Neutrophil to lymphocyte ratio and albumin bilirubin grade in hepatocellular carcinoma: A systematic review
2020-10-29AymanBannagaRameshArasaradnam
Ayman Bannaga, Ramesh P Arasaradnam
Abstract
Key words: Hepatocellular carcinoma; Albumin bilirubin Grade; Neutrophil to lymphocyte ratio; Alpha fetoprotein; Prognosis; Survival
INTRODUCTION
Hepatocellular carcinoma (HCC) is the final sequel of chronic liver disease (CLD) with increasing incidence worldwide. The most common causes of chronic liver disease are related to alcohol abuse and chronic viral hepatitis infections (B and C). In the western hemisphere, the incidence is notably increasing following the rise of non-alcoholic fatty liver disease. Early noninvasive diagnostic methods to identify HCC are lacking in primary care. Most of the patients present late with an advanced stage of the disease, which is manifested in poor clinical outcomes[1,2].
The main system used to estimate the liver function in HCC patients is the Child Turcotte Pugh (CTP). This score was created in the early 1970s as a method for prognostication of CLD[3,4]. CTP scoring rely on five parameters namely, Bilirubin, Albumin, International Normalised Ratio, Ascites, and Encephalopathy. The last two parameters are dependent on physical examination; this is of course is quite variable between clinicians. While CTP score can be useful in prognostication, a score like the Model For End-Stage Liver Disease (MELD) was shown to have better prognostic value in CLD[5,6].
HCC prognostic staging systems integrated CTP in addition to imaging results and the comorbid status of the patient. The main staging systems used in HCC include the Barcelona Clinic Liver Cancer (BCLC), Cancer of Liver Italian Program, Hong Kong Liver Cancer staging system, the Japanese Tumour Node Metastasis staging system for primary liver cancer[1,2].
HCC literature continues to report on studies from around the world aiming to find simpler prognostic markers for the disease. Linear predictive models generated from large data sets were shown to be able to prognosticate for HCC patients[7,8]. Indeed, simpler prognostic ways are required given the complexity of the intermediate stage of HCC[9]. The emerging literature describes two new markers in HCC prognosis, the Neutrophil to Lymphocyte Ratio (NLR) and the Albumin Bilirubin (ALBI) grade.
NLR is a simple and generic way to look into the cellular immune response and is considered a measure of the physiologic response of the body to different stressful factors[10]. NLR was described to be a prognostic factor in many liver diseases. In nonalcoholic fatty liver disease, NLR was associated with inflammatory activity and different histological fibrotic grades[11-15]. In chronic viral hepatitis B and C, NLR predicted response to anti-viral therapy[16-21]. In cirrhosis, NLR was associated with worse outcomes[22-27]. In alcoholic hepatitis, NLR predicted mortality and identified patients likely to require steroid treatment[28,29]. In primary biliary cholangitis, NLR predicted one-year mortality[30,31]. NLR was also studied in liver transplantation and found to be correlated with poor prognosis and graft dysfunction[32-38]. It is also important to note that NLR was also described to be prognostic in the gastrointestinal, renal tract, lung, and breast cancers[39-56]. Furthermore, miscellaneous studies Identified NLR to be associated with colorectal adenoma, tinnitus, hyperemesis gravidarum, hypertensive renal disease, acute appendicitis, and bacterial and viral infections[57-65].
Albumin Bilirubin grade was described in 2015 by Johnsonet al[66]. It is a mathematical model for assessment of liver function in patients with hepatocellular carcinoma based on data from 1313 Japanese patients. ALBI uses the numerical values of both albumin and bilirubin to measure the distance/relation of these values to the overall prognosis of HCC. Johnsonet al[66], identified that ALBI = (log10 bilirubin × 0.66) + (albumin × -0.085), where bilirubin is in μmol/L and albumin in g/L. ALBI has three grades; ALBI ≤ -2.60 or Grade 1, ALBI > -2.60 to ≤ -1.39 or Grade 2 and ALBI > -1.39 or grade 3.
This systematic review aimed to evaluate the studies published over the last five years in relation to the use of NLR and ALBI grade as prognostic indicators in HCC. Additionally, we also evaluated the performance of NLR and ALBI locally in our centre.
MATERIALS AND METHODS
We searched PubMed using the following MeSH Terms “neutrophil to lymphocyte ratio liver” and “albumin bilirubin grade” on February 5, 2020 covering the last 5 years. Following the initial search, all articles were retrieved. The checklist of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses was instituted in this review. We further applied the Problem, Intervention, Comparison Outcome (PICO) criteria to filter the retrieved articles, by identifying the problem as HCC patients, interventions as NLR/ALBI, comparators as conventional prognostic scores/systems and outcome as the described prognosis in the clinical studies.
In addition to the systematic search, we also looked into our local results concerning HCC, NLR, and ALBI in our centre. We retrospectively analysed all HCC cases between December 2013 and December 2018. The analysis was done using the IBM SPSS Statistics software version 25. We looked into the baseline characteristics of the patients. Survival analysis was performed using the Kaplan-Meier method and the log-rank test. Bivariate analysis was performed to detect the correlation between different variables and survival using the Independent Samplest-test to compare the means between independent groups. We also performed receiver operating characteristic analysis between the ALBI grades, and CTP scores and death from HCC.
RESULTS
NLR and ALBI in HCC
The initial systematic search revealed 430 articles related to NLR. After applying the PICO criteria 376 NLR articles were excluded, leaving 54 studies describing the relation between HCC and NLR (Table 1)[67-121]. Furthermore, there were 348 articles related to ALBI and after applying the PICO criteria, 253 articles were excluded leaving 95 studies describing the relation between HCC and ALBI (Table 2)[66,122-216].
HCC outcomes and validation of NLR and ALBI in our centre
Given the strong evidence around NLR and ALBI as demonstrated in (Table 1 and Table 2), we aimed to validate these prognostic indicators in our patients. Between December 2013 and December 2018, a total of 121 HCC patients was identified using the hospital informatics systems. We evaluated their clinical notes, test results, treatment, survival post treatment and overall survival since the diagnosis was made. Overall survival was calculated for each patient by calculating the time when the case was first discussed in the local hepato-pancreaticobiliary (HPB) multidisciplinary team (MDT) meeting till the end of collecting the data on September 3, 2019. The HPB-MDT meeting is formed by HPB surgeon, hepatologist, oncologist, histopathologist and interventional liver radiologist.
