Effects of denosumab treatment in chronic liver disease patients with osteoporosis
2020-10-29ChisatoSaekiMitsuruSaitoTsunekazuOikawaMasanoriNakanoYuichiTorisuMasayukiSarutaAkihitoTsubota
Chisato Saeki, Mitsuru Saito, Tsunekazu Oikawa, Masanori Nakano, Yuichi Torisu, Masayuki Saruta, Akihito Tsubota
Abstract
Key words: Chronic liver disease; Denosumab; Osteoporosis; Bone mineral density; Bone turnover; Bone quality
INTRODUCTION
Osteoporosis is a frequent complication in patients with chronic liver disease (CLD), particularly in those with liver cirrhosis (LC) and primary biliary cholangitis[1-4]. Osteoporosis can cause fragility fractures, thereby increasing morbidity and decreasing health-related quality of life in CLD patients[5]. Therefore, early diagnosis and effective treatment of osteoporosis are crucial in preventing fragility fracture and maintaining health-related quality of life.
In terms of tissue material properties, bone mineral density (BMD) and bone quality are essential for determining bone strength[6-8]. Bone mineralization, which is regulated mainly by bone remodeling, provides stiffness to the bones, whereas collagen fibers influence the tensile strength, ductility, and toughness of the bones[7,8]. Collagen crosslink formation, a post-translational modification of collagen, plays an important role in the material level of bone quality[7,8]. The formations of collagen cross-links are classified into two types: Enzymatic and non-enzymatic cross-links. Enzymatic crosslinks induced in an enzyme-dependent manner and produced by osteoblasts promote ductility and strength as well as bone mineralization. In contrast, non-enzymatic crosslinks represented by advanced glycation end products (AGEs), which are induced by glycation and oxidant stress, impair the function of osteoblasts and bone’s mechanical properties. Therefore, impaired enzymatic cross-links and/or accelerated nonenzymatic cross-links in bone collagen deteriorate ductility and increase bone fragility[7,8]. Pentosidine is a biomarker for AGEs that accumulate in bone with increasing age and enhance the bone resorption activities of osteoclasts[9,10]. Urinary and serum pentosidine levels were reported to be positively and independently correlated to fractures in postmenopausal women and diabetic patients[11-14]and are now being used to estimate fracture risk in patients with osteoporosis and diabetes.
Receptor activator of nuclear factor kappa-B ligand (RANKL), also known as tumor necrosis factor-related activation-induced cytokine and osteoprotegerin ligand, is expressed on various cells including osteoblasts, binds to the receptor RANK on osteoclasts and precursors surfaces, and promotes differentiation and activation of osteoclasts, which are involved in bone resorption[15,16]. Osteoprotegerin (OPG) is expressed on several cells including osteoblasts, serves as a soluble decoy receptor for RANKL, and interrupts the interaction between RANK and RANKL by competing with RANK, suppressing osteoclastogenesis and bone resorption[15]. Hence, the RANK/RANKL/OPG signaling pathway plays a critical role in regulating bone resorption by osteoclasts and bone formation by osteoblasts.
Denosumab is a human monoclonal antibody with high affinity and specificity for RANKL and mimics the endogenous effect of OPG, thereby inhibiting bone resorption and remodeling[17,18]. Reportedly, denosumab increased BMD and decreased the levels of bone turnover markers, leading to a reduction in the osteoporotic fracture risk in postmenopausal women[19-24]. Furthermore, long-term treatment with denosumab was proved safe and associated with low bone remodeling rates and a constant increase in BMD without reaching a plateau[24]. Therefore, denosumab has attracted attention as an effective osteoporosis treatment that improves health-related quality of life[25]. However, there are few reports evaluating the efficacy of denosumab in CLD patients.
The aim of this study was to clarify the effects of denosumab treatment on BMD, bone turnover, and bone quality in CLD patients with osteoporosis.
