Prognostic factors influencing outcome in adult liver transplantation using hypernatremic organ donation after brain death
2020-09-21ZhengJunZhouGuangShunChenZhongZhouSiQiangLiYangYangBinHaiZhiQiJieQunLi
Zheng-Jun Zhou , Guang-Shun Chen , Zhong-Zhou Si, Qiang Li, Yang-Yang Bin, Hai-Zhi Qi,Jie-Qun Li
Center of Organ Transplantation, The Second Xiangya Hospital of Central South University, Changsha 410011, China
Keywords:
ABSTRACT
Introduction
Methods
Study population
Between January 2013 and June 2018, the data for all adult (≥18 years old) deceased donor LT performed in the Second Xiangya Hospital of Central South University were reviewed (n= 600).Re-LT patients and patients of allografts harvested from organ donation after cardiac death were ruled out (n= 14), and the remaining 586 organ donation after brain death (DBD) were included in the study.The follow-up period for the entire cohort was 1 year.According to the donor serum sodium levels immediately before procurement, 586 recipients were divided into three groups:group 1 (normal sodium), sodium levels of donor<155 mmol/L(n= 4 4 4); group 2 (moderate high), sodium levels ≥155 mmol/L,but<170 mmol/L (n= 92); and group 3 (severe high), sodium levels ≥170 mmol/L (n= 50).In order to investigate the effects of the exposure time of liver grafts from hypernatremia to reperfusion on the outcomes of liver transplantation, the exposure time was defined as the period of continuous high sodium levels(≥155 mmol/L) until the reperfusion of the donor liver (UW solutions are also hyperosmolar).And we found that recipients from our center using hypernatrimic organs with the exposure more than 36 h had comparatively negative outcome post-LT.Therefore,the 142 patients with sodium levels ≥155 mmol/L (groups 2 and 3) were subdivided into two further subgroups: subgroup A, the exposure time was shorter than 36 h (n= 119); and subgroup B, the exposure time was ≥36 h (n= 23).In cases when the donor had recurrent hypernatremia, the normal process was repeated, and the duration of the last incidence of hypernatremia was taken as the standard.The study protocol was conformed to the1975DeclarationofHelsinkiand was approved by the Ethical Committee of the Second Xiangya Hospital of Central South University No.2019-050).
Operative procedure and immunosuppression therapy
All instances of organ donation were performed according to the protocols of China.The donor livers were procured using rapid donor liver procurement including aortic and portal vein flushingand cold storage as previously described [10].All hepatic allografts were perfused and preserved using University of Wisconsin (UW)solution.The operative procedure was performed by the same surgical team with similar standard techniques or piggyback methods.The recipients received ATG-Fresenius or Basiliximab as part of the induction protocol.Posttransplant immunosuppression included 500 mg intravenous methylprednisolone during the anhepatic phase.Tacrolimus was administered 48 h post-transplant at an initial dose of 0.04 mg/kg twice daily, with a subsequent dose adjustment to achieve proper blood concentration.Mycophenolate mofetil (0.75 g, Q12h) was initiated at posttransplant day 2.
Outcomes
Early graft function, including aspartate transaminase (AST),alanine transaminase (ALT), total bilirubin (TB), and prothrombin time (PT) were recorded at day 1, 3, 7 and 14 after LT.Outcomes included 1-year survival rates of grafts and recipients, 1-year graft loss, acute rejection, and biliary and vascular complications.Graft rejection was diagnosed by liver biopsy or clinical diagnosis.Vascular complications included thrombosis and stenosis of the hepatic artery and portal vein.Biliary complications included biliary stricture changes, bile leakage and ischemic biliary injury.
Statistical analysis
Continuous or categorical variables were presented as medians[interquartile range (IQR)], percentages or ratios, separately.Comparison between groups was performed using the Kruskal-Wallis test, Mann-WhitneyUtest, Pearson's Chi-squared test or Fisher's exact test in SPSS 11.0 (IBM Corp., Armonk, New York, NY, USA).The proportional hazards assumption was conducted on the risk factors affecting graft loss in the hypernatremic donors, and statistically significant risk factors were included, and Cox proportional hazards regression model analysis was used.Differences withPvalues<0.05 were considered statistically significant.