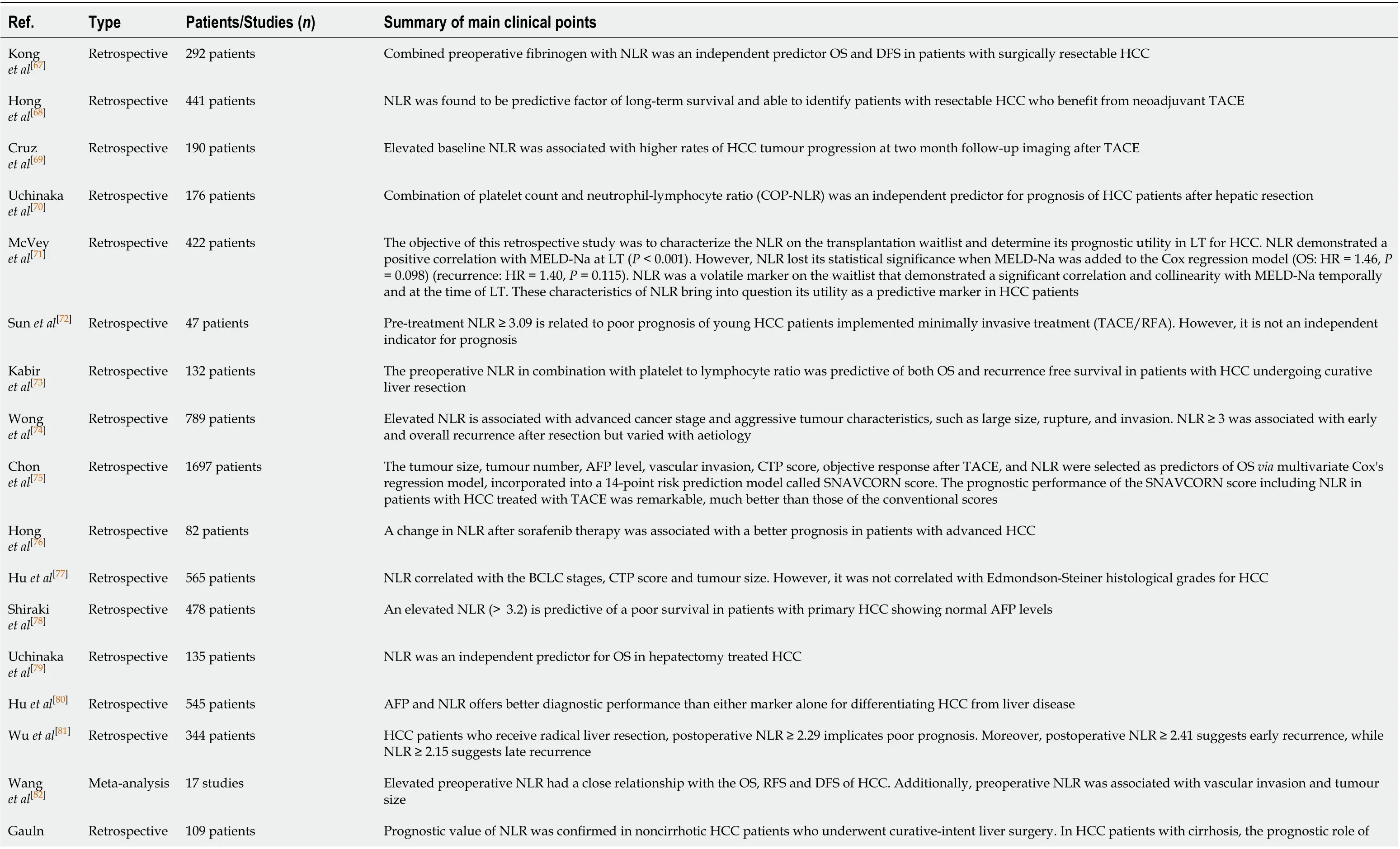
Table 1 studies describing the relation between hepatocellular carcinoma and Neutrophil to Lymphocyte Ratio in the last 5 years

et al[83]NLR was not confirmed Qi et al[84]Meta-analysis 20475 patients; 90 studies Low baseline NLR was significantly associated with better OS, RFS and DFS. Low post treatment NLR was significantly associated with better OS. Decreased NLR was significantly associated with OS, RFS and DFS Tan et al[85]Retrospective 402 Pre-ablation NLR was a valuable predictor in locally advanced HCC patients treated with RFA. NLR ≥ 2.2 indicated a poor prognosis Najjar et al[86]Systematic review 7902 patients with liver resection; 2929 patients with liver transplantation Pretransplant NLR was most often predictive of HCC recurrence, RFS and OS. NLR was, however, more variably and less clearly associated with worse outcomes following liver surgical resection Xu et al[87]Meta-analysis 13 studies 1936 patients Elevated pretransplant NLR had a close association with the OS, RFS DFS of patients undergoing liver transplantation for HCC, respectively. In addition, elevated NLR was associated with the presence of vascular invasion and Milan criteria Chen et al[88]Retrospective 287 patients The combination of the NLR and the PLR, for predicting the survival time of patients with HCC who had received RFA was associated with developing distant intrahepatic recurrence, extrahepatic metastasis, shorter OS and RFS Lué et al[89]Retrospective 154 patients NLR was found to be an independent prognostic indicator for OS in HCC patients treated with sorafenib Liu et al[90]Retrospective 760 patients Combination of the NLR to the aspartate aminotransferase-to-alanine aminotransferase ratio was found to be an independent marker of poor prognosis in patients with HCC receiving TACE Margetts et al[91]Retrospective 1168 patients Neutrophils alone, rather than lymphocytes, were independently associated with outcome Min et al[92]Meta-analysis 12979 patients Elevated NLR had a close relationship with OS and DFS of liver cancer. It was also associated with tumour vascular invasion, multiple tumours, AFP ≥ 400 ng/ML, presence of HBV S Ag and cirrhosis Liu et al[93]Retrospective 793 patients NLR plus prognostic nutritional index score had superior discriminative abilities, compared with either the NLR or PNI alone in predicting the outcomes of patients with unresectable HCC after TACE Hung et al[94]Retrospective 672 patients In patients who had curative liver resection for HCC, NLR > 2.5 had larger tumour size, higher histology grade, and higher rates of tumour multiplicity and vascular invasion. After a median follow up of 76.3 mo, 437 (65.0%) patients had tumour recurrence. When patients had tumour recurrence, 5-year post-recurrent survival was best in the patients staying with NLR ≤ 2.5 Li et al[95]Retrospective 724 patients In HCC patients undergoing curative resection a prognostic index model, NγLR = [neutrophil count (109/L) × γ-glutamyl transpeptidase (U/L)]/[(lymphocyte count) (109/L) × U/L], was selected. Elevated NγLR predicted a worse OS and progression-free survival (PFS) for HCC patients Jin et al[96]Retrospective 556 patients Platelet times neutrophil to lymphocyte ratio in hepatitis B related HCC within BCLC stage A was found to be a prognostic indicator of poor outcomes Zhang et al[97]Retrospective 756 patients Investigated the outcome of synchronous hepatectomy and splenectomy in HCC. Splenectomy and NLR were found to be significant independent prognostic factors Li et al[98]Retrospective 81 patients The preoperative NLR is a prognostic predictor after hepatectomy for HCC patients with portal/hepatic vein tumour thrombosis. NLR > 2.9 indicated poorer OS and DFS Liu et al[99]Prospective 160 patients Elevated NLR is associated with the pathogenesis and progression of HBV related HCC. The study also identified that there was also reduced thymic output and hyperactivation of T lymphocytes which may contribute to the decrease of T lymphocytes, which could be also related to the pathogenesis of HBV related HCC Son et al[100]Retrospective 56 patients Low NLR was significantly associated with better PFS and OS in patients with locally advanced HCC treated with radiotherapy Taussig et al[101]Prospective 86 patients In 86 HCC treatment-naïve patients who had chemoembolization or radioembolization, NLR was found to be associated with early progressive disease after intra-arterial therapy of HCC Yang et al[102]Retrospective 1020 patients NLR found to be independent prognostic factor for DFS in HCC patients undergoing hepatectomy

NLR: Neutrophil to lymphocyte ration; OS: Overall survival; DFS: Disease free survival; HCC: Hepatocellular carcinoma; TACE: Transarterial chemoembolization; LT: Liver transplantation; MELD-Na: Model for end-stage liver disease-Na; RFA: Radiofrequency ablation; PLR: Platelet to lymphocyte ratio; RFS: Recurrence free survival ; CTP: Child Turcotte Pugh score ; BCLC: Barcelona clinic liver cancer staging system; AFP: Alpha fetoprotein; HBV: Hepatitis B virus; SIRT: Selective internal radiation therapy.
HCC diagnosis was based on the identification of the typical hallmarks of HCC, which differed according to the imaging techniques or contrast agents used. All patients had an initial abdominal ultrasound scan either in our hospital or from a referring centre (general practice centre or district hospital). Initial computed tomography scan was used to make the radiological diagnosis. In case of any uncertainty, a dynamic contrast-enhanced MRI was done. 54 patients (44.6%) were diagnosed by HCC features on computed tomography scan while 67 (55.4%) patients were diagnosed with liver MRI features.