生理生化特征试验结果显示(表5),菌株CEH-ST79有过氧化氢酶、氧化酶、β-半乳糖苷酶、硝酸盐还原、明胶液化、淀粉水解和酪蛋白测定均为阳性,精氨酸双水解酶、精氨酸脱羧酶、H2S产生、水杨素、吲哚、溶血和脲酶测定为阴性。
MATERIALS AND METHODS
Study design and patients
This was a retrospective study of denosumab treatment for osteoporosis, which was conducted at the Jikei University School of Medicine (Tokyo, Japan) and Fuji City General Hospital (Shizuoka, Japan). A total of 60 CLD patients met the inclusion criteria and initiated denosumab treatment between 2017 and 2019. The inclusion criteria were as follows: (1) Presence of CLD with any etiology (hepatitis B or C, alcoholic liver disease, autoimmune hepatitis, primary biliary cholangitis, or nonalcoholic steatohepatitis); (2) Presence of osteoporosis diagnosed according to the World Health Organization criteria (T score ≤ -2.5); (3) No history of osteoporosis treatment; and (4) Subjects receiving denosumab treatment over 12 mo. The exclusion criteria were as follows: (1) Hypocalcemia (defined as serum calcium concentration < 8.5 mg/dL); (2) Subjects with glucocorticoid use; and (3) Subjects constantly receiving dental treatment. Denosumab was subcutaneously administered at a dose of 60 mg once every 6 months in combination with daily oral supplements of 610 mg of calcium and vitamin D [400 IU of cholecalciferol (native vitamin D) for patients with an estimated glomerular filtration rate ≥ 35 mL/min/1.73 m2or 0.75 µg of eldecalcitol (active vitamin D) for those with estimated glomerular filtration rate < 35 mL/min/1.73 m2]. Although the study period was 12 mo, denosumab treatment is ongoing.
LC was diagnosed based on laboratory tests, morphological assessment with imaging (ultrasonography, computed tomography, and/or magnetic resonance), and/or the presence of esophageal/gastric varices confirmed using upper gastrointestinal endoscopy. BMD at the lumbar spine (L2-L4), femoral neck, and total hip was evaluated at 0 and 12 mo of treatment. Serum tartrate-resistant acid phosphatase-5b (TRACP-5b; bone resorption marker) and total procollagen type I Nterminal propeptide (P1NP; bone formation maker) were measured at 0, 1, 3, 6, and 12 mo. Plasma pentosidine (bone quality marker) was measured at 0 and 12 mo. Hypocalcemia was graded according to the Common Terminology Criteria for Adverse Events version 5.0. This study was conducted in accordance with the Declaration of Helsinki and was approved by the ethics committee of the Jikei University School of Medicine (approval No. 28-194) and Fuji City General Hospital (approval No. 162). Written informed consent was obtained from all patients.
End points
The primary end point included changes from baseline to 12 mo of treatment in BMD at the lumbar spine, femoral neck, and total hip. The secondary end point included changes from baseline to 12 mo of treatment in bone turnover (serum TRACP-5b and P1NP) and quality (plasma pentosidine) markers.
Assessment of bone mineral density and fractures
BMD was assessed at the lumbar spine (L2-L4), femoral neck, and total hip using dualenergy X-ray absorptiometry (PRODIGY; GE Healthcare, Madison, WI, United States). Osteoporosis was diagnosed according to the World Health Organization criteria (Tscore ≤ -2.5 for osteoporosis, between -2.5 and -1.0 for osteopenia, and > -1.0 for normality)[26]. Vertebral fractures were evaluated using spinal lateral X-rays at baseline and 12 mo of treatment.
Clinical and laboratory assessment
A blood sample was obtained from each patient after overnight fasting. Serum aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, gammaglutamyltransferase, albumin, and total bilirubin were measured using routine laboratory methods. Serum TRACP-5b, serum P1NP, and plasma pentosidine were measured using enzyme immunoassay (SB Bioscience, Tokyo, Japan), electrochemiluminescence immunoassay (Roche Diagnostics, Tokyo), and enzymelinked immunosorbent assay (FUSHIMI Pharmaceutical, Kagawa, Japan), respectively.
Statistical analysis
Continuous variables are represented as medians and interquartile ranges. The Mann-WhitneyUtest was used to compare continuous variables between the two groups. The Wilcoxon signed rank test and Friedman test were used to compare changes in treatment-related biomarkers over time. Categorical variables are represented as the number of patients and percentages. Statistical analyses were performed using SPSS version 26 software (IBM, Armonk, NY, United States). APvalue of < 0.05 was considered statistically significant.