Results
Influence of donor serum sodium levels on early outcomes of LT
Among the 586 deceased donor LT between January 2013 and June 2018, 92 recipients received a liver graft with serum sodium levels ≥ 155 and<170 mmol/L; 50 with serum sodium levels ≥170 mmol/L.Except for donor's age, there were no differences in donor sex, body mass index (BMI), cause of death, liver function and ICU stay (Table 1).The clinical characteristics of recipients and operations among the three groups demonstrated no differences in age, sex, model for end-stage liver disease (MELD) score, percent-age of acute-on-chronic liver failure (ACLF) [11], cold ischemia time(CIT), warm ischemia time (WIT) [12], operative time and volume of intraoperative transfusion (Table 1).
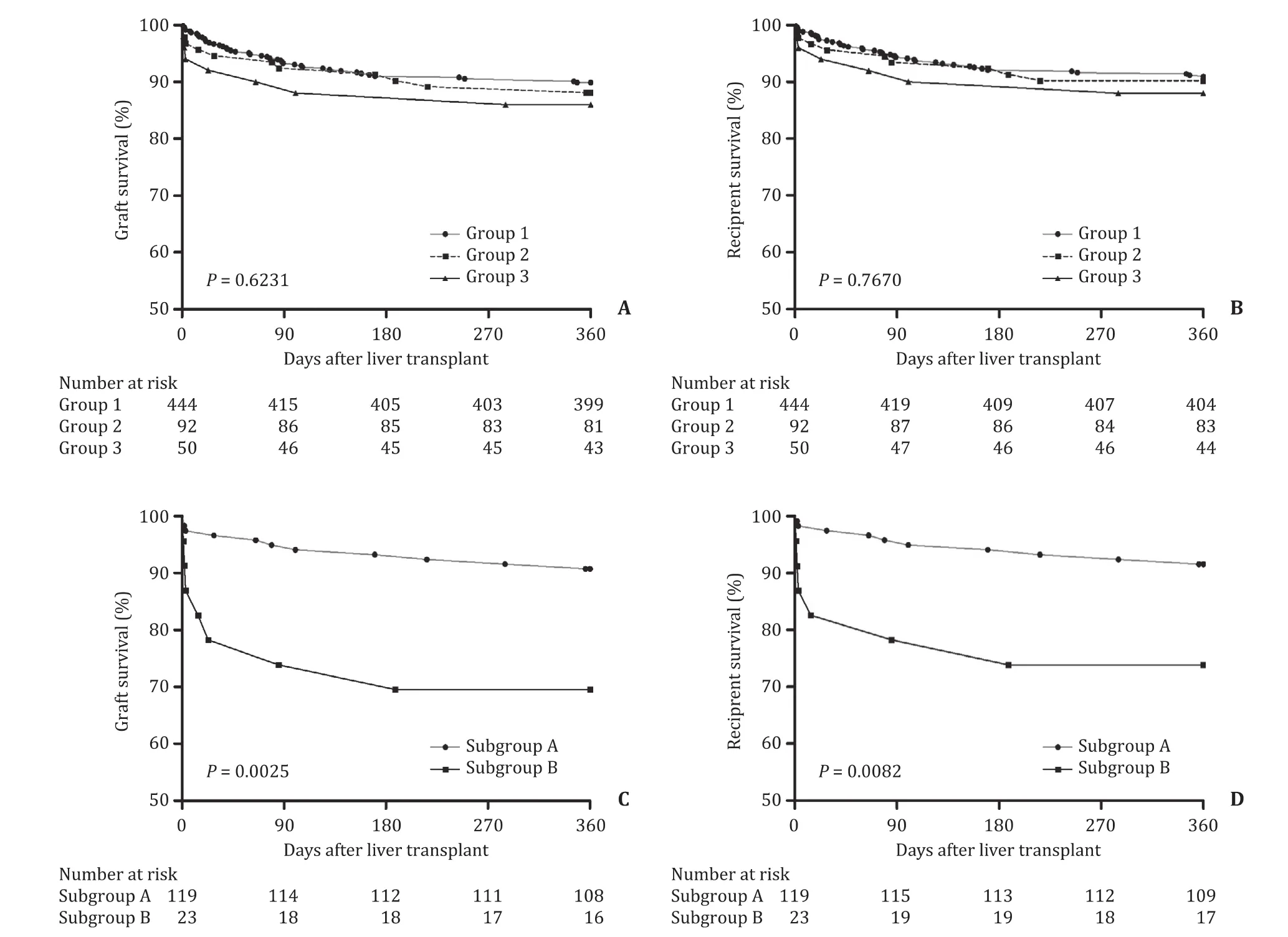
Fig.2.Kaplan-Meier curve for survival analysis of grafts and patients.A & B: Survival analysis of garfts and patients; C & D: Survival analysis of garfts and patients between subgroup A (< 36 h) and subgroup B (≥36 h).