Commonest symptoms that patients presented with were abdominal pain and weight loss. Raised alpha fetoprotein (AFP) was found in 68 patients (> 10 KU/L). 82 patients (67.8%) had radiological features of liver cirrhosis. Majority of the patients had relatively good liver function as per CTP score (Table 3). Oesophageal varices and ascites were present in 36 patients (29.8%) and 29 patients had splenomegaly (24%). Patients were staged using the BCLC system (Table 3). Raised AFP (> 10 KU/L) was found in 68 patients (33 patients with AFP > 100KU/L, and 33 patients > 300KU/L). Normal AFP (AFP < 10 KU/L) was found in 53 patients. 50 patients had confirmatory histology for HCC leaving the sensitivity of AFP in comparison to histology to be low at 44%. Morphological characteristics of the HCC are described in (Table 3).
Current HCC treatment modalities available at our centre include liver surgery, radiofrequency ablation (RFA), transarterial chemoembolisation (TACE), palliative chemotherapy (Sorafenib). For the liver transplant, patients were transferred to a nearby national transplant centre and then followed up in our hospital. Curative treatment (liver resection, RFA and/or liver transplant) was done in 13.2% of the patients. Non curative treatment (TACE and Sorafenib) was done in 41.3% of the patients. The rest of the patients (45.5%) were offered the best supportive care due to their late presentation at the time of diagnosis.
There were 10 patients that were referred for a liver transplant, 4 were transplanted. Among the other 6 liver transplant referrals two were denied a transplant because continued alcohol consumption. Three patients were denied a liver transplant because the tumour size increased while waiting for a transplant assessment. One patient died while on the waiting list for a liver transplant. On reviewing the clinical notes, it is important to note that both TACE and RFA were used as a bridge for liver transplant and liver resection in 3 cases. Three patients were offered TACE but declined to have any treatment. Few more cases were offered Sorafenib but declined to have chemotherapy for HCC following discussion with a specialised oncologist.
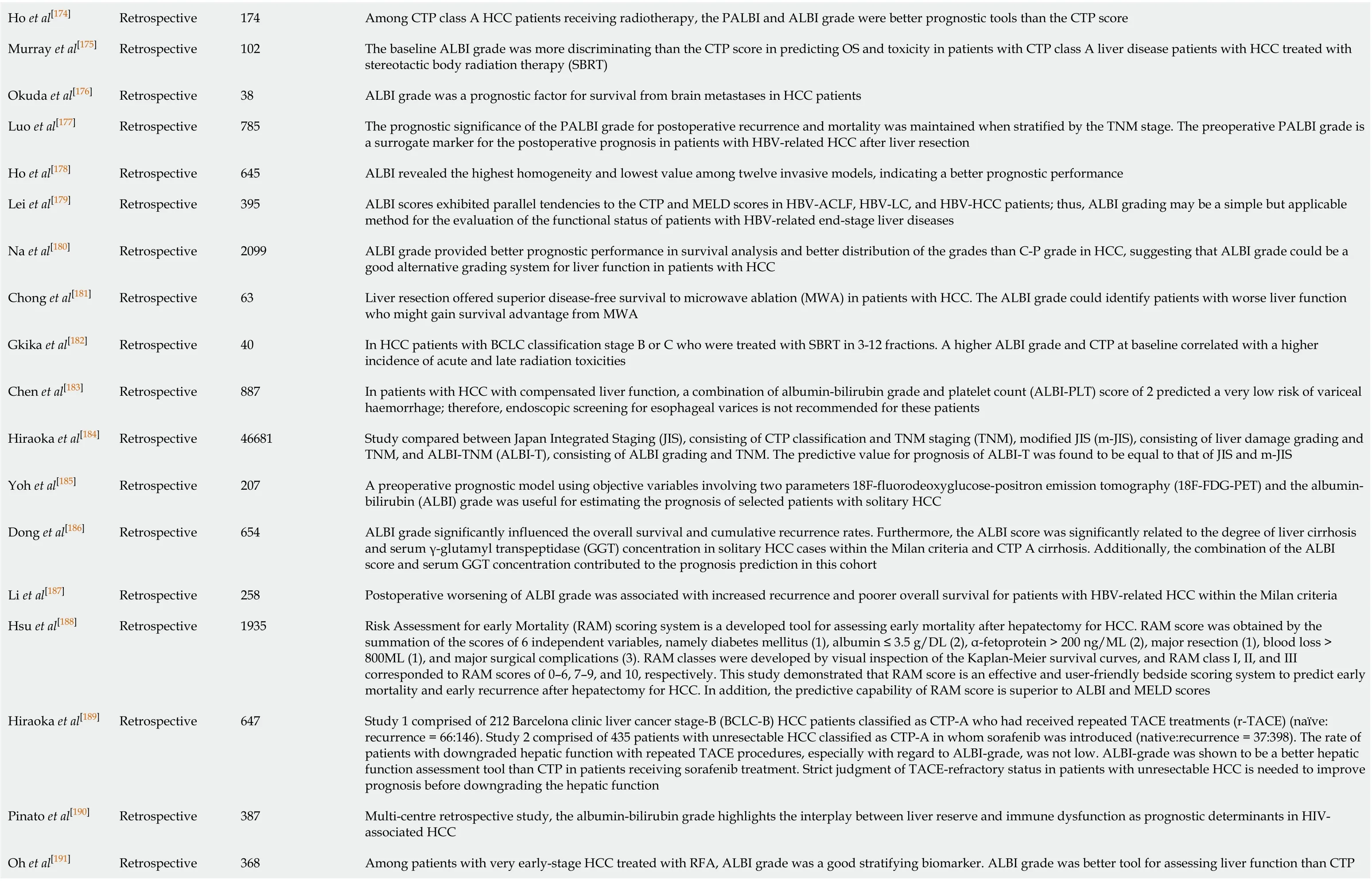
We divided patients into two groups treated and not treated. The treated groupincluded curative and non-curative modalities. The mean and median survival for the treated group was 29.7 mo and 18 mo, respectively. The mean and median survival for the non-treated group was 7.7 mo and 4 mo, respectively. This can be observed in the Kaplan-Meier survival curves for the treated and non-treated groups in (Figure 1A). Mean survival for resection was 47.8 mo, liver transplant was 23.2 mo, RFA was 12.29 months, TACE was 17.3 mo and Sorafenib was 4 mo.

