Hepatic artery reconstruction in pediatric liver transplantation:Experience from a single group
2020-09-21MingXunFengJiXuZhngPingWnBiJunQiuLiHongGuJinJunZhngQingXi
Ming-Xun Feng Ji-Xu Zhng Ping Wn Bi-Jun Qiu Li-Hong Gu Jin-Jun Zhng Qing Xi *
a Department of Liver Surgery, Renji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai 200000, China
b Department of Ultrasonography, Renji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai 200000, China
Key words:
ABSTRACT
Introduction
The expansion of pediatric liver transplant programs in China led to a markedly improved survival of children affected by endstage liver diseases.However, vascular complications occur far more often in pediatric liver transplantation (PLT) than in adult liver transplantation (LT) because of the small vessel diameter, and vessel quality [1,2].Arterial complications after PLT consist of hepatic artery thrombosis (HAT) and hepatic artery stenosis (HAS).Both complications are crucial for the outcome of the patients.HAT mostly occurs within the first post-LT month resulting in ischemic biliary complication [3]and eventually death [4-6].The present study retrospectively analyzed a large PLT cohort, and aimed to find the incidence, treatment, and prognosis of HAT in PLT.
Methods
This study was approved by the Ethics Committee of Renji Hospital, Shanghai Jiao Tong University School of Medicine [No.2016-134K(C)].Written informed consent was obtained from the guardians of all participants.We did 259 PLTs in the whole year of 2017 (patients<18 years) in a single liver transplantation group in Renji Hospital, Shanghai Jiao Tong University School of Medicine.The median age of the patients was 7 months (range 4-181 months).Thirty-four patients (13.1%) received deceased donor liver transplantation (DDLT), and 225 (86.9%) had living donor liver transplantation (LDLT).The primary diseases leading to LT were as follows: biliary atresia (83.8%), cholestatic diseases (4.2%),metabolic diseases (8.5%) and others (3.5%).The median artery diameter of the living grafts was 1.4 mm (range 1.0-1.8 mm), and the median artery diameter of the recipients was 1.5 mm (range 0.9-1.6 mm) in LDLT.The median follow-up duration was 2.88 years(range 2.42-3.41 years).The characteristics of these patients were shown in Table 1.
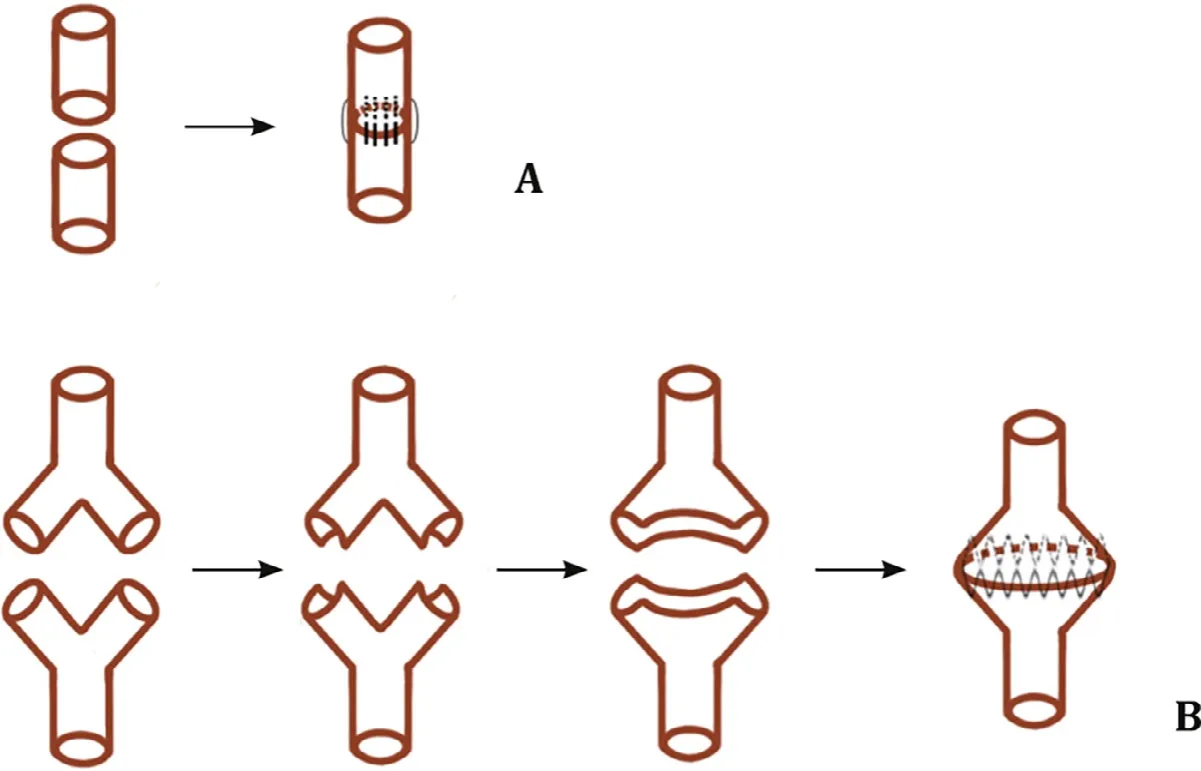
Fig.1.A: Arterial reconstruction in LDLT using interrupted 8-0 or 9-0 Prolene sutures; B: Arterial constellation at DDLT: gastroduodenal artery-common hepatic arterial bifurcations and recipients.Common hepatic artery-splenic arterial bifurcations were transformed into a “horn”like patch.LDLT: living donor liver transplantation; DDLT:deceased donor liver transplantation.