RESULTS
Patient characteristics
Among the 405 CLD patients who underwent the assessment of BMD, 138 patients were diagnosed with osteoporosis; among these, 78 patients met the exclusion criteria and thus were excluded from this study. Therefore, 60 patients were finally included in the analysis (Figure 1).
The baseline clinical characteristics of the 60 patients enrolled in this study are shown in Table 1. The median age of the patients was 74.0 (68.5–79.8) years. The study included 47 female patients (78.3%). Twenty-five patients (41.7%) had LC. The number of patients with history of osteoporotic fracture was 25 (41.7%). The median BMD values at the lumber spine, femoral neck, and total hip were 0.84 (0.76–0.94) g/cm2, 0.61 (0.56–0.66) g/cm2, and 0.67 (0.59–0.71) g/cm2, respectively. Only one patient was treated with denosumab in combination with oral eldecalcitol due to chronic kidney disease.
Efficacy of denosumab treatment on bone mineral density
Next, we compared the changes from baseline in BMD between men and women, between patients aged < 65 years and ≥ 65 years, and between LC and non-LC groups (Figure 3A-C, Table S2-S4). The BMD values in all groups except for femoral neck BMD in men were significantly improved at 12 mo of treatment (Table S2-S4). However, the percentage changes were not significantly different between any two groups (Figure 3A-C). These findings indicate that denosumab treatment significantly improved BMD, irrespective of gender, patient age, and presence/absence of LC.

Table 1 Baseline characteristics of the patients, n (%)
Efficacy of denosumab treatment on bone turnover and quality markers
The changes in bone turnover and quality markers during denosumab treatment are shown in Figure 4 and Table S5. The median serum TRACP-5b level was 533 mU/dL at baseline and rapidly decreased by 77.7% at 1 mo of treatment and remained at a similar level thereafter (Figure 4A, Table S5). The median serum