Recent evolution of living donor liver transplantation at Kyoto University: How to achieve a one-year overall survival rate of 99%?
2020-09-21ToshimiKaido
Toshimi Kaido
a Department of Gastroenterological and General Surgery, St. Luke's International University Hospital, 9-1 Akashi-cho, Chuo-ku, Tokyo 104-8560, Japan
b Division of Hepato-Biliary-Pancreatic and Transplant Surgery, Department of Surgery, Graduate School of Medicine, Kyoto University, Kyoto, Japan
Keywords:
ABSTRACT
Introduction
The first successful living donor liver transplantation (LDLT) was performed in 1989 in Australia by Russell Strong as an alternative to deceased donor liver transplantation (DDLT) for a pediatric patient with biliary atresia [1].Owing to a shortage of deceased donors, LDLT has flourished in various parts of the world, particularly in East Asia [2].Since the first LDLT in June 1990 up to April 2020, nearly 20 0 0 liver transplantations (LTs) have been performed at Kyoto University; only 80 (4%) have been DDLT.Similar to other Japanese institutions, the vast majority of LT (96%) are thus LDLTs.
Previously, LDLT was considered as a “high-risk, high-return”medical treatment due to the high short-term mortality followed by favorable long-term survival.Improving short-term outcomes would thus seem likely to greatly improve long-term outcomes.It was our task to change “high-risk, high-return”to “low-risk, highreturn”situation.The question was how to reach such difficult goal.
Peter Drucker (1909-2005), often considered the father of management, said that, “business has only two functions: marketing and innovation.The aim of marketing is to know and understand the customer so well that the product or service fits him and sells itself.”This idea definitely seems applicable to medical treatments,including LT.One thus needs to know and understand donors and recipients (our customers) extremely well.Once such an understanding achieved, many evidence-based innovations are needed to realize the aim.Using this concept, various innovations were made to the field of LDLT in order to improve the short-term outcomes after LDLT since I joined the Kyoto-LT team in April 2007.In this review article, the recent evolutions made in Kyoto in the field of both of LDLT taking thereby into account the donor as well as the recipient side in order to improve the short-term outcomes are presented.
Left graft-first policy and portal vein pressure modulation
In LDLT, donor safety is clearly of utmost importance.The complication rates among living donors after donor surgery were analyzed according to the graft type.For overall complications, right lobe graft donors had a significantly higher complication rate than left lobe graft donors (44.2% vs.18.8%;P<0.001) [3].Biliary complications were also significantly higher (12.2% vs.4.9%;P<0.001).When considering donor safety, left lobe procurement is thus preferable to right lobe procurement, due to much lower complication rate and larger remnant liver.However, two major obstacles arise when adopting a left graft-first policy: the lower limit of the graft-to-recipient weight ratio (GRWR) and the risk of small-forsize syndrome (SFSS).
As for the lower limit of the GRWR, lower limits were gradually and carefully decreased, changing from 0.8% to 0.7% in December 2007.Since April 2009, the lower limit of GRWR is now0.6%.To prevent SFSS, we started portal vein pressure (PVP) control based on the preliminary findings that patients with PVP ≥15 mmHg after reflow showed a significantly lower overall survival(OS) rate than those with PVP<15 mmHg [4].Fig.1 shows the original Kyoto PVP modulation algorithm.In patients with high PVP (>15 mmHg) after reflow, a splenectomy was performed to reduce PVP.On the other hand, for patients with low PVP after reflow (≤15 mmHg), porto-systemic shunt (e.g.splenorenal shunt)was test clamped and ligated if PVP remained low.In contrast, if PVP was increased to>15 mmHg, a splenectomy was performed followed by a renewed test-clamping of the shunt.If PVP remained high, we did not ligate the shunt and kept it open.If PVP became low (≤15 mmHg), the shunts were ligated.Using this algorithm,it was shown that the lower limit of GRWR could be safely lowered to 0.6% [ 5 , 6 ].The Clavien-Dindo ≥III donor complication rate has gradually decreased to nearly zero since introducing the combination of left graft-first policy and PVP control (Fig.2).Based on these findings it can be concluded that donor safety can be achieved.
