care Medicine, Hangzhou Hospital of Traditional Chinese Medicine, Hangzhou 310007, China
[Abstract] Objective To explore and analyze the prognostic factors of patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD) combined with type Ⅱ respiratory failure and who underwent invasive mechanical ventilation. Methods The clinical data (including age, gender, laboratory indicators, complications and comorbidities) of patients with acute exacerbation of chronic obstructive pulmonary disease and invasive mechanical ventilation treatment of type Ⅱ respiratory failure admitted from October 2013 to April 2015 were collected. According to the clinical outcome of this hospitalization, the study subjects were divided into survival group and death group. The clinical data of the study subjects were analyzed. Through single factor and multifactor logistic regression analysis, the independent factors affecting their prognosis were explored. Results ①There were significant differences in hemoglobin, blood urea nitrogen, serum albumin, whether the decrease rate of PaCO2 after invasive mechanical ventilation was greater than 31.64%, complicated ventilator-associated pneumonia, and complicated multiple organ dysfunction syndrome in both groups after admission(P<0.05). ②Whether the decrease rate of PaCO2 after invasive mechanical ventilation was greater than 31.64%, complicated ventilator-associated pneumonia, and multiple organ dysfunction syndrome were independent factors affecting prognosis, and the decrease rate of PaCO2 was its protective factor. Conclusion The complication with multiple organ dysfunction syndrome and ventilator-associated pneumonia in AECOPD combined with type Ⅱ respiratory failure patients with invasive mechanical ventilation are independent risk factors for poor prognosis, and the decrease rate of PaCO2 greater than 31.64% is a protective factor.
[Key words] Acute exacerbation of chronic obstructive pulmonary disease; Type Ⅱ respiratory failure; Invasive mechanical ventilation; Prognostic factors
慢性阻塞性肺疾病(Chronic obstructive pulmonary disease,COPD)是一种以不完全可逆的气流受限持续存在为特征的疾病,呈进行性发展。COPD患者病情进展,可导致生活质量下降,劳动力丧失,是目前公认的全球公共卫生问题[1]。
慢性阻塞性肺疾病急性加重(AECOPD)是指患者呼吸系统症状如咳嗽咳痰、胸闷气促等急性恶化,严重时可出现呼吸衰竭,AECOPD合并Ⅱ型呼吸衰竭是使用机械通气最常见的病因之一。根据已发表的文献资料,因急性加重收住ICU的COPD患者住院期间死亡率达15%以上,1年内死亡率为22%~43%[2-5]。多数文献报道死亡率的影响因素包括较高的年龄、低蛋白血症、合并症、肺源性心脏病、既往急性加重或住院病史、长期家庭氧疗和呼吸困难严重程度[2-6]。其他影响AECOPD患者远期生存率的危险因素还包括活动耐量低、胸部CT显示肺组织密度低和支气管管壁厚[7]。但COPD患者长期预后和近期预后的影响因素并不完全相同,许多长期预后因素如肺功能并不影响近期预后[8]。
本研究分析70例AECOPD合并Ⅱ型呼吸衰竭行有创机械通气治疗患者的临床资料,探讨其预后的影响因素,为重症AECOPD患者的治疗和管理提供依据。
1 资料与方法
1.1 一般资料
选择2013年10月~2015年4月收治的AECOPD合并Ⅱ型呼吸衰竭行有创机械通气治疗的患者70例为研究对象。其中男51例,女19例;年龄48~88岁,平均(75.09±8.37)岁。根据患者住院期间的临床结局,将研究对象分为存活组和死亡组。存活组指成功脱机,病情好转,遵医嘱离院的患者。死亡组包括在院内死亡及自动出院后24 h内死亡的患者。存活组50例,男34例,女16例;平均年龄(74.0±8.92)岁。死亡组20例,男性17例,女性3例,平均年龄(77.8±6.20)岁。两组患者一般资料比较,差异无统计学意义(P>0.05),具有可比性。
纳入标准:所有确诊病例均符合2014年中华医学会呼吸分会COPD分组制定的《慢性阻塞性肺疾病诊疗指南》(2013年修订版),此次因AECOPD入院,且合并2型呼吸衰竭。
排除标准:(1)胸廓畸形、免疫抑制或免疫缺陷、恶性肿瘤合并急性呼吸衰竭者。(2)此次发病前基础疾病不稳定或急性加重者。(3)临床资料不完整者。
1.2方法
所有病例均按照气管插管指征行有创机械通气,根据患者自主呼吸情况选择合适的通气模式。参数设置:潮气量(VT)6~8mL/kg,通气频率(f)12~20次/min,吸、呼气时间比(I:E)≤1:2,根据血氧饱和度(SaO2)调节给氧濃度(FiO2),使SaO2维持>90%,压力支持(PSV)10~20 cmH2O,呼气末正压(PEEP)4~6 cmH2O。在撤机过程中均采用SIMV+PSV模式,逐渐降低呼吸频率、PSV,逐步过渡到间歇使用呼吸机、撤机和拔管,部分患者予无创呼吸机支持。所有病例均进行常规综合治疗,包括抗炎、化痰、解痉平喘,纠正电解质及酸碱平衡紊乱,维持出入量平衡,同时予以营养支持。合理使用抗生素,积极处理伴随疾病及并发症。对极度焦虑、烦躁不安者适当予以镇静剂治疗。
1.3观察指标
观察入院24 h内血白细胞计数(White blood cell count,WBC)、血红蛋白(Hemoglobin,HGB)、血清清蛋白(Albumin,ALB)、血尿素氮(Blood urea nitrogen,BUN)、C反应蛋白(C-reactive protein,CRP),有创机械通气前后动脉血气分析指标(PaCO2、pH值、PaO2/FiO2)。观察有创机械通气治疗前是否有无创呼吸机支持治疗,入院治疗过程中是否发生并发症和合并症,如呼吸机相关性肺炎(Ventilator-associated pneumonia,VAP)、多脏器功能不全综合征(Multiple organ dysfunction syndrome,MODS)、拔管失败。