Table 1The baseline of the patients (n = 259).
The choice of hepatic artery reconstruction was based on the type of graft.Microsurgical reconstructions were used in living donor grafts as well as in left lateral lobes from deceased donors(split LT).Arterial reconstruction was performed using an operating microscope (Carl Zeiss Inc., Model S88, Jena, Germany).The reconstruction was done using interrupted 8-0 or 9-0 Prolene(Ethicon Inc., Somerville, USA) sutures (Fig.1 A) [7].Since the common hepatic artery bifurcation was available both in donor and recipient when performing whole liver graft DDLT, the anastomosis was done using continuous suturing in a patch-to-patch fashion.The recipients' arterial bifurcations (gastroduodenal and common hepatic arteries) and donors' arterial bifurcations (common hepatic and splenic arteries) were chosen to make a “horn”like patch;anastomosis were done using 2.5 ×magnifying glasses (Fig.1 B).
Intra-operative color Doppler flow imaging (CDFI) was used to monitor both arterial patency and blood flow velocity.Hepatic arterial peak systolic velocity and resistance index were routinely recorded afterwards once daily within the first 7 days after LT, and at post-LT day 14 before discharging the patients.Afterwards CDFI was performed every 6 months during the outpatient visits if no hepatic artery flow was detected.Angio-CT scan was performed to confirm the arterial problem.
All recipients received a heparin sodium IV-drip as routine anticoagulation therapy in order to prevent HAT during two weeks after LT.The management of HAT was mainly determined by the interval between the LT and the occurrence of the thrombotic event.In case of an acute HAT defined as an event happening within 5 days post-LT, surgical re-anastomosis was recommended within 12 h after the detection of HAT.
When HAT occurred after 6 days post-LT, a conservative anticoagulation therapy was usually adopted.An oral anti-coagulation(anti vitamin-K agent, warfarin) was added to the heparin-based anticoagulation therapy in order to keep an international normalized ratio value of between 1.8 and 2.2.Prophylactic antibiotherapy was used simultaneously to prevent potential abscess formation caused by HAT.
Statistical analysis
Non-normally distributed data were described as median values and range.Statistical analysis was done using IBM SPSS Statistics 23.0 (IBM Corp., Armonk, NY, USA).Because the frequency of HAT was less than 5 in the LDLT and DDLT groups, the comparison of HAT incidence in LDLT and DDLT was calculated with Fisher's exact test, and aP<0.05 was considered statistically significant.
Results
HAT occurred in 5 patients (1.9%) and no HAS was detected during the follow-up.Four patients had a whole graft DDLT whilst only one patient receiving a left lateral lobe LDLT developed HAT(P= 0.001).All HATs were diagnosed between postoperative day(POD) 3 and 9 (Table 2).
