Optimizing biliary outcomes in living donor liver transplantation:Evolution towards standardization in a high-volume center
2020-09-21TsanShiunLinJeffreySamuelCoChaoLongChenAldwinDOng
Tsan-Shiun Lin, JeffreySamuel Co, Chao-Long Chen , AldwinD.Ong
Liver Transplantation Center, Department of Surgery, Kaohsiung Chang Gung Memorial Hospital, 123 Ta-Pei Road, Niao Sung, Kaohsiung 833, Taiwan, China
Keywords:
ABSTRACT
Introduction
Biliary complications remain to be the most significant cause of morbidity after liver transplantation (LT) especially with the use of partial grafts.While a myriad of factors have been identified to increase the risk of biliary complications, such as hepatic artery thrombosis and acute cellular rejection, techniques in biliary reconstruction have received the most attention [1].However, reflective conclusions could only best be derived from high-volume centers with good overall long-term survival [2 , 3].
This review article focuses on the adaptation and evolution of biliary reconstruction techniques for living donor LT (LDLT) in our center, and includes a summary of our classification system for biliary reconstruction and most recent data concerning the clinical course of patients who developed biliary complications after LDLT.
Conventional biliary reconstruction
The Liver Transplantation Center of Kaohsiung Chang Gung Memorial Hospital (KCGMH) was established in 1993 after relocating from Linkou CGMH, where in 1984, Professor Chao-Long Chen accomplished Asia's first successful LT.Since then, over 1700 LDLT cases have been performed in KCGMH under his leadership, and survival outcomes have been consistently excellent by global standards.The center has continually adapted and innovated with every new challenge to improve patient outcomes.One area in LDLT is biliary reconstruction.
Optimizing the bile duct to reduce postoperative biliary complications after LDLT is a complex process that extends from the initial stage of donor evaluation to immunosuppression and surveillance.Intraoperatively, the KCGMH team has made strides in standardizing the techniques.During donor graft procurement,routine complete-hilar-plate-encircling technique [4 , 5]and intraoperative cholangiography are employed, except for selected left lateral segment grafts [6].During recipient biliary reconstruction,a continuous-suture-interrupted-tie technique is used [7].The program's protocols have been described in detail in multiple publications [4 , 5].Conventional biliary reconstructions were performed by two experienced LT surgeons who alternately took cues in reconstructing the bile duct [4].Our reconstructions initially involved the selective placement of internal stents for duct-to-jejunum (DJ)anastomoses and T-tube for duct-to-duct (DD) anastomoses.These methods were abandoned since October 2001, due to the incidence of post-transplant cholangitis and retained stents [4].
Transition to microsurgical biliary reconstruction
Since March 2006, all biliary reconstructions in our center have been performed by an experienced microsurgeon (LTS) under an operating microscope (Carl Zeiss, Jena, Germany) with a magnification of 5 to 15 ×.Periductal tissue around the bile duct is left untouched and is not dissected.Likewise, dissection of the hepatic artery to distant from the duct is avoided to preserve vascularity.Sharp transection of the bile duct is always done using scissors [6].