P1NP level was 57 ng/mL at baseline and gradually decreased by 22.8% at 1 mo and 68.4% at 3 mo, and remained at a similar level thereafter (Figure 4B, Table S5). There was little or no change in the serum calcium concentration during denosumab treatment (Figure 4C, Table S5). The median plasma pentosidine level was 0.0584 μg/mL at baseline and significantly decreased at 12 months (0.0501 μg/mL;P= 0.010) (Figure 4D, Table S5).
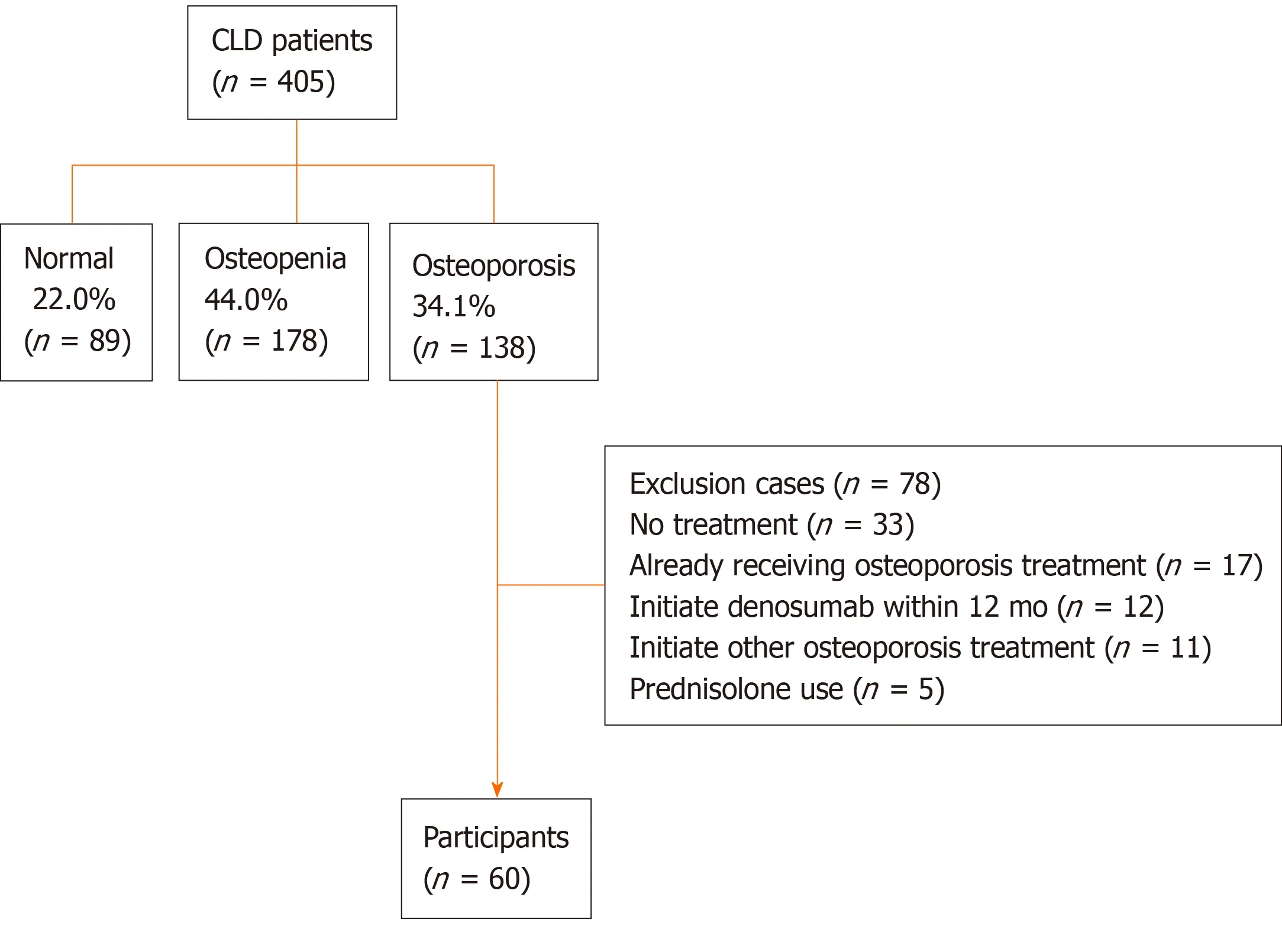
Figure 1 Flow diagram of patients enrolled in the present study. Bone mineral density was assessed at the lumbar spine (L2-L4), femoral neck, and total hip in 405 chronic liver disease patients. One hundred thirty-eight patients were diagnosed with osteoporosis (34.1%); among these, 78 patients met the exclusion criteria and 60 patients were finally included in the present study. CLD: Chronic liver disease.

Figure 2 Bone mineral density values and proportion of bone mineral density response categories based on the bone mineral density percentage changes. A: Bone mineral density (BMD) values at the lumbar spine, femoral neck, and total hip at baseline and 12 mo of denosumab treatment. Deltas and percentages represent median change rates from baseline to 12 mo. aP < 0.001 compared to baseline; B: The proportion of BMD response categories based on the BMD percentage changes from baseline to 12 mo of denosumab treatment at the lumbar spine, femoral neck, and total hip. BMD: Bone mineral density.
Safety and adverse events
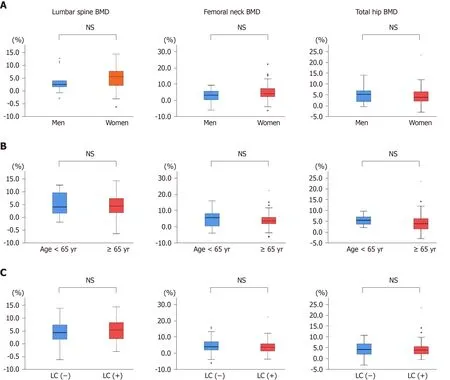
Figure 3 Comparison of the median percentage changes from baseline to 12 mo of denosumab treatment in bone mineral density at the lumbar spine, femoral neck, and total hip. A: Men and women; B: Patients aged < 65 years and ≥ 65 years; C: Patients with and without liver cirrhosis. There were no significant differences between the groups. NS: Not significant; BMD: Bone mineral density; LC: Liver cirrhosis.