检测方法:①采集患者空腹外周静脉血5 mL,分离血清,采用Beckman全自动生化分析仪(Au5841)分析生化指标。②采集患者外周静脉血5 mL,使用同舸全自动血细胞分析仪(XE2100)检测血常规白细胞,采取免疫比浊法测定C反应蛋白(西门子全自动蛋白分析仪BNⅡ System)。③采集患者有创机械通气前后动脉血3 mL,采用雷度血气分析仪(ABL800)检测血气指标,氧分压(PaO2)、二氧化碳分压(PaCO2)、pH值、PaO2/FiO2。
1.4统计学方法
数据应用SPSS22.0统计学软件进行分析,计数资料用[n(%)]表示,采用χ2检验;符合正态分布的计量资料用(x±s)表示,组间比较采用t检验或t'检验(方差不齐时),组内比较采用配对t检验或t'检验(方差不齐时);非正态分布的计量资料用M(QL,QU)表示,组间比较采用非参数检验。秩相关两变量间相关性采用Spearman等级相关分析。采用单因素分析和多因素Logistic回归分析。采用ROC曲线评价相关因素对预后的预测作用。P<0.05为差异有统计学意义。
2 结果
2.1 两组患者血常规、CRP及生化指标比较
死亡组HGB、ALB均显著低于存活组(P<0.05),死亡组BUN显著高于存活组(P<0.05)。见表1。
[3] Nevins ML,Epstein SK.Predictors of outcome for patients with COPD requiring invasive mechanical ventilation[J].Chest,2001,119(6):1840-1849.
[4] Patil SP,Krishnan JA,Lechtzin N,et al.In-hospital mortality following acute exacerbations of chronic obstructive pulmonary disease[J].Arch Intern Med,2003,163(10):1180-1186.
[5] Ranieri P,Bianchetti A,Margiotta A,et al.Predictors of 6-month mortality in elderly patients with mild chronic obstructive pulmonary disease discharged from a medical ward after acute nonacidotic exacerbation[J].J Am Geriatr Soc,2008,56(5):909-913.
[6] Matkovic Z,Huerta A,Soler N,et al.Predictors of adverse outcome in patients hospitalised for exacerbation of chronic obstructive pulmonary disease[J].Respiration,2012, 84(1):17-26.
[7] Singanayagam A,Schembri S,Chalmers JD.Predictors of mortality in hospitalized adults with acute exacerbation of chronic obstructive pulmonary disease[J].Ann Am Thorac Soc,2013,10(2):81-89.
[8] Kaelin RM,Assimacopoulos A,Chevrolet JC.Failure to predict six-month survival of patients with COPD requiring mechanical ventilation by analysis of simple indices.A prospective study[J].Chest,1987,92(6):971-978.
[9] Connors AFJ,Dawson NV,Thomas C,et al.Outcomes following acute exacerbation of severe chronic obstructive lung disease.The SUPPORT investigators(Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments)[J].Am J Respir Crit Care Med,1996,154(4Pt1):959-967.
[10] Safdar N,Dezfulian C,Collard HR,et al.Clinical and economic consequences of ventilator-associated pneumonia:A systematic review[J].Crit Care Med,2005,33(10):2184-2193.
[11] Muscedere JG,Martin CM,Heyland DK.The impact of ventilator-associated pneumonia on the Canadian health care system[J].J Crit Care,2008,23(1):5-10.
[12] Koulenti D,Blot S,Dulhunty JM,et al.COPD patients with ventilator-associated pneumonia:Implications for management[J].Eur J Clin Microbiol Infect Dis,2015,34(12):2403-2411.
[13] 中華医学会重症医学分会.呼吸机相关性肺炎诊断、预防和治疗指南(2013)[J].中华内科杂志,2013,52(6):524-543.
[14] Hurst JR,Perera WR,Wilkinson TM,et al.Systemic and upper and lower airway inflammation at exacerbation of chronic obstructive pulmonary disease[J].Am J Respir Crit Care Med,2006,173(1):71-78.
[15] Shimada H,Moriwaki Y,Kurosawa H,et al.Inflammatory mediator and organ dysfunction syndrome[J].Nihon Geka Gakkai Zasshi,1998,99(8):490-496.
[16] Liu H,Zhang T,Ye J.Determinants of prolonged mechanical ventilation in patients with chronic obstructive pulmonary diseases and acute hypercapnic respiratory failure[J].Eur J Intern Med,2007,18(7):542-547.
[17] Afessa B,Morales IJ,Scanlon PD,et al.Prognostic factors,clinical course,and hospital outcome of patients with chronic obstructive pulmonary disease admitted to an intensive care unit for acute respiratory failure[J].Crit Care Med,2002,30(7):1610-1615.
[18] Calverley PM,Anderson JA,Celli B,et al.Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease[J].N Engl J Med,2007,356(8):775-789.
[19] Xiao K,Guo C,Su L,et al.Prognostic value of different scoring models in patients with multiple organ dysfunction syndrome associated with acute COPD exacerbation[J].J Thorac Dis,2015,7(3):329-336.
[20] Khamiees M,Raju P,Degirolamo A,et al.Predictors of extubation outcome in patients who have successfully completed a spontaneous breathing trial[J].Chest,2001, 120(4):1262-1270.
(收稿日期:2019-09-18)