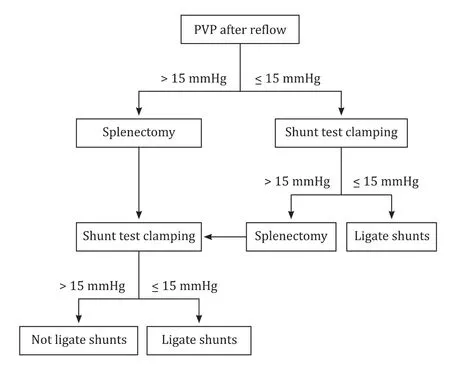
Fig.1.Former portal vein pressure (PVP) modulation algorithm.
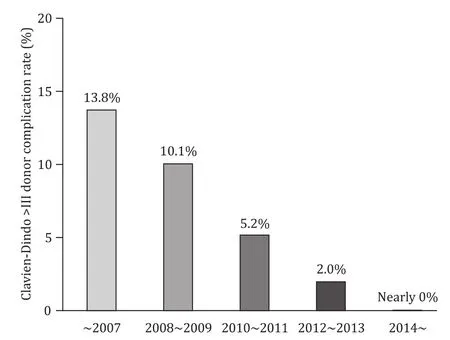
Fig.2.Clavien-Dindo > III donor complication rate.
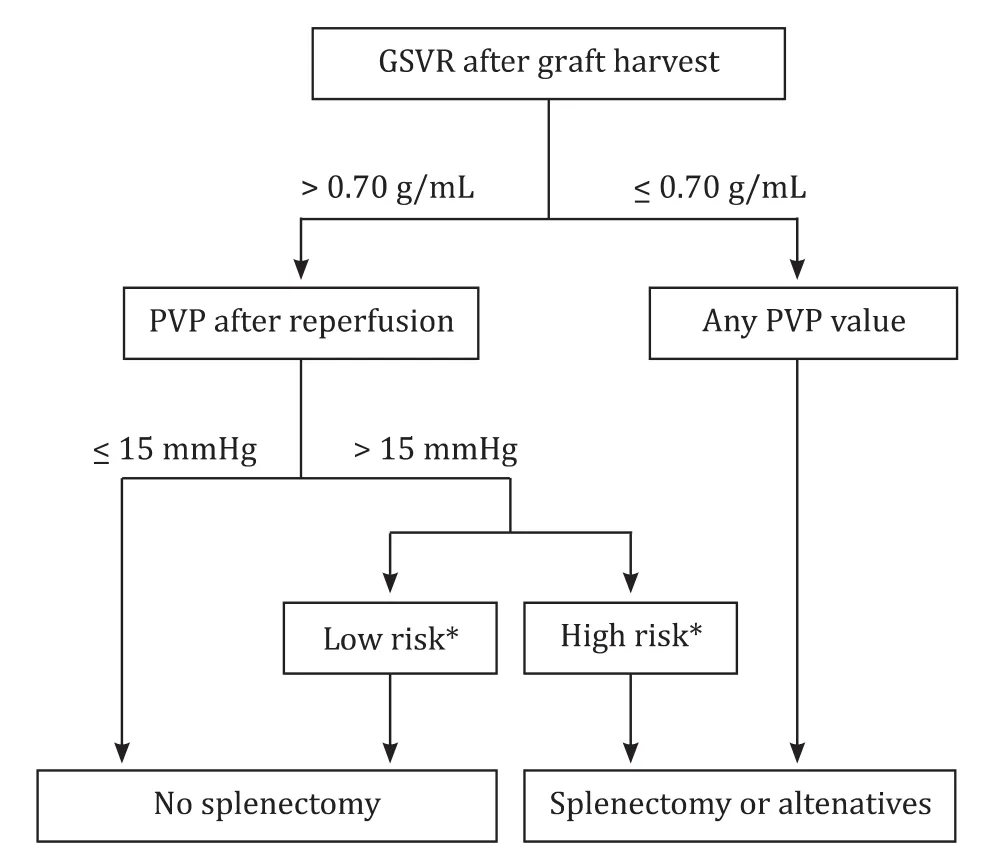
Fig.3.Current portal vein pressure (PVP) modulation algorithm.*: High risk means ABO-incompatible liver transplantation or donor age > 45 years old.Low risk means ABO-compatible liver transplantation and donor age ≤45 years old.