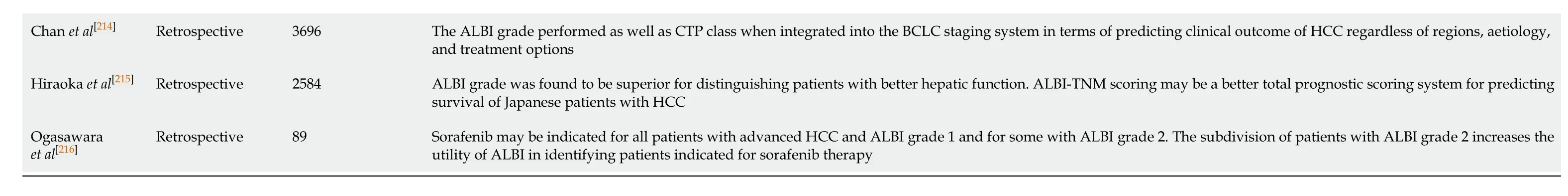
Table 2 Studies describing the relation between hepatocellular carcinoma and albumin bilirubin grade in the last 5 years

Zhang et al[136]Retrospective 544 Combination of ALBI grade and the fibrosis-4 index (FIB-4) predicted HCC patient outcomes after liver resection. A high ALBI-FIB-4 score was associated with a high incidence of postoperative recurrence and mortality Ho et al[137]Retrospective 123 A comparison among ALBI grades at the start of Lenvatinib for treatment for unresectable HCC identified decline in hepatic function in the early stage ( ≤ 4 weeks, especially within 2 weeks)Hiraoka et al[138]Retrospective 3690 A proposed ALBI-based nomogram of BCLC system was found to be a feasible strategy to estimate the survival of individual HCC patient except for very early stage patients Takada et al[139]Retrospective 190 Baseline ALBI was a predictor to direct candidates for second-line treatment after sorafenib in unresectable HCC Ni et al[140]Retrospective 349 Platelet ALBI (PALBI) grade demonstrated significant greater area under the curve values than ALBI grade or CTP class in predicting 1-, 3- and 5-year OS in patients with large HCCs after transarterial chemoembolization combined with microwave ablation (TACE-MWA)Nguyen et al[141]Retrospective 110 Baseline ALBI grade is an independent predictor of survival in patients treated with sorafenib Ho et al[142]Retrospective 1655 ALBI grade is feasible in predicting survival in HCC patients within the Milan criteria, and helps identify high-risk patients who need timely liver transplantation Lee et al[143]Retrospective 570 ALBI is associated with survival in BCLC stage B HCC patients undergoing TACE. ALBI can be applied to select patients who can get most benefit from TACE Hiraoka et al[144]Retrospective 84 Good hepatic function represented by the ALBI grades at introduction of the initial tyrosine kinase inhibitor (TKI) is a requirement for improved prognosis of unresectable HCC undergoing TKI sequential therapy, including Lenvatinib (LEN)Elshaarawy[145]Retrospective 1910 Validation study for the proposed modified albumin-bilirubin-TNM (mALBI-T) grade as a prognostic model for patients with HCC. ALBI-T grade was a superior prognostic tool that selects patients with HCC who have better liver reservoir and tumour stage Ueshima et al[146]Retrospective 82 Patients with CTP score of 5 and ALBI grade 1 predicted a higher response rate and lower treatment discontinuation due to adverse events by Lenvatinib treatment Sonohara et al[147]Retrospective 305 Platelet-albumin-bilirubin (PALBI) grade can be used for assessing perioperative risks for hepatectomy for HCC Antkowiak et al[148]Retrospective 1000 Median OS for ALBI 1, 2, and 3 grades was 46.7, 19.1, and 8.8 months, respectively. Median OS for CTP A, B, and C was 21.7, 11.3, and 6.0 mo, respectively. ALBI outperforms CTP in survival prognosis in yttrium-90 radioembolization (Y90) treated patients. On sub-analyses, serum albumin (not bilirubin) appears to be the main driver of survival prediction Honmyo et al[149]Retrospective 1270 ALBI and Albumin-Indocyanine Green Evaluation (ALICE) grading systems could estimate the liver function of patients with HCC. Regarding hepatectomy patients, the ALICE grade was a more suitable model than the ALBI grade Khalid et al[150]Retrospective 71 Mean ALBI score in the study was -1.59 ± 0.69, with the majority (49. 2 %) falling in grade 2. The mean duration of survival at the last follow up was of 12.1 ± 12.14 mo (1-49). Univariate analysis showed serum albumin (P = 0.003), serum bilirubin (P = 0.018), CTP score (P = 0.019), ALBI grade (P = 0.001) and presence of varices (P = 0.04) to be the main predictors of 6 months survival after TACE. On Cox analysis, only ALBI score (P = 0.038) showed statistically significant association Luo et al[151]Retrospective 132 Combined albumin- bilirubin (ALBI) grade and aspartate aminotransferase-to-platelet count ratio index (APRI) score and presence of microvascular invasion correlated with postoperative mortality. The area under the curve for ALBI-APRI score was significantly higher than either ALBI or APRI alone for predicting both postoperative recurrence and mortality. ALBI-APRI score may be a predictor for the prognosis of patients with HCC within Milan criteria following liver resection Lu et al[152]Retrospective 2038 Study aimed to identify liver function reserve in CTP class A HCC patients. The platelet-albumin-bilirubin (PALBI) was discriminatory for risk stratification of PHLF grade B/C and OS in CTP class A HCC patients following resection Lee et al[153]Retrospective 6669 The median OS durations of PALBI grade1 (38.4%), grade2 (33.2%), and grade3 (28.4%) patients were 81, 30, and 5 mo, respectively (P < 0.001). The PALBI grade had a larger area under the receiver operator characteristic curve (AUC) than did the CTP class, MELD score, and ALBI grade. Moreover, the PALBI and ALBI grades enabled subclassification of CTP A patients (P < 0.001). In a multivariate analysis, the PALBI and ALBI grades were significant risk factors for OS (P < 0.05). According to treatment modality, the PALBI grade was predictive of OS in patients receiving TACE or supportive care. The ALBI grade was predictive of OS in patients undergoing surgical resection or radiofrequency ablation In HCC after stereotactic body radiation therapy CTP class was significantly related to OS, with a median OS of 29.9 mo in CTP-A, 11.5 in CTP-B. ALBI grade was also significantly related to OS, with a median OS of 53.0 mo in ALBI-1, 19.5 mo in ALBI-2, and 6.5 mo in ALBI-3. The ALBI score was a more objective, discriminatory and Su et al[154]Retrospective 594
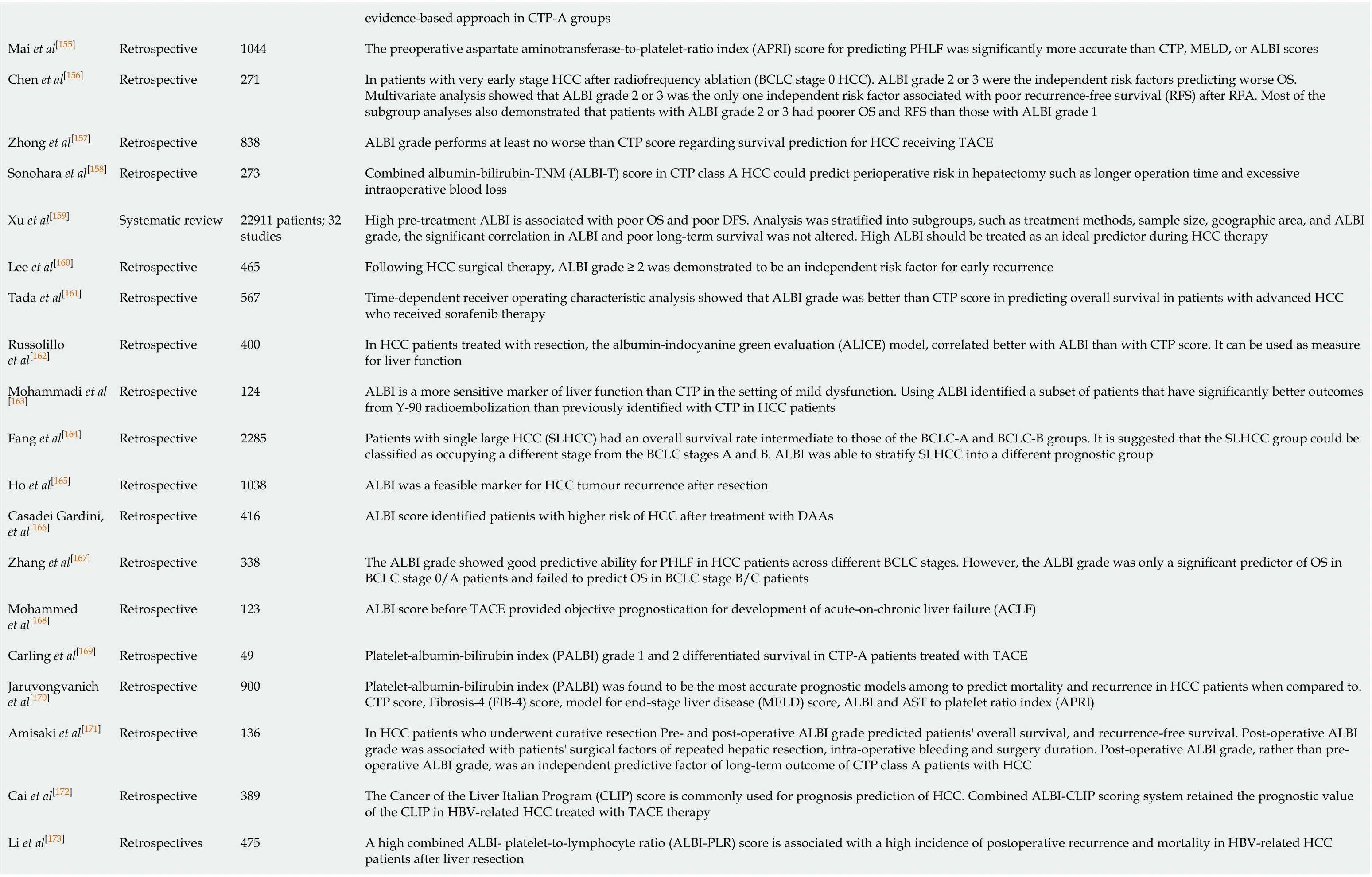
evidence-based approach in CTP-A groups Mai et al[155]Retrospective 1044 The preoperative aspartate aminotransferase-to-platelet-ratio index (APRI) score for predicting PHLF was significantly more accurate than CTP, MELD, or ALBI scores Chen et al[156]Retrospective 271 In patients with very early stage HCC after radiofrequency ablation (BCLC stage 0 HCC). ALBI grade 2 or 3 were the independent risk factors predicting worse OS. Multivariate analysis showed that ALBI grade 2 or 3 was the only one independent risk factor associated with poor recurrence-free survival (RFS) after RFA. Most of the subgroup analyses also demonstrated that patients with ALBI grade 2 or 3 had poorer OS and RFS than those with ALBI grade 1 Zhong et al[157]Retrospective 838 ALBI grade performs at least no worse than CTP score regarding survival prediction for HCC receiving TACE Sonohara et al[158]Retrospective 273 Combined albumin-bilirubin-TNM (ALBI-T) score in CTP class A HCC could predict perioperative risk in hepatectomy such as longer operation time and excessive intraoperative blood loss Xu et al[159]Systematic review 22911 patients; 32 studies High pre-treatment ALBI is associated with poor OS and poor DFS. Analysis was stratified into subgroups, such as treatment methods, sample size, geographic area, and ALBI grade, the significant correlation in ALBI and poor long-term