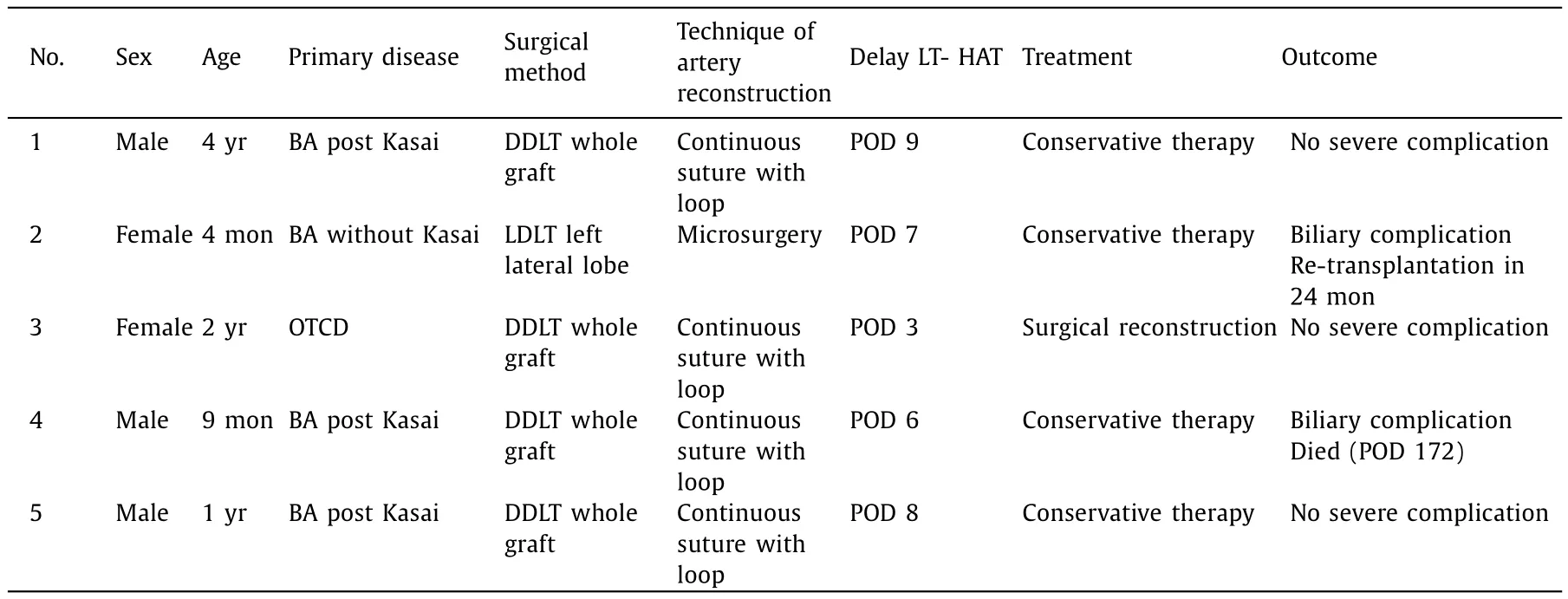
Table 2HAT after pediatric liver transplantation patients.
All 5 HAT patients were first detected at routine CDFI.Angio-CT scan confirmed the diagnosis in all 5 patients.After enhanced anticoagulation using warfarin, four hepatic arteries recanalized.Surgical re-anastomosis was only necessary once.Two patients developed severe biliary complications despite reinforced anticoagulation in unmanageable biloma and diffuse bile duct dilation.One needed to be re-transplanted two years later, and the other died of biliary complications at post-LT day 172.
Discussion
Vascular complications after LT are vital for the outcome of the patients.HAT merely happens in early posttransplantation period and it is one of the main causes of early graft and patient loss [8].According to the meta-analysis reported by Bekker et al.[9]., PLT has a significantly higher incidence of HAT than adult LT (2.9% vs.8.3%,P<0.001) leading to an important mortality rate reaching even 25%.Thus, close attention should be paid to prevent and monitor the occurrence of HAT in PLT.
The risk factors of HAT in PLT include the young age of patients, the use of DDLT [10]or use of both large [11]and small[12]graft volume/recipient body weight ratio grafts and inadequate length of hepatic artery [13].In our experience we observed indeed that DDLT using whole liver graft led to a much higher incidence of hepatic artery complications than LDLT (11.8% vs.0.4%,P= 0.001), which was consistent with Zhang's study [10].Our experience indicated that the grafts from pediatric deceased donors have smaller diameters and suffer more ischemic injury compared to LDLT grafts.Besides this, the patch-to-patch reconstruction frequently used in DDLT is more likely to result in hepatic artery redundancy following reconstruction.The arterial blood flow is more frequently compromised in pediatric DDLT thereby leading to HAT,and one should be aware of the risk of HAT when using such allografts.
Starzl was the first to advocate the microsurgical technique in PLT in 1976 [14]in order to improve the quality of artery reconstruction and to decrease the incidence of HAT [15].
Although whether the technique of microsurgical reconstruction in PLT decreases the incidence of HAT remains a matter of debate [12], we support this modality because this technique can cope with all differently encountered intra-operative anatomical situations of artery reconstruction, thus improving the quality of artery reconstruction especially when the diameter of artery is ≤2 mm [16].
HAT is also related to the proficiency of the surgery and the surgeon [9].HAT occurs more likely in PLT centers performing less than 30 LTs annually.Therefore, these procedures as well as the microsurgical reconstruction techniques should be reserved to experienced PLT centers.