Indeed, the described PVP modulation was useful to improve short-term outcomes.However, since we also reported that older donor age and ABO-incompatibility are independent risk factors for poor patient survival in LDLT, the PVP modulation procedure was reevaluated looking thereby if this technical adaptation was necessary in all LDLT procedure or if there was a place for its selective use [ 7 -10 ].Consequently, we clarified that PVP modulation was key to preventing SFSS and subsequent early graft loss with grafts from either ABO-incompatible or older donors [11].Interestingly, the average donor age in our institution is, for an unclear reason, around 45 years old, an age which is markedly higher than in many other Japan (mid- to late-30s) and Korea (mid- to late-20s) centers.Based on these new findings, the PVP algorithm was adapted.In brief, PVP is not anymore modulated in recipients receiving ABO-compatible and younger donor(≤45 years old) grafts even if the PVP is high (>15 mmHg) after reflow.
In cirrhotic recipients who need LT, the spleen volume not only reflects the portal hemodynamic status but is also associated with excessive portal venous flow and PVP after reperfusion during LT.Gyoten et al.reported that preoperative assessment of graft-tospleen volume ratio (GSVR) is a useful aid to point at the need for splenectomy before reperfusion preventing thereby portal hypertension [12].Despite these findings, the clinical impact of GSVR on post-transplant outcomes remained unclear.Most recently, we investigated the impact of GSVR on outcome after LDLT.Low GSVR(≤0.70 g/mL) was associated with an increased incidence of early graft loss and poor graft survival when the spleen was preserved,but did not affect outcome when splenectomy was performed [13].Based on these new findings, the PVP algorithm was again refined by dividing patients into two subgroups according to their GSVR(Fig.3).Splenectomy or surgical alternatives including splenic artery ligation or embolization and splenic devascularization were performed in patients presenting low GSVR (≤0.70 g/mL) regardless of PVP.Within cases of high GSVR (>0.70 g/mL), PVP modulation was performed for high-risk patients (ABO-incompatible cases or donors>45 years old) as mentioned above.This updated PVP algorithm is now in the process of validation.
Laparoscopy-assisted living donor hepatectomy (hybrid donor operation)
Formerly, living donor hepatectomy was performed as an open abdominal procedure using an inverted T-shape or inverted L-shape incision.However, the donor not being a patient, but rathera healthy individual, smaller wound and reduced invasiveness are more than desirable.Cherqui et al.first reported laparoscopic living donor hepatectomy in 2002 [14].Since then, many papers, mainly from Korea, underlined the utility of laparoscopic living donor hepatectomy [ 15 -17 ].More recently, robotic living donor hepatectomy has been successfully introduced in clinical practice [ 18 , 19 ].
Unfortunately (as of June 2020), the Japanese National Insurance System does not yet cover laparoscopic living donor hepatectomy.Laparoscopy-assisted living donor hepatectomy (hybrid donor operation) was therefore introduced in June 2012, with the intention to reduce the invasiveness to the donor; this technique allows to reduce the abdominal midline incision to 12 to 14 cm.So far more than 200 hybrid donor operations (for all left and right lobe graft cases and for most posterior graft procedures) have been performed.Lateral segment grafts are procured using an open approach with a 10- to 12-cm upper midline incision.Such hybrid donor operations can be as safely performed as open donor hepatectomy and can, furthermore, improve the quality of life without impairing donor or recipient outcomes [20].This hybrid donor operations are at the moment a temporary measure before going to full laparoscopic and robotic donor hepatectomies once the national insurance system allows to cover such type of donor operations.
Expanded criteria of LDLT for hepatocellular carcinoma (HCC)
We would like to briefly mention our expanded criteria of LDLT for recipients with HCC, although this issue is more closely related to mid- to long-term outcomes than short-term outcomes.Needless to say, LT is an ideal treatment for HCC because it not only resects HCCs in the liver but also replaces underlying impaired liver with normal liver.In other words, LT is a radical treatment for HCC because it can simultaneously treat not only intrahepatic metastasis but also multicentric carcinogenesis.Different from Western countries, the high incidence of HCC due to the high epidemic rate of hepatitis B or C virus and the critical shortage of deceased donor organs have led to the rapid development of LDLT in Eastern countries including Japan, Korea, and China.Especially in Japan, there is actually no chance for patients with HCC to undergo DDLT due to the extreme shortage of deceased donor livers.Therefore, the category of LT and the concept of selection criteria of LT for HCC are different between the Western and Eastern countries.