survival was not altered. High ALBI should be treated as an ideal predictor during HCC therapy Lee et al[160]Retrospective 465 Following HCC surgical therapy, ALBI grade ≥ 2 was demonstrated to be an independent risk factor for early recurrence Tada et al[161]Retrospective 567 Time-dependent receiver operating characteristic analysis showed that ALBI grade was better than CTP score in predicting overall survival in patients with advanced HCC who received sorafenib therapy Russolillo et al[162]Retrospective 400 In HCC patients treated with resection, the albumin-indocyanine green evaluation (ALICE) model, correlated better with ALBI than with CTP score. It can be used as measure for liver function Mohammadi et al [163]Retrospective 124 ALBI is a more sensitive marker of liver function than CTP in the setting of mild dysfunction. Using ALBI identified a subset of patients that have significantly better outcomes from Y-90 radioembolization than previously identified with CTP in HCC patients Fang et al[164]Retrospective 2285 Patients with single large HCC (SLHCC) had an overall survival rate intermediate to those of the BCLC-A and BCLC-B groups. It is suggested that the SLHCC group could be classified as occupying a different stage from the BCLC stages A and B. ALBI was able to stratify SLHCC into a different prognostic group Ho et al[165]Retrospective 1038 ALBI was a feasible marker for HCC tumour recurrence after resection Casadei Gardini, et al[166]Retrospective 416 ALBI score identified patients with higher risk of HCC after treatment with DAAs Zhang et al[167]Retrospective 338 The ALBI grade showed good predictive ability for PHLF in HCC patients across different BCLC stages. However, the ALBI grade was only a significant predictor of OS in BCLC stage 0/A patients and failed to predict OS in BCLC stage B/C patients Mohammed et al[168]Retrospective 123 ALBI score before TACE provided objective prognostication for development of acute-on-chronic liver failure (ACLF)Carling et al[169]Retrospective 49 Platelet-albumin-bilirubin index (PALBI) grade 1 and 2 differentiated survival in CTP-A patients treated with TACE Jaruvongvanich et al[170]Retrospective 900 Platelet-albumin-bilirubin index (PALBI) was found to be the most accurate prognostic models among to predict mortality and recurrence in HCC patients when compared to. CTP score, Fibrosis-4 (FIB-4) score, model for end-stage liver disease (MELD) score, ALBI and AST to platelet ratio index (APRI)Amisaki et al[171]Retrospective 136 In HCC patients who underwent curative resection Pre- and post-operative ALBI grade predicted patients' overall survival, and recurrence-free survival. Post-operative ALBI grade was associated with patients' surgical factors of repeated hepatic resection, intra-operative bleeding and surgery duration. Post-operative ALBI grade, rather than preoperative ALBI grade, was an independent predictive factor of long-term outcome of CTP class A patients with HCC Cai et al[172]Retrospective 389 The Cancer of the Liver Italian Program (CLIP) score is commonly used for prognosis prediction of HCC. Combined ALBI-CLIP scoring system retained the prognostic value of the CLIP in HBV-related HCC treated with TACE therapy Li et al[173]Retrospectives 475 A high combined ALBI- platelet-to-lymphocyte ratio (ALBI-PLR) score is associated with a high incidence of postoperative recurrence and mortality in HBV-related HCC patients after liver resection
Ho et al[174]Retrospective 174 Among CTP class A HCC patients receiving radiotherapy, the PALBI and ALBI grade were better prognostic tools than the CTP score Murray et al[175]Retrospective 102 The baseline ALBI grade was more discriminating than the CTP score in predicting OS and toxicity in patients with CTP class A liver disease patients with HCC treated with stereotactic body radiation therapy (SBRT)Okuda et al[176]Retrospective 38 ALBI grade was a prognostic factor for survival from brain metastases in HCC patients Luo et al[177]Retrospective 785 The prognostic significance of the PALBI grade for postoperative recurrence and mortality was maintained when stratified by the TNM stage. The preoperative PALBI grade is a surrogate marker for the postoperative prognosis in patients with HBV-related HCC after liver resection Ho et al[178]Retrospective 645 ALBI revealed the highest homogeneity and lowest value among twelve invasive models, indicating a better prognostic performance Lei et al[179]Retrospective 395 ALBI scores exhibited parallel tendencies to the CTP and MELD scores in HBV-ACLF, HBV-LC, and HBV-HCC patients; thus, ALBI grading may be a simple but applicable method for the evaluation of the functional status of patients with HBV-related end-stage liver diseases Na et al[180]Retrospective 2099 ALBI grade provided better prognostic performance in survival analysis and better distribution of the grades than C-P grade in HCC, suggesting that ALBI grade could be a good alternative grading system for liver function in patients with HCC Chong et al[181]Retrospective 63 Liver resection offered superior disease-free survival to microwave ablation (MWA) in patients with HCC. The ALBI grade could identify patients with worse liver function who might gain survival advantage from MWA Gkika et al[182]Retrospective 40 In HCC patients with BCLC classification stage B or C who were treated with SBRT in 3-12 fractions. A higher ALBI grade and CTP at baseline correlated with a higher incidence of acute and late radiation toxicities Chen et al[183]Retrospective 887 In patients with HCC with compensated liver function, a combination of albumin-bilirubin grade and platelet count (ALBI-PLT) score of 2 predicted a very low risk of variceal haemorrhage; therefore, endoscopic screening for esophageal varices is not recommended for these patients Hiraoka et al[184]Retrospective 46681 Study compared between Japan Integrated Staging (JIS), consisting of CTP classification and TNM staging (TNM), modified JIS (m-JIS), consisting of liver damage grading and TNM, and ALBI-TNM (ALBI-T), consisting of ALBI grading and TNM. The predictive value for prognosis of ALBI-T was found to be equal to that of JIS and m-JIS Yoh et al[185]Retrospective 207 A preoperative prognostic model using objective variables involving two parameters 18F-fluorodeoxyglucose-positron emission tomography (18F-FDG-PET) and the albuminbilirubin (ALBI) grade was useful for estimating the prognosis of selected patients with solitary HCC Dong et al[186]Retrospective 654 ALBI grade significantly influenced the overall survival and cumulative recurrence rates. Furthermore, the ALBI score was significantly related to the degree of liver cirrhosis and serum γ-glutamyl transpeptidase (GGT) concentration in solitary HCC cases within the Milan criteria and CTP A cirrhosis. Additionally, the combination of the ALBI score and serum GGT concentration contributed to the prognosis prediction in this cohort Li et al[187]Retrospective 258 Postoperative worsening of ALBI grade was associated with increased recurrence and poorer overall survival for patients with HBV-related HCC within