Compared with group 1 (normal sodium), there were significantly increased liver enzyme values (AST and ALT) and prolonged PT levels at postoperative day 1 and 3 in groups 2 and 3; however,all of these values were similar at day 7 and thereafter (Fig.1).The values of TB during the 14 days after transplant were similar among groups (Fig.1).
Table 1 also summarizes the postoperative outcome measures in the 3 groups.There were no statistically significant differences of 1-year graft loss and early events (acute rejection, biliary and vascular complications).Kaplan-Meier analysis demonstrated no significant difference in grafts and recipients survival up to 1-year following LT among the three groups (Fig.2 A, B).
35.The forest: Woods or forests frequently appear as settings in fairy tales. Forests symbolize the female principle, the unconscious, danger, mistakes, problems, fertility, and enchantment68. They often serve as the homes for outlaws69 such as in the Robin70 Hood71 legend, fairies, or supernatural beings (Olderr 1986).Return to place in story.
Impact of the exposure time of liver grafts from hypernatremia to reperfusion on early outcomes of LT
There were 119 patients in subgroup A and 23 patients in subgroup B.The CIT in subgroup B was significantly shorter than that in subgroup A, which may be attributed to our effort s to reduce the CIT in cases with hypernatremic donors, especially to hepatic allografts of the exposure time ≥36 h.There were no other statistically significant differences in the characteristics of both donors and recipients (Table 2).
AST was increased significantly in subgroup B at day 1, 3 and 7 after LT (Fig.3).The values of ALT and PT in subgroup B were significantly higher than those in subgroup A at day 1 and 3 (Fig.3).The frequency of 1-year graft survival in subgroup A was significantly higher than that of subgroup B.Kaplan-Meier analysis showed poorer overall survival of grafts (Fig.2 C,P= 0.0025) and recipients (Fig.2 D,P= 0.0082) in subgroup B than those in subgroup A.
Multivariate analysis of the prognostic factors
Multivariate Cox regression analysis showed that donor age, ICU stay and cardiopulmonary resuscitation (CPR), as well as recipient MELD score and CIT, had significant impact on recipient outcomes(Table 3).This is consistent with the aforementioned results that donor serum sodium levels had no influence on the early outcomes of recipients.
Multivariate analysis of the prognostic factors based on hypernatremic donors
The results of Cox-proportional hazard regression analysis were shown in Table 4.The data suggested that the exposure time of liver grafts from hypernatremia to reperfusion (HR = 1.117; 95% CI:1.053-1.186;P<0.001), and CIT (HR = 1.015; 95% CI: 1.006-1.024;P = 0.001) MELD (HR = 1.061; 95% CI: 1.003-1.121;P= 0.037) had a significant negative effect on the outcomes in recipients of hepatic allografts from hypernatremic donors.Consistent with the results in Table 2 , the exposure time and CIT were the important prognostic factors associating with the poor outcomes in recipients receiving hypernatremic donors.

Table 2Donor and recipient characteristics, LT procedure and early graft outcomes in different subgroups with the exposure time of liver grafts from hypernatremia to reperfusion.

Table 3Multivariate Cox regression model analysis on the prognostic factors of recipient outcomes based on the entire population.