In contrast to DDLT, the indications of LDLT for HCC are decided based on the balance between risks to the live donor and benefits to the recipient.As a result, many Asian transplantation centers also have adopted expanded criteria beyond standard criteria such as the Milan criteria [21]and the University of California San Francisco criteria [22].In general, however, the more the morphological limits of the selection criteria expand, the more the recurrence rates after LT increase.On the basis of the idea that incorporating tumor biological markers and predicting microvascular invasion and poor differentiation could exclude patients with high risk of recurrence before LT, we established new expanded selection criteria, the Kyoto criteria, combining 3 independent significant risk factors for recurrence: tumor number and tumor size based on the findings of pretransplant imaging and tumor markers; tumor number ≤ 10, maximal diameter of each tumor ≤ 5 cm; and serum des-gamma-carboxy prothrombin (DCP) levels ≤400 mAU/mL in 2007 (Fig.4) [23].DCP, also known as protein induced by vitamin K absence or antagonist II, is a well-known tumor marker of HCC whose expression is significantly related to poor prognosis.In a retrospective analysis, 78 patients who met the Kyoto criteria showed significantly lower 5-year recurrence rate than the 40 patients who exceeded the criteria (5% vs.61%,P<0.001) [24].Similarly, 5-year OS rate in patients within the Kyoto criteria was significantly higher compared with patients exceeding the Kyoto criteria (87% vs.34%,P<0.001).Kaido et al.prospectively validated the usefulness of the Kyoto criteria [25].Intention-to-treat analysis of 62 patients who underwent LDLT after implementation of the Kyoto criteria showed that the 5-year OS rate and the recurrence rate were 82% and 7%, respectively.In terms of tumor biology, the incidence of microvascular invasion was significantly lower in patients within the Kyoto criteria than in patients exceeding the Kyoto criteria (P<0.001).Furthermore, the incidence of poorly differentiated HCC was significantly lower in patients within the Kyoto criteria than in patients exceeding the Kyoto criteria (P= 0.010).Moreover, we reported the usefulness of the Kyoto criteria even in LDLT for patients with small HCC and intermediate-stage HCC[ 26 , 27 ].These findings indicate that incorporating tumor markers into selection criteria can successfully widen the indication without increasing the recurrence rate in LDLT for patients with various categories of HCC.
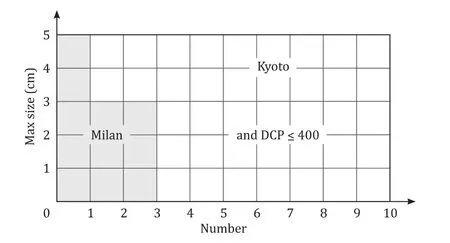
Fig.4.Milan criteria and Kyoto criteria.DCP: des-gamma-carboxy prothrombin.
Infection control as the key to improve short-term survival
When joining the LT program at Kyoto University in 2007, I noticed a special characteristic of the survival curve after LT: a sharp decrease early after LT, followed by gradual decrease during the mid- to long-term follow-up.This characteristic is quite different from survival curves obtained after other surgeries such as gastrectomy for gastric cancer and hepatectomy for HCC.This is a form of marketing as described by Drucker.Indeed long-term survival would definitely improve if the short-term survival curve could be raised substantially.So, first causes of death in the early period after LDLT were examined.Infection was identified as the most frequent (63%) cause of post-LT death [10].Indeed, patients with bacteremia after LDLT showed significantly worse OS than those without [28].Controlling posttransplant infection would thus logically lead to an improved short-term survival after LDLT.
Diagnosing and treating infection in a timely manner and discriminating infection from rejection is not always easy in clinical practice, since both complications are usually accompanied by increases in white blood cells and C-reactive protein.Moreover,treatments for infection and rejection are completely opposed.Inappropriate reinforcement of immunosuppression will further boost already present infections, whereas inadequate immunosuppression will lead to rejection.New biological markers are thus needed to effectively differentiate infection from rejection.Procalcitonin (PCT), a biomarker of severe bacterial infection, was examined as a biomarker for bacteremia.Measurement of PCT was indeed found to effectively distinguish bacteremia from rejection after LDLT; PCT cutofflevels of 0.5 ng/mL and 2.0 ng/mL could be useful to diagnose bacteremia or its absence [29].Furthermore,bundled strategies against infection, including PCT measurement and hand hygiene with contact precautions after LDLT, were established and validated [30].