the Milan criteria Hsu et al[188]Retrospective 1935 Risk Assessment for early Mortality (RAM) scoring system is a developed tool for assessing early mortality after hepatectomy for HCC. RAM score was obtained by the summation of the scores of 6 independent variables, namely diabetes mellitus (1), albumin ≤ 3.5 g/DL (2), α-fetoprotein > 200 ng/ML (2), major resection (1), blood loss > 800ML (1), and major surgical complications (3). RAM classes were developed by visual inspection of the Kaplan-Meier survival curves, and RAM class I, II, and III corresponded to RAM scores of 0–6, 7–9, and 10, respectively. This study demonstrated that RAM score is an effective and user-friendly bedside scoring system to predict early mortality and early recurrence after hepatectomy for HCC. In addition, the predictive capability of RAM score is superior to ALBI and MELD scores Hiraoka et al[189]Retrospective 647 Study 1 comprised of 212 Barcelona clinic liver cancer stage-B (BCLC-B) HCC patients classified as CTP-A who had received repeated TACE treatments (r-TACE) (naïve: recurrence = 66:146). Study 2 comprised of 435 patients with unresectable HCC classified as CTP-A in whom sorafenib was introduced (native:recurrence = 37:398). The rate of patients with downgraded hepatic function with repeated TACE procedures, especially with regard to ALBI-grade, was not low. ALBI-grade was shown to be a better hepatic function assessment tool than CTP in patients receiving sorafenib treatment. Strict judgment of TACE-refractory status in patients with unresectable HCC is needed to improve prognosis before downgrading the hepatic function Pinato et al[190]Retrospective 387 Multi-centre retrospective study, the albumin-bilirubin grade highlights the interplay between liver reserve and immune dysfunction as prognostic determinants in HIVassociated HCC Among patients with very early-stage HCC treated with RFA, ALBI grade was a good stratifying biomarker. ALBI grade was better tool for assessing liver function than CTP Oh et al[191]Retrospective 368
score for very early-stage HCC treated with RFA Lo et al[192]Retrospective 152 ALBI was a predictor for both survival and liver toxicity. Complementary use of CTP and ALBI score could predict the risk of post stereotactic ablative radiation therapy (SABR) liver toxicity. Further prospective studies are necessary before use of the ALBI score can become part of daily practice Chong et al[193]Retrospective 488 Liver resection offered superior survival to RFA in patients with BCLC stage 0/A HCC. The ALBI grade could identify those patients with worse liver function who did not gain any survival advantage from curative liver resection Lee et al[194]Retrospective 404 ALBI can stratify the patients with advanced HCC for the second-line trials or salvage therapy Hansman et al[195]Retrospective 180 ALBI grades are accurate survival metrics in high-risk patients undergoing conventional TACE for HCC Zou et al[196]Retrospective 229 The ALBI score showed superior predictive value of post-operative outcomes over CTP score Ho et al[197]Retrospective 881 ALBI grade served as an objective and feasible surrogate to predict the prognosis of HCC patients undergoing TACE Hiraoka et al[198]Retrospective 3495 ALBI grade is a useful and easy classification system for assessment of hepatic function for therapeutic decision making Kao et al[199]Retrospective 622 ALBI grade offered personalized long-term survival data for patients with early-stage HCC who undergo RFA Gui et al[200]Retrospective 117 ALBI grade demonstrated clear survival discrimination that is superior to CTP class among HCC patients treated with radio-embolization,particularly within the subgroup of CTP class A patients Kuo et al[201]Retrospective 260 ALBI grade at baseline and also ALBI grade change during treatment predicted the prognosis of advanced HCC patients who received sorafenib Waked et al[202]Retrospective 3030 The ALBI grade categorised patients receiving TACE into three clear prognostic groups, thereby emphasising the importance of underlying liver function in the outcome of TACE Pinato et al[203]Retrospective 447 The ALBI grade at sorafenib discontinuation identified a subset of patients with prolonged stability of hepatic reserve and superior survival. This may allow improved patient selection for second-line therapies in advanced HCC King et al[204]Retrospective 448 Patients with ALBI grade > 1, CTP class B or poor performance status seem to derive limited benefit from sorafenib treatment Li et al[205]Retrospective 491 The ALBI grade added superior prognostic value compared to CTP class in patients with HCC who underwent liver resection Ma et al[206]Retrospective 318 ALBI grade predicted OS in patients with early-HCC. Reclassification of CTP class according to ALBI grade might improve the management of HCC Liu et al[207]Retrospective 3182 ALBI grades assess liver dysfunction in HCC. The PALBI grade is consistently better in all patients, in patients with minimally decreased liver function, and in patients receiving different aggressive therapies Pinato et al[208]Retrospective 2426 In this large, multi-centre retrospective study, the ALBI grade satisfied the criteria for accuracy and reproducibility following statistical validation in Eastern and Western HCC patients, including those treated with TACE. Consideration should be given to the ALBI grade as a stratifying biomarker of liver reserve in routine clinical practice Hiraoka et al[209]Retrospective 754 ALBI grade is simple and useful for prediction of prognosis and therapy decision-making in the heterogeneous population of BCLC stage B patients Chan et al[210]Retrospective 1973 The ALBI grade performs as well as the CTP grade when integrating into the CLIP system Edeline et al[211]Retrospective 1019 ALBI should be a stratifying factor in trials of systemic therapy Hickey et al[212]Retrospective 428 ALBI grade outperforms CTP class at discriminating survival in patients receiving TACE or (90) Y radioembolization. ALBI grade is also valuable in patients with moderate liver dysfunction and BCLC stage B disease Wang et al[213]Retrospective 1242 The ALBI grade predicted PHLF and OS in patients with HCC undergoing liver resection with curative intent more accurately than the CTP class
ALBI: Albumin bilirubin grade; HCC: Hepatocellular carcinoma ; CTP: Child turcotte pugh score; HCV: Hepatitis C virus; US-PMWA: Ultrasound-guided percutaneous microwave ablation; TACE-MWA: Transarterial chemoembolization combined with microwave ablation; OS: Overall survival; RFS: Recurrence free survival; CEUS: Contrast-enhanced ultrasound; NLR: Neutrophil lymphocyte ratio; SIRT: Selective internal radiation therapy; PHLF: Post-hepatectomy liver failure; BCLC: Barcelona clinic liver cancer staging system; MELD: Model for end-stage liver disease; RFA: Radiofrequency ablation; DAAs: Direct-acting antivirals; PALBI: Platelet-albumin-bilirubin index; FIB-4: Fibrosis-4 ; APRI: AST to platelet ratio index; CLIP: Cancer of the liver Italian program; DFS: Disease free survival; HBV: Hepatitis B virus; AUC: Area under the curve.