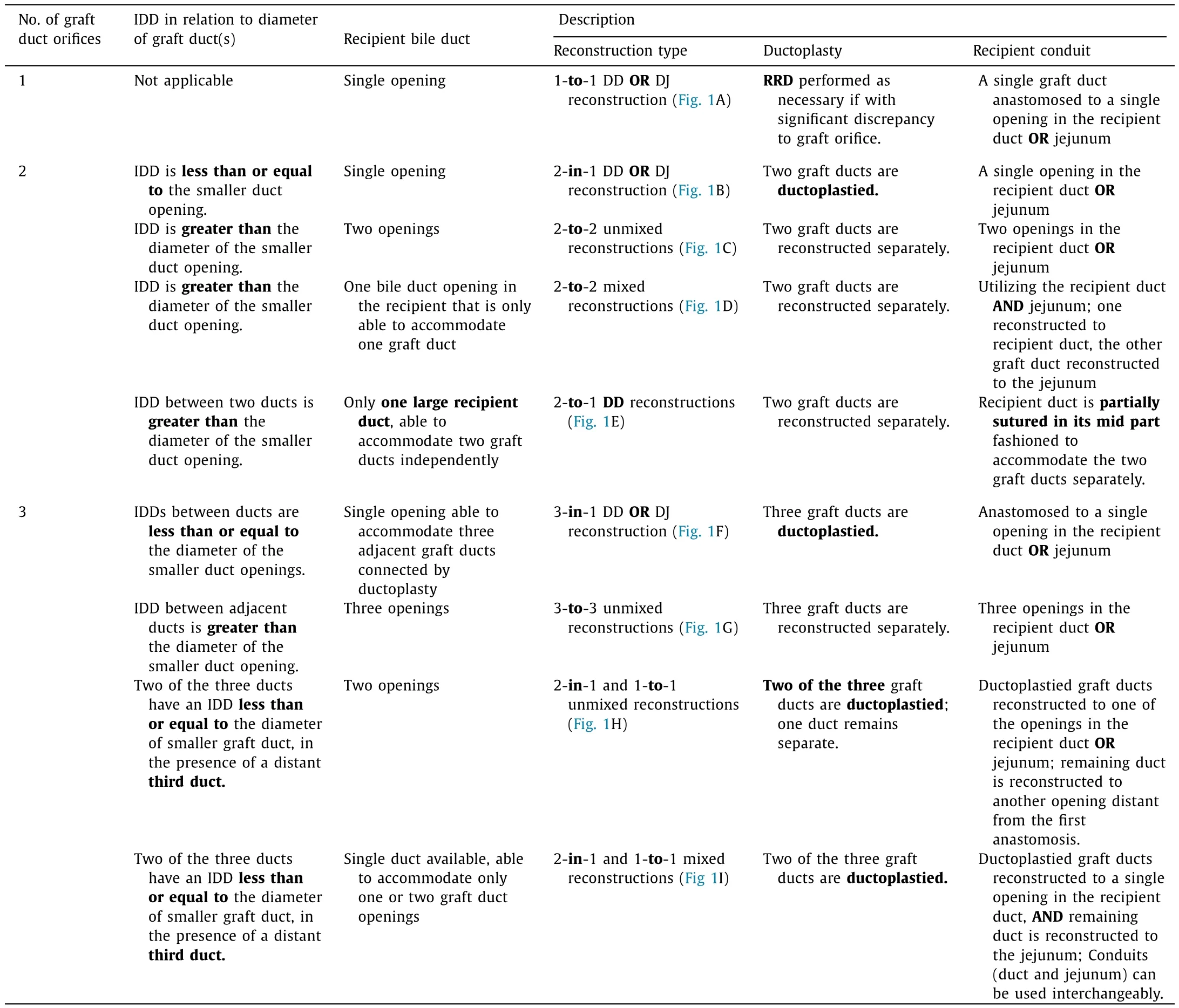
Table 1Classification system for biliary reconstruction in LDLT.
Recipient reduction ductoplasty (RRD), to better approximate the graft to the recipient duct, was done if necessary.RRD was originally performed by an LT surgeon without aid of magnification, while the decision to do graft ductoplasty for multiple graft duct openings was left for the microsurgeon.Microsurgical biliary reconstruction (MBR) was then done using a 6-0 Prolene suture on a 6-0 gage cardiovascular-point needle, employing an interrupted-suturing-technique for the posterior wall, followed by a continuous-suture-interrupted-tie technique for the anterior wall.However, the first 15 RRDs without microscopic aid resulted in a high biliary complication rate(6/15, 40%) [5].
Modifications to the MBR technique
After extensive review and analysis of techniques, adjustments were made so that all subsequent graft and recipient ductoplasties and biliary anastomoses were to be performed exclusively by the microsurgeon under the microscope.These changes significantly reduced biliary complications in a subsequent series down to 6.8% [5].
The primary assessment for poor biliary complication rates was due to the size discrepancy between the recipient and graft ducts.Although RRD was performed, this discrepancy was still obvious under the microscope which remained a challenge for the microsurgeon to fix.
We believe that the majority of the initial anastomotic biliary complications were largely attributable to technical factors.Hence,the following modifications were instituted [5]:
1.RRD is to be performed under an operating microscope when there is size discrepancy between graft and recipient.
2.The posterior wall of the graft and recipient duct is to be secured using interrupted sutures.A continuous-sutureinterrupted-tie technique then is employed for the anterior walls of the graft and recipient ducts, and the remaining length of the recipient duct for RRD.