Simultaneously, risk factors for post-transplant infection were investigated.Surprisingly, none of the well-known risk factors(e.g.Child-Pugh-Turcotte C, high model for end-stage liver disease score, and massive bleeding) but pre-transplant malnutrition was identified as an independent risk factor for in-hospital mortality [31].Based on this finding, the impact of pre-transplant nutrition and body composition on outcomes after LDLT was investigated in depth [ 32 -39 ].Notably, we first reported that pretransplant low skeletal muscle mass (SMM) is an independent risk factor after LDLT [32].
Sarcopenia and body composition
Sarcopenia is a concept first proposed by Rosenberg in 1989 and was named in combination with “sarx”and “penia”, which mean muscle and decrease in Greek, respectively [40].Sarcopenia is now characterized by a progressive decline in SMM and muscle strength or physical activity.However, the impact on surgical outcome, including LT, has been unclear.The impact of pretransplant sarcopenia on outcomes after LT was prospectively analyzed.It was first shown that patients with pretransplant sarcopenia had a significantly worse survival than those without sarcopenia in LDLT(P<0.05) [35].Interestingly, SMM worsened after LDLT and did not recover to preoperative levels until one year after LDLT, while hand grip strength, after an initial sharp decrease at one month,recovered to preoperative levels by 6 months after LDLT.These findings indicated the necessity for mid- to long-term nutritional and rehabilitation interventions after LDLT to achieve full recovery of SMM.Taking into consideration the negative impact of low pretransplant SMM, “inability to walk unaided”was added as a simple criterion for LT from January 2013 onwards to exclude patients with severe sarcopenia for LDLT [30].After the implementation of this criterion, the 1-year OS rate after LDLT improved significantly to 94% [35].A certain insatisfaction about this new criterion remained as the evaluation of this criterion was somewhat subjective; e.g.how long and at what speed should the recipient be able to walk?
In order to establish objective criteria, focus was directed towards other body composition parameters, in addition to SMM,such as muscle steatosis and visceral adiposity.Body compositions can be evaluated by cross-sectional imaging modalities such as CT at the L3 level, bioimpedance analysis (BIA) and dual X-ray absorptiometry (DXA).Among these, CT is the most useful for LT recipients, as indeed these patients already need to undergo abdominal CT to evaluate other issues such as the presence of liver cancer or presence of portosystemic shunt and splenic volume before LT.This examination also avoids additional exposure to radiation and additional costs in assessing SMM.Sarcopenia working groups in Europe and Asia have proposed cutoffvalues for low SMM based on BIA and DXA examinations done in healthy young individuals,but not from CT information.As healthy individuals have no reason to undergo CT, data from such individuals to establish sex-specific cutoffs for CT are lacking.
Fortunately, however, living donors are healthy individuals and healthy individuals can be living donors.So body composition data derived from 657 healthy living liver donors and their corresponding proposed sex-specific cutoffs for the SMM index (SMI), intramuscular adipose tissue content (IMAC) and area and ratio of visceral-to-subcutaneous adipose tissue (VSR) were recently examined in this context by our group [36].Since cutoffs for body composition are likely to differ according to ethnicity, we believe that our obtained values are reliable and could serve as standards for the East Asian populations.Using these novel cutoffs, the negative impact of preoperative physical abnormalities such as muscle steatosis and visceral adiposity on outcomes after LDLT was first clarified [36].