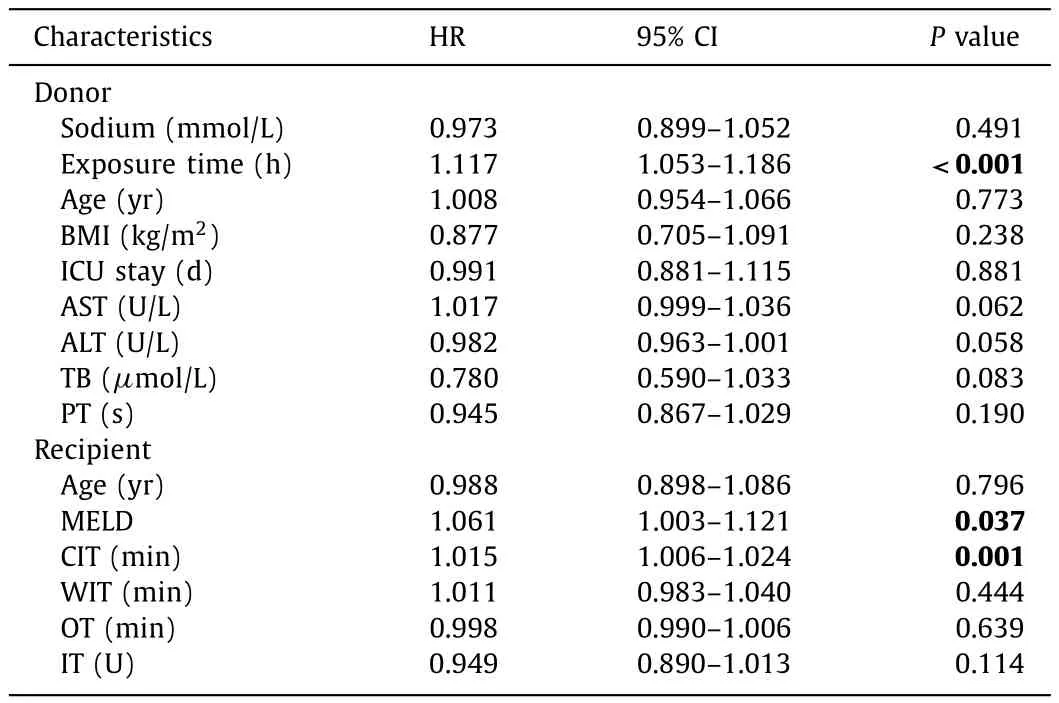
Table 4Multivariate Cox regression model analysis on the prognostic factors of recipient outcomes using grafts exposed from hypernatrimia to reperfusion.
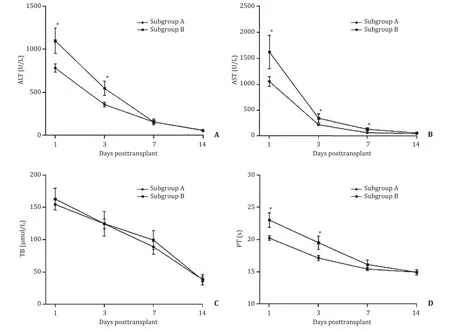
Fig.3.Posttransplant ALT, AST, TB and PT in subgroups A and B.*: P < 0.05, vs. subgroup B.ALT: alanine transaminase; AST: aspartate transaminase; TB: total bilirubin; PT:prothrombin time.
Discussion
In the present study, the newest research materials were extracted from a single center from January 2013 to June 2018.In addition, no published study has ever identified the unfavorable prognostic factors associated with poor outcomes in LT patients receiving hepatic allografts from hypernatremic donors.We found that the effect of hypernatremia on early liver graft function is limited.There were no significant differences in the 1-year survival rates of grafts and recipients, 1-year graft loss rates and early events among the groups with different levels of serum sodium.However, when we subdivided the exposure time of liver grafts from hypernatremia to reperfusion into<36 h (subgroup A) and ≥36 h (subgroup B), the frequency of 1-year graft loss in subgroup B was significantly higher than that of subgroup A.Kaplan-Meier analysis also showed poorer overall survival of grafts and recipients in subgroup B.Importantly, the results of Cox-proportional hazard regression analysis showed that the exposure time and CIT are the important poor prognostic factors of liver recipients.
These results are in accordance with preceding researches in adult or pediatric LT recipients [ 2-4 , 13-15 ].However, other studies have also found conflicting results, suggesting that donor hypernatremia had a negative impact on the outcome of LT.In the 1990s,a number of studies have found that donor hypernatremia resulted in a greater incidence of PNF, poorer graft function, and an increased risk of early graft loss after LT [ 7-9 , 16 , 17 ].Soon afterwards,Totsuka et al.[18]demonstrated that donor hypernatremia (Na+>155 mmol/L) as well as WIT and CIT independently affected graft survival.Pokorny et al.[6]also showed that peak serum sodium>155 mmol/L was an independent predictor with the highest significance for PNF.Another study by Markmann and associates found that peak serum sodium ≥170 mmol/L had independent prognostic significance for primary liver graft outcomes [19].