The incidence of hypocalcemia (< 8.5 mg/dL) was 11.7 % (7 of the 60 patients): 4 incidents occurred at 1 mo, 2 at 3 mo, and 1 at 12 mo of treatment. Two of the hypocalcemic patients were non-compliant with calcium and vitamin D supplementation. All cases were asymptomatic and classified as grade 1 hypocalcemia, with levels returning to the normal range without additional treatment. No patients experienced any fractures or other moderate-to-severe adverse events during the 12-mo study period.
DISCUSSION
Osteoporosis, resulting in frequent fractures and leading to significant morbidity, is a common complication in CLD[1-5]. Therefore, an appropriate treatment for osteoporosis is essential for improving health-related quality of life in CLD patients. In the present study, we demonstrated that denosumab significantly improved BMD in CLD patients, regardless of gender, patient age, and presence/absence of liver cirrhosis. The median percentage changes from baseline to 12 mo of treatment in BMD at the lumbar spine, femoral neck, and total hip were +4.44%, +3.71%, and +4.03%, respectively, in the present study; they were +5%–6%, +2%–3%, and +2%–3.5%, respectively, in previous reports for men and postmenopausal women with primary osteoporosis[28-30]. In a large phase 3 trial for primary osteoporosis, 10-year denosumab treatment increased BMD by +21.7%, +9.2%, and +9.0%, respectively[24]. A recent pilot study for a small number of patients with autoimmune liver disease showed that 3-year denosumab treatment significantly improved BMD without any adverse events[31]. These findings suggest that denosumab treatment is effective for osteoporosis in CLD patients. The present study is the first to highlight the efficacy of denosumab in treating osteoporosis in CLD patients.
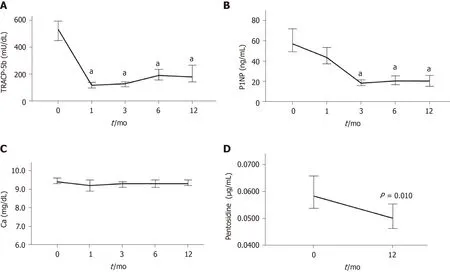
Figure 4 Time-course changes from baseline to 12 mo of denosumab treatment. A: In the levels of serum tartrate-resistant acid phosphatase 5b; B: Serum procollagen type N-terminal propeptide; C: Serum calcium; and D: Plasma pentosidine. aP < 0.001 vs baseline.
According to the definition of osteoporosis, bone strength is determined by both BMD and bone quality[7,8]. BMD depends mainly on bone remodeling, whose status is reflected by bone turnover markers. Bone quality is determined by enzymatic and non-enzymatic collagen cross-links. Increased AGE cross-links (e.g., pentosidine as its surrogate biomarker) have been proposed as a major cause of bone fragility[7,8]. Reportedly, pentosidine levels in the cortical and cancellous bones of patients with femoral neck fracture were higher than those in age-matched controls[32,33]. Higher serum and urine pentosidine levels were associated with increased fracture risk and incidence of vertebral fractures in diabetic patients[12,14]. Furthermore, serum and bone pentosidine levels were higher in patients with hip fractures than in those with osteoarthritis; additionally, a significant, positive correlation was found between serum and bone pentosidine levels in the fracture patients[34]. These results suggest that pentosidine could be a useful biomarker for estimating bone quality.
In the present study, TRACP-5b declined sharply at 1 mo of denosumab treatment and was sustained thereafter, whereas P1NP declined gradually and reached the nadir at 3 mo of treatment. These pharmacokinetic profiles are consistent with those reported in previous studies[20,35]. Meanwhile, the present study is the first to demonstrate that denosumab significantly reduced plasma pentosidine levels in CLD patients, given that only few studies have investigated the effect of denosumab on bone quality markers. Similar findings were observed in denosumab treatment for prostate cancer patients receiving androgen deprivation therapy[36]. Taken together, denosumab treatment could not only efficiently modify bone remodeling in the early phase of the treatment but also improve bone quality in terms of tissue material properties.