Therefore it was aimed to establish more objective criteria and assess the impact of SMI, IMAC and VSR on OS among adults after LDLT.Other than these variables, there are some parameters assessing sarcopenia including skeletal muscle area (SMA), handgrip strength, and gait speed.We chose these three variables in this study for the following reasons.First, SMI is more popular and accurate to evaluate sarcopenia than SMA, because SMI was calculated by normalizing SMAs at the L3 level including the psoas, erector spinae, quadratus lumborum, transversus abdominis, external and internal obliques, and rectus abdominis for height(cm2/m2).Second, we could measure SMI, IMAC and VSR using pretransplant CT scan in the retrospective analysis.In contrast, we did not measure hand-grip strength and gait speed for all recipients.Third, hand-grip strength and gait speed are not so objective compared with SMI, IMAC and VSR, because these variables can be quantified using respective range of Hounsfield units in pretransplant CT.Accordingly, OS rates were stratified after LDLT according to low SMI, high IMAC, and high VSR [37].Notably, the 1-year OS rate among patients with abnormality in all three of these factors was 41%.Interestingly, incidence of bacteremia was significantly higher in patients with 3 abnormal factors (47%), 2 factors(42%), or 1 factor (37%) than in patients with 0 factor (23%)(P= 0.027) [41].These findings strongly suggest that recipients with preoperative impaired body composition are vulnerable to lethal infection such as bacteremia.As a result of these findings,we recommend that patients harboring all three factors should be oriented towards the DDLT waiting list and undergo nutritional and rehabilitation therapy during the waiting period.Previously,our team showed that OS was significantly higher in sarcopenic patients receiving perioperative nutritional therapy compared to sarcopenic patients who did not [32].Pretransplant exercise for more than one week significantly increased SMM as well as physical activity [42].Taken together, new selection criteria for LDLT was established: patients with ≤2 abnormal body composition factors.Moreover, aggressive perioperative nutritional and rehabilitation therapy for recipients with 1 or 2 abnormal body composition factors became routinely performed since October 2016.Fortunately, no recipient has been excluded from LDLT candidacy solely on the presence of all three abnormal factors since October 2016.Surprisingly, after implementing all the aforementioned improvements, based on extensive clinical research done by the Kyoto transplant team, a current 1-year OS rate of 99% in adult recipients who underwent LDLT between October 2016 and December 2019 has been reached.These short-term outcomes seem to be the highest among high-volume centers around the world.Without exaggeration it can be said that our goal, “low-risk, high-return”state in LDLT, has been achieved.
Most recently, we stumbled upon a great discovery that has not previously been disclosed.Numerous studies have demonstrated that older donor age is a strong risk factor for poor graft function or survival after both DDLT and LDLT [ 7 -9 , 43 , 44 ].The precise reason for this has been unclear so far.We focused not on recipient, but rather on donor body compositions and investigated the relationship between donor muscularity, muscle mass and quality,and graft function or survival.Surprisingly, this study was the first to demonstrate that high muscularity in donors is an independent protective factor for graft survival after LDLT [45].Particularly the combination in male donor and high muscularity resulted in a significantly better one-year graft survival rates after LDLT compared to a control group (97% vs.82%,P= 0.024).Older donor age was also associated with lower donor muscularity.Although the mechanisms by which decreased donor muscularity results in impaired graft function still needs to be elucidated, our findings help to explain why older donor age is a strong risk factor for poor graft function and survival after LT.Not only recipient body composition, but also donor body composition are closely related to therecipient outcomes in LDLT.Selection of living donors with relatively high muscularity might thus be a further key to improve short-term outcomes after LDLT.All these, both donor and recipient, findings clearly show that body composition plays a crucial role in LDLT.
Conclusions
Under a paradigm of “marketing and innovation”, various innovations and effort s have been made during the last decade by the Kyoto transplant team aiming at improving short-term outcome of both donor and recipient.As a result, excellent short-term outcome after LDLT has been achieved, along with some potentially epochmaking discoveries.
Acknowledgments
None.
CRediT authorship contribution statement
Toshimi Kaido :Conceptualization, Writing-original draft,Writing-reviewing & editing.
Funding
None.
Ethical approval
All study protocols shown in this article were approved by the Ethics Committee of Kyoto University and all procedures were conducted in accordance withtheDeclarationofHelsinkiof1996.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Small-for-size syndrome in liver transplantation: Definition,pathophysiology and management
- Endoscopic papillary large balloon dilation with or without sphincterotomy for large bile duct stones removal: Short-term and long-tem outcomes
- Optimizing biliary outcomes in living donor liver transplantation:Evolution towards standardization in a high-volume center
- Hepatic vein in living donor liver transplantation
- Hepatobiliary&Pancreatic Diseases International
- Hepatic artery reconstruction in pediatric liver transplantation:Experience from a single group