CTP Score was also good in predicting overall survival. The mean and median survival for CTP (A) was 26.3 and 15 mo, CTP (B) 9.6 and 5 mo and CTP (C) 3.2 and 2 mo. This can be also observed in the survival curves (Figure 1B).
Overall survival per tumour number is shown in (Table 3). There was a negative significant relationship between the size of the largest HCC tumour/nodule detected on imaging and survival (P= 0.009). Our study also showed that BCLC is a good staging system when it comes to survival. The median survival for BCLC 0 was 50 mo, BCLC A was 40 mo, BCLC B was 21 mo, BCLC C was 6 mo and for BCLC D was 2 mo. Median survival with AFP < 10 KU/L was 20 mo and with AFP > 10 KU/L was 5 mo. We found that AFP was inversely related to survival, the higher the AFP the smaller number of months they live after HCC diagnosis. However, this relationship was not statically significant (P= 0.132).
NLR had a significant (P= 0.011) negative relationship, the higher the NLR the smaller number of months patients live after HCC diagnosis. NLR was categorised to < 3 and > 3 as previously described literature (Figure 1C). The mean and median survival with NLR < 3 was 24.5 and 11 mo respectively and with NLR > 3 the mean was 12.1 mo and the median survival was 6 mo.
We also calculated the ALBI grades at diagnosis and compared them to overall survival. The mean and median survival for ALBI grade 1 were 37.7 and 26 mo, ALBI grade 2 were 13.4 and 6 mo and for ALBI grade 3 were 4.5 and 3 months (Figure 1D).
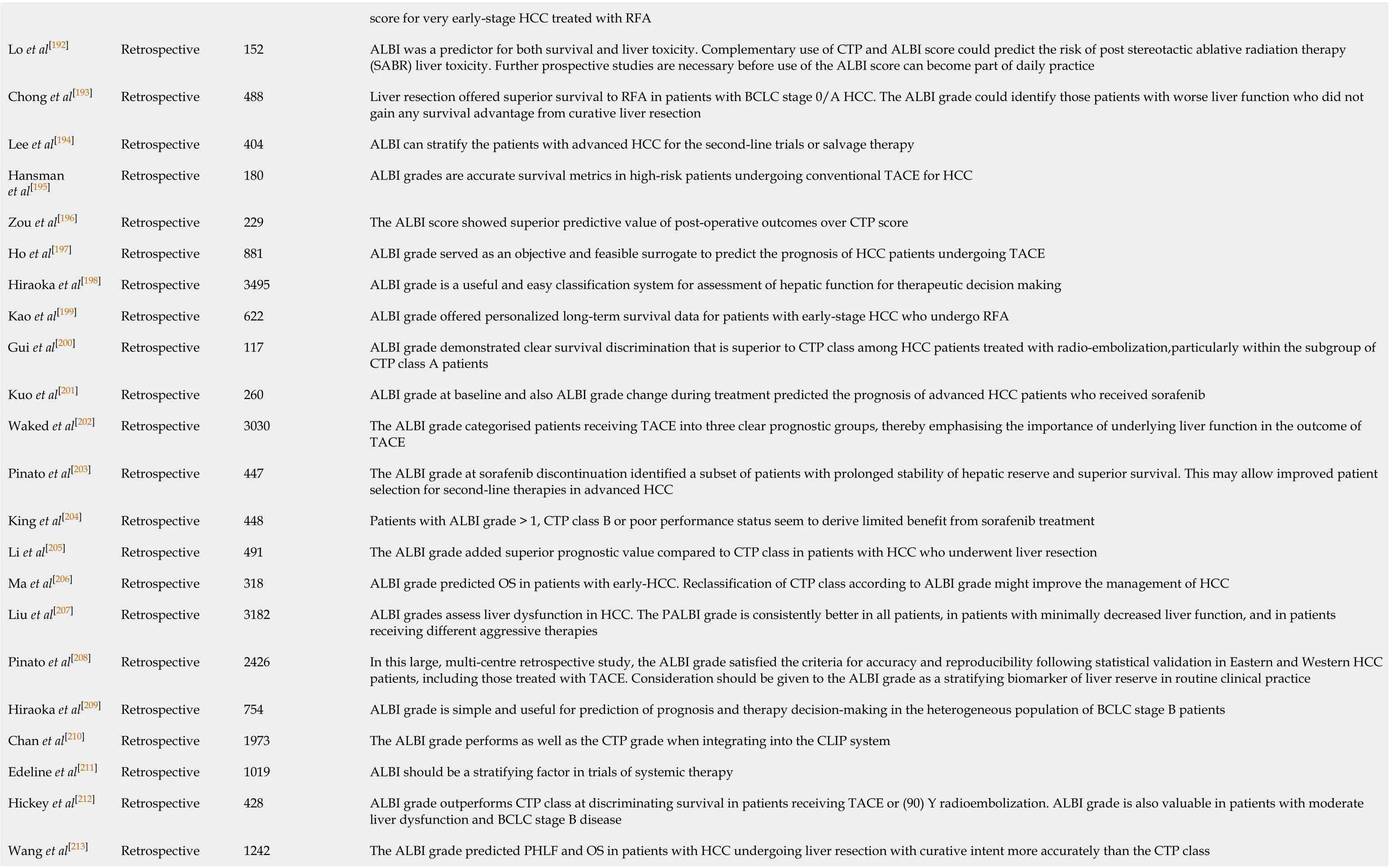
Visually the Kaplan Meier curves showed better discriminative performance for ALBI grade than CTP score. To further evaluate this, we performed a comparison between receiver operating characteristics curves of CTP and ALBI. The area under the curve showed that ALBI was better than CTP in detecting death from HCC (Figure 2).

Table 3 Characteristics of hepatocellular carcinoma in University Hospital, Coventry, United Kingdom between December 2013 and December 2018
DISCUSSION
Our systematic search identified many studies describing NLR and ALBI in HCC over the last 5 years. Indeed, they are simple to use and they are also done routinely in HCC patients. It is important to note that NLR was proposed to be a surrogate marker of inflammation and immunological status in many diseases not just solely in HCC, it was also reported to add prognostic value in various other cancers. Only a few studies in this review found NLR not an independent indicator for prognosis[71,72], while many studies associated NLR with HCC progression and metastatic spread. In particular, our review identified that NLR was associated with tumour vascular invasion and large tumour size and raised NLR (> 3) was associated with early and overall recurrence and survival after resection in HCC patients. Our local cohort also revealed that patients with high NLR (> 3) had an inversely significant relationship with survival.
In this review, the ALBI results described in (Table 2) showed better discriminative performance than CTP class as an indicator for survival after HCC diagnosis in many studies. ALBI was validated in large cohorts and was shown to be a good prognostic model in HCC. ALBI was shown to be able to stratify the choice of therapeutic interventions in HCC, in addition to the morphological features of HCC.
Our local cohort demonstrated typical characteristics for the HCC patient, being frequently in males and that two thirds of the patients had liver cirrhosis. Commonest presenting symptoms were abdominal pain and weight loss. In addition to this incidental diagnosis and hepatic decompensation were also common. This suggests that there was variability in the clinical presentation. Biochemical liver abnormality was commonly detected with serum Alkaline phosphatase being markedly raised in comparison to Alanine transaminase.