3.Where multiple duct openings are present in the hepatic graft, donor ductoplasty is to be performed only if the interductal distance (IDD) between the openings is less than or equal to the diameter of the smaller duct opening, otherwise, anastomoses are to be done separately.
4.We created a biliary reconstruction classification system according to the number, size, and IDD of the graft and recipient duct openings.
Biliary reconstruction classification in LDLT
The type of biliary reconstruction depends on (I) the number of duct orifices in the hepatic graft, (II) the IDD in relation to the diameter of the smaller duct opening where two or more graft ducts are present, and (III) the recipient bile duct number and size relative to the graft ducts.On these bases, a classification system has been devised (A) the type of biliary reconstruction, (B) the need for any ductoplasty, and (C) the use of recipient bile duct and/or jejunum as conduit (Table 1) [5].Schematic representations of the various biliary reconstructions are shown in Fig.1.
Our series have shown that MBR capably surmounts the difficulties brought about by the anatomical variations of hepatic ducts in partial liver grafts and the recipients [5].Moreover, with the microsurgery-only graft and recipient ductoplasty modification to our biliary reconstruction technique, biliary complication rates have successfully declined.
Incidence of biliary complications and interventions performed
A total of 156 biliary complications (156/1131, 13.8%) were retrieved from 1131 LDLT recipients from March 2006 to December 2016.All MBRs were performed by LTS (microsurgeon) and biliary complications were managed by the same multidisciplinary team from our center.Patients with biliary complications classi-fied as Clavien-Dindo Grade I and II (n= 41) were excluded from the analysis.These biliary complications included patients who developed transient early biliary leak with spontaneous resolution within 1 week, liver transection surface leak, and imaging-only stenosis.None of our cases developed biliary complication-related life-threatening states (Grade IV) nor led to mortality (Grade V).The analysis included 115 patients (10.2%) who had Grade III biliary complications and required intervention.These patients were followed up for at least two years.
Patients with Grade III biliary complications were managed primarily by endoscopic retrograde biliary drainage (ERBD) with stent placement (n= 80, 69.6%), and percutaneous transhepatic cholangio-drainage (PTCD) (n= 16, 13.9%).Of 12 patients (10.4%)who required surgical intervention, 3 (2.6%) underwent retransplantation.Seven other patients had pigtail insertion for biloma(6.1%).Eighty patients (69.6%) were diagnosed with biliary complications within 1 year after LDLT.The most common biliary complications were strictures (n= 73, 63.5%), followed by leak (n= 32,27.8%), and combined leak and stricture (n= 10, 8.7%).Biliary complications resolved in 80 patients (69.6%) after a median duration of 16.9 (IQR 7-26) months from onset, while 35 patients (30.4%)still had persistence or recurrence of their complications by the end of study.
Summary
Strategies to improve recipient outcomes after LDLT are constantly in evolution and innovations should always be on the way under close scrutiny.Biliary reconstruction is a technically demanding procedure and is associated with known significant complications.Through the years, several investigators have tenaciously probed into creating several technical innovations and have expanded our understanding of the causes concerning these adversities.Currently, biliary reconstruction using microsurgical technique holds much promise in significantly lowering the biliary complication rate after LDLT.With our classification system for biliary reconstruction and standardized protocols, we have been able to maintain an overall intervention-requiring biliary complications rate of 10.2% after long-term follow-up.
Acknowledgments
None.
CRediT authorship contribution statement
Tsan-Shiun Lin:Data curation, Formal analysis, Investigation,Methodology, Visualization.Jeffrey Samuel Co:Writing - original draft.Chao-Long Chen:Conceptualization, Investigation, Supervision, Writing - review & editing.Aldwin D.Ong:Visualization, Formal analysis, Writing - review & editing.
Funding
None.
Ethical approval
Not needed.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Small-for-size syndrome in liver transplantation: Definition,pathophysiology and management
- Endoscopic papillary large balloon dilation with or without sphincterotomy for large bile duct stones removal: Short-term and long-tem outcomes
- Recent evolution of living donor liver transplantation at Kyoto University: How to achieve a one-year overall survival rate of 99%?
- Hepatic vein in living donor liver transplantation
- Hepatobiliary&Pancreatic Diseases International
- Hepatic artery reconstruction in pediatric liver transplantation:Experience from a single group