Currently, CDFI is one of the most important methods to monitor the vascular reconstructions after LT.Kutluturk et al.[11]recommended daily CDFI after PLT for the first week after transplantation in order to detect this dreadful complication in time.Technical difficulties and delays to revascularize hepatic artery during the procedure pose a risk of critical ischemic damage to the biliary tree of the liver graft [17].Therefore, early detection and intervention of HAT are indeed the key to treat HAT patients [18].Previous studies demonstrated that hepatic artery resistance index<0.6 has a high sensitivity (95.2%) and specificity (81.8%), allowing to predict the occurrence of HAT.CDFI represents therefore a major help for the surgeon to tackle this problem and allows preemptive treatment of HAT [19].Angio-CT scan was used to confirm the HAT when there was a suspicion.It is reported that contrast-enhanced ultrasound has higher sensitivity and accuracy in diagnosing HAT [20], which may help surgeons to detect HAT in time.
The “frontline”treatment of HAT consists of surgical and/or endovascular treatment [21-23].Indeed, conservative treatment leads to a high mortality rate.Our data suggest that pediatric patients receiving conservative treatment may however have the similar prognosis to those who received surgical or endovascular treatment [24].A therapeutic algorithm for HAT in PLT should be mainly based on the delay between the transplant procedure and the moment of the HAT diagnosis and the type allograft: HAT happening within one week after transplantation is most likely related to surgical deficiency and needs surgical or endovascular treatment; if happening late, especially in the context of whole graft DDLT, conservative treatment (using efficacious anticoagulation) is a preferred option.Also, the type of transplantation plays a role.HAT in LDLT is more lethal than whole graft DDLT due to the very different way of arterial collateralization which is more rapid in whole than in partial (in the case of PLT, left lateral lobe) LT.The treatment of HAT in LDLT should therefore be more aggressive.According to the experience of Park et al.[21], right gastroepiploic artery is preferred in re-anastomosis surgery, and reanastomosis of biliary duct is necessary in most cases in adult LDLT.In this study, one patient had an HAT on POD 3, and he recovered smoothly after receiving arterial re-anastomosis, using the previous hepatic artery without re-anastomosis of biliary duct.After 3 years of follow-up, the four other patients, who presenteda delayed HAT, regained hepatic artery flow under anticoagulation therapy; two recovered smoothly without any complications, and one of who received LDLT developed refractory biliary complications.
The limitation of this study is that the number of HAT patients is small which affects the accuracy of statistical analysis.Further study with larger cohort is necessary.Also, the study is a retrospective study, which cannot eliminate the biases.Therefore, a well-designed randomized controlled trial is necessary to articulate the advantage of microsurgical technique.
In conclusion, microsurgical techniques significantly improve the outcome of the arterial reconstruction in PLT.The risk for arterial complication is significantly higher in DDLT.Aggressive surgical or endovascular treatment is necessary if HAT occurs early after transplantation.Conservative therapy can achieve good outcome in selected pediatric patients.
Acknowledgments
None.
CRediT authorship contribution statement
Ming-Xuan Feng:Data curation, Conceptualization, Formal analysis, Writing - original draft.Jia-Xu Zhang:Data curation,Conceptualization, Formal analysis, Writing - original draft.Ping Wan:Data curation, Formal analysis.Bi-Jun Qiu:Data curation.Li-Hong Gu:Data curation.Jian-Jun Zhang:Conceptualization, Supervision.Qiang Xia:Conceptualization, Funding acquisition, Supervision, Writing - review & editing.
Funding
This project was supported by grants from the National Key R&D Program of China (2017YFC0908100); Cohort Study of HCC and Liver Diseases, Double First-Class Foundation, Shanghai Jiao Tong University (W410170015); Overall Leverage Clinical Medicine Center, NHFPC Foundation (2017ZZ01018); Key Clinical Subject Construction Project of Shanghai (shslczdzk05801); and Shanghai Shenkang Three-year Program (16CR1003A).
Ethical approval
This study was approved by the Ethics Committee of Renji Hospital, Shanghai Jiao Tong University School of Medicine [No.2016-134K(C)].Written informed consent was obtained from the guardians of all participants.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Small-for-size syndrome in liver transplantation: Definition,pathophysiology and management
- Endoscopic papillary large balloon dilation with or without sphincterotomy for large bile duct stones removal: Short-term and long-tem outcomes
- Recent evolution of living donor liver transplantation at Kyoto University: How to achieve a one-year overall survival rate of 99%?
- Optimizing biliary outcomes in living donor liver transplantation:Evolution towards standardization in a high-volume center
- Hepatobiliary&Pancreatic Diseases International
- Techniques for overcoming atretic changes of the portal vein in living donor liver transplantation