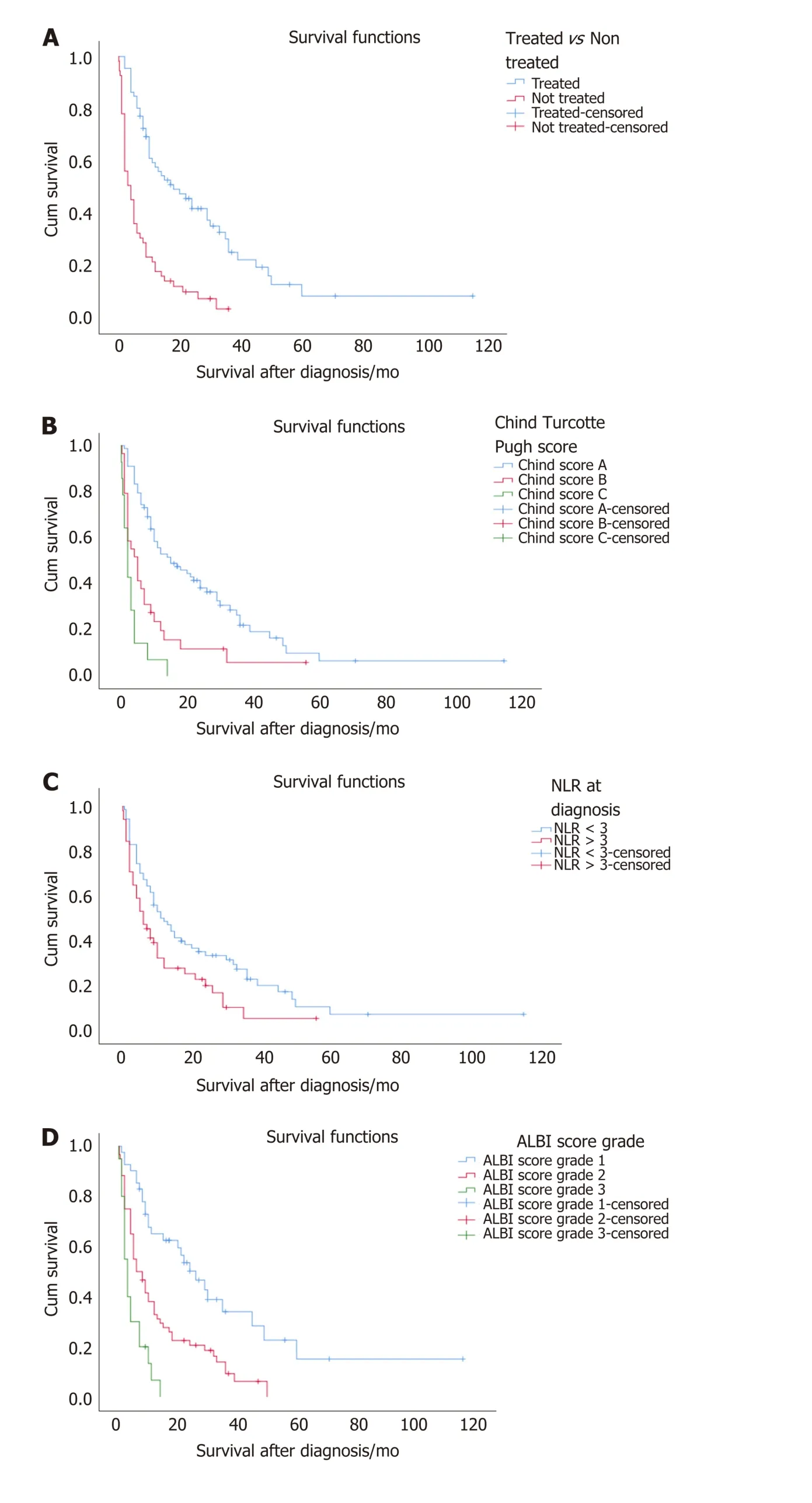
Figure 1 Hepatocellular carcinoma survival curves. A: Survival curve between the treated and non-treated group; B: Survival curve between different stages of the child Turcotte Pugh score; C: Survival curve comparing low and high neutrophil to lymphocyte ratio; D: Survival curve comparing different albumin bilirubin grades. NLR: Neutrophil to lymphocyte ratio. ALBI: Albumin bilirubin.
We would like to highlight that nearly 50% of the patients in our study had normal AFP. This suggests its poor sensitivity and specificity. International guidelines advised on not using AFP routinely in screening patients at risk of developing HCC[1,2]. As in the literature, we found that in secretory HCC the serum AFP increases with the tumour growth and can predict poor survival and hence AFP can be considered a predictor of survival in patients who already had raised AFP at time of the diagnosis.
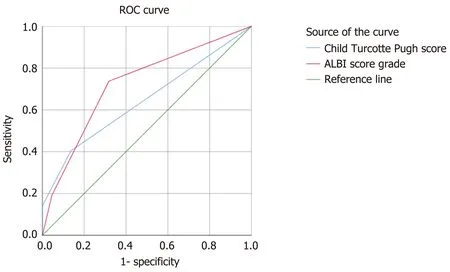
Figure 2 Receiver operating characteristic curves comparing between child turcotte pugh score and albumin bilirubin grading system. The area under the curves represents death from hepatocellular carcinoma. ROC: Receiver operating characteristic.
We found that patients who were treated with surgical resection have survived more than patients who had a liver transplant. However, this is not significant given that only 4 patients underwent liver transplantation in our cohort. RFA and TACE were used in some cases as bridge therapy while awaiting transplantation. Some patients who underwent chemotherapy by Sorafenib often developed side effects and were not able to continue with the chemotherapy.
This review was limited to 5 years only and hence not inclusive of all data around NLR and HCC. Nevertheless, studies concluded in (Table 1) are sufficient to formulate a clinical opinion that NLR is a generic marker of inflammation in HCC and is associated with the overall prognosis. On the other hand, the review included all studies published since the first paper describing ALBI. Another limitation is that nearly all studies were retrospective, however, many had large numbers of HCC patients.
Many HCC patients are diagnosed radiologically in this era. The cancer HPB-MDT involved need to adequately prognosticate and stage patients. NLR and ALBI can aid by eliminating variable judgement between clinicians. Given the evidence from this systematic search, we argue that ALBI can be incorporated in staging HCC rather than CTP and that NLR can be used as an additional marker for severity of HCC in case of normal AFP. This will be required to be looked into by the interested stakeholders in the care of HCC patients.
CONCLUSION
NLR and ALBI are validated easy cost-effective markers that can predict survival and help in stratifying therapeutic interventions. They should be included in modified staging systems for HCC. They can be used for monitoring inflammation status and liver function in HCC patients in addition to overall functional status and radiological features.
ARTICLE HIGHLIGHTS

Research objectives
To study the published literature of NLR and ALBI from a clinical point of view.
Research methods
Systematic search over the last 5 years of published literature on NLR and ALBI, and validation of these markers in a retrospective cohort locally in our centre.
Research results
NLR is a generic measure of inflammation in infection, cancer and the critically ill. Raised NLR predicted HCC prognosis and survival. ALBI was better than CTP score in predicting overall survival and liver function in HCC patients. NLR and ALBI can be used in prediction of HCC recurrence after surgery, ablation and chemo/ radioembolisation.
Research conclusions
NLR and ALBI can be used in staging and prognosis of HCC.
Research perspectives
Stakeholders interested in HCC care should consider the use of NLR and ALBI in staging systems for HCC.
ACKNOWLEDGEMENTS
Authors acknowledge the hepato-pancreaticobiliary (HPB) multidisciplinary team and the Performance and Informatics Team at University Hospital, Coventry, UK.
杂志排行
World Journal of Gastroenterology的其它文章
- Bowel function and quality of life after minimally invasive colectomy with D3 lymphadenectomy for rightsided colon adenocarcinoma
- Treatment repurposing for inflammatory bowel disease using literature-related discovery and innovation
- Effects of denosumab treatment in chronic liver disease patients with osteoporosis
- Radiomics of rectal cancer for predicting distant metastasis and overall survival
- Liver fat accumulation measured by high-speed T2-corrected multi-echo magnetic resonance spectroscopy can predict risk of cholelithiasis
- Exploring the food-gut axis in immunotherapy response of cancer patients