Elevated donor serum sodium is one of the most common complications after brain death.A previous study suggested that liver allograft injury related to donor hypernatremia occurs at the time of procurement, during cold storage, or at reperfusion [8].An increased intracellular osmolality in the graft results in a fluid shift toward the graft leading to graft congestion, hepatocyte death and graft dysfunction [ 7 , 8 ].This difference in intracellular and extracellular osmolality causes cell swelling, which in turn exacerbates reperfusion injury [ 7 , 20 ].However, there is no uniformly accepted mechanism to explain how donor hypernatremia can negatively impact allograft function.Cywinski et al.[5]suggested the serum sodium differences between recipients of orthotopic liver transplantation and cadaveric donors (△ Na+), which would determine osmolality gradient between extracellular and intracellular compartments, does not affect immediate postoperative allograft function and short-term patient outcomes.Previous study also showed that the correction of donor hypernatremia before organ procurement improved both graft function and survival, which suggested that latent changes in hepatocytes induced by hypernatremia arereversible and might be attenuated by appropriate donor management [8].Further studies are needed to elucidate the exact mechanism of osmolality inducing liver allograft injury.Pathological examination of allografts to search specific osmotic injury may be very meaningful for assessment of donor quality.In the present study, hypernatremic donors induced significantly higher liver enzyme values and prolonged PT levels at the postoperative day 1 and 3, however, all of these values were similar by day 7 and thereafter.There was no suggestion of an increase of either ALT,AST, TB or PT with increasing levels of hypernatremia, which would be expected in the existence of a dose-response effect.
One possible explanation for the disparity in prognosis with other studies is the exposure time of liver grafts from hypernatremia to reperfusion.Because UW solutions are slightly hyperosmolar [21], the liver graft harvested from a hypernatremic donor will be exposed to hyperosmolar solutions until reperfusion.CIT,the time of liver graft exposure to hyperosmolar solutionsinvitro,is considered a part of the exposure time of liver grafts.In the present study, Cox proportional hazard regression analysis showed that both the exposure time and CIT are important prognostic factors contributing to the poor outcomes in recipients receiving grafts from hypernatremic donors.At our center, we are extremely careful to donors with a longer exposure time from hypernatremia to reperfusion.If possible, we tried to correct donor hypernatremia before organ procurement by dialysis or infusion of hyponatremic solution, and only 23 cases exceeded 36 h.Furthermore, almost all of the donor liver allografts transplanted at our center were imported regionally, which made it possible to control the CIT.The organ procurement procedure of all donors rarely lasted more than 2 h, followed by rapid transport and transplantation with a median CIT of about 8 h.Moreover, the median CIT of the liver grafts from subgroup B was only 6 h.In the present study, the duration that the liver grafts from hypernatremia to reperfusion was very short.
In this study, there were no statistically significant differences in the outcomes of patients among the three groups, suggesting that the degree of hypernatremia had no effect on patient outcomes under the described conditions.However, even with the shorter CIT, the frequency of 1-year graft loss in subgroup B was significantly higher than that of subgroup A.Kaplan-Meier analysis also showed poorer overall survival of recipients in subgroup B.Consequently, reducing the exposure time of liver grafts from hypernatremia to reperfusion is of great importance.
In conclusion, in recipients who received liver allografts from hypernatremic donors, minimization of the exposure time of liver grafts from hypernatremia to reperfusion is critical to transplantation success.
Acknowledgments
None.
CRediT authorship contribution statement
Zheng-Jun Zhou:Conceptualization, Data curation, Methodology, Writing - review & editing.Guang-Shun Chen:Data curation,Resources, Investigation.Zhong-Zhou Si:Writing - review & editing.Qiang Li:Software.Yang-Yang Bin:Data curation.Hai-Zhi Qi:Writing - review & editing.Jie-Qun Li:Conceptualization, Funding acquisition, Writing - original draft, Writing - review & editing.
Funding
This study was supported by grants from the Natural Science Foundation of Hunan Province , China (No.2018JJ2561) and the National Natural Science Foundation of China (No.81102241).
Ethical approval
The study was approved by the Ethical Committee of the Second Xiangya Hospital of Central South University (No.2019-050).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Recent evolution of living donor liver transplantation at Kyoto University: How to achieve a one-year overall survival rate of 99%?
- Endoscopic papillary large balloon dilation with or without sphincterotomy for large bile duct stones removal: Short-term and long-tem outcomes
- Optimizing biliary outcomes in living donor liver transplantation:Evolution towards standardization in a high-volume center
- Hepatic vein in living donor liver transplantation
- Hepatobiliary&Pancreatic Diseases International
- Hepatic artery reconstruction in pediatric liver transplantation:Experience from a single group