Long-term denosumab treatment constantly increased BMD without reaching a plateau, despite persistently reduced bone turnover markers, and seemed to be more effective than bisphosphonate (BP)[24,37]. In the ovariectomized cynomolgus monkeys study, denosumab induced continuous modeling-based bone formation in the cortical bone, which indicates the increase of the content of enzymatic immature and mature cross-links, and continuously increased BMD, despite the reductions of bone resorption and formation biomarkers[38]. Similarly, administration of parathyroid hormone (1-34) (teriparatide), which stimulates bone formation, increased the content of enzymatic cross-links, bone volume, and trabecular thickness, and decreased pentosidine (non-enzymatic AGE cross-links), leading to improvement of bone strength, in ovariectomized monkeys[39]. In contrast, BP treatment increases BMD with reaching a plateau[37], and long-term suppression of bone remodeling (bone resorption and formation) increased pentosidine levels in dogs and humans[40,41]. Taken together, denosumab treatment may not impede the bone formation and increases the content of enzymatic cross-links, which could contribute to the reduction of non-enzymatic AGE cross-links (such as pentosidine) and improvement of bone quality and strength.
Adherence to osteoporosis medication is a critical issue, given that low compliance is associated with a higher risk of osteoporotic fractures[42]. Indeed, approximately 50% of patients treated with oral BP discontinued their prescribed treatment regimen within one year[42,43]. However, denosumab users had better 1-year and 2-year adherence than weekly oral BP users[43]. Hence, denosumab treatment is a recommended therapeutic option for CLD patients with osteoporosis.
During the 12-mo study period, no patients experienced any fractures or moderateto-severe adverse events. Hypocalcemia was observed in 11.7% (7 of the 60 patients) and mainly developed in the early phase after the first dosing, which was similar to results in a previous report[44]; however, it was asymptomatic, transient, and mild (grade 1). Thus, denosumab treatment was safe in CLD patients.
This study had some limitations. First, the sample size was not large enough to evaluate the efficacy of denosumab in each subgroup. Second, given that the study period of 12 mo was short, we could not clarify the long-term treatment outcomes (such as fragility fractures and health-related quality of life) and adverse events associated with long-term administration. Third, given that this was not a randomized control study to evaluate the efficacy of denosumab versus BP, we could not demonstrate the real differences in CLD patients with osteoporosis.
CONCLUSION
In conclusion, denosumab increased BMD, suppressed bone turnover, and improved bone quality marker levels in CLD patients with osteoporosis, irrespective of gender, patient age, and presence/absence of liver cirrhosis. Given that denosumab treatment is effective and safe, it is a beneficial treatment option for osteoporosis in CLD patients. A large-scale, long-term, randomized controlled study is needed to confirm these findings.
ARTICLE HIGHLIGHTS


Research results
BMD values at the lumbar spine (+4.44%), femoral neck (+3.71%), and total hip (+4.03%) were significantly improved at 12 mo of treatment, regardless of differences in baseline characteristics. Denosumab treatment significantly suppressed bone turnover markers and improved a bone quality marker at 12 mo. No patients experienced fractures and adverse events, except for transient hypocalcemia.
Research conclusions
Denosumab treatment is effective and safe even in CLD patients with osteoporosis. Thus, denosumab is a beneficial treatment option for osteoporosis in CLD patients.
Research perspectives
This study opened up new possibilities for osteoporosis treatment in CLD patients. Specifically, it is noteworthy that denosumab treatment improved a bone quality marker along with BMD. A large-scale, randomized controlled study is needed to confirm the long-term effects of denosumab.
ACKNOWLEDGEMENTS
We thank the medical staff at Jikei University School of Medicine and Fuji City General Hospital for data collection.
猜你喜欢
杂志排行
World Journal of Gastroenterology的其它文章
- Bowel function and quality of life after minimally invasive colectomy with D3 lymphadenectomy for rightsided colon adenocarcinoma
- Treatment repurposing for inflammatory bowel disease using literature-related discovery and innovation
- Neutrophil to lymphocyte ratio and albumin bilirubin grade in hepatocellular carcinoma: A systematic review
- Radiomics of rectal cancer for predicting distant metastasis and overall survival
- Liver fat accumulation measured by high-speed T2-corrected multi-echo magnetic resonance spectroscopy can predict risk of cholelithiasis
- Exploring the food-gut axis in immunotherapy response of cancer patients
