Impact of treatment modalities on patients with recurrent hepatocellular carcinoma after liver transplantation: Preliminary experience
2020-09-21ZheYngShuoWngXinYoTinQinFenXieLiZhungQiYongLiChengZeChenShuSenZheng
Zhe Yng , Shuo Wng , Xin-Yo Tin , Qin-Fen Xie , Li Zhung , Qi-Yong Li ,Cheng-Ze Chen , Shu-Sen Zheng , , c , *
a Department of Hepatobiliary and Pancreatic Surgery, Department of Liver Transplantation, Shulan (Hangzhou) Hospital, Zhejiang Shuren University School of Medicine, 848 Dongxin Road, Hangzhou 310022, China
b Division of Hepatobiliary Pancreatic Surgery, the First Affiliated Hospital, Zhejiang University School of Medicine, 79 Qingchun Road, Hangzhou 310 0 03,China
c National Clinical Research Center of Infectious Diseases, 79 Qingchun Road, Hangzhou 310 0 03, China
Keywords:
ABSTRACT
Introduction
Hepatocellular carcinoma (HCC) is the sixth most common cancer worldwide and the fourth major cause of cancer-related death [1].Because of the high prevalence of hepatitis B virus (HBV)infection and liver cirrhosis, 55% of the new cases and deaths occur in China [2].As a potentially curative treatment for liver cirrhosis and cancer, liver transplantation (LT) is widely used for the treatment of selected patients with early-stage HCC, and it brings the most benefit compared with other treatments [3].However, posttransplant tumor recurrence is considered the most important factor in limiting the long-term survival of patients.
Current treatment options include surgical resection, transarterial chemoembolization (TACE), systemic chemotherapy, radiofrequency ablation (RFA), external beam radiation and molecular targeted therapy [4].A few studies have addressed the effect of surgical management in patients with post-LT HCC recurrence [ 5 , 6 ].However, the evidence level of recommendations is weak, and there is still no consensus on a standard of care for recurrent HCC after LT.
This study aimed to evaluate the efficacy and safety of various treatments for patients with recurrence of HBV-related HCC post-LT in a Chinese population.We also aimed to identify the risk factors associated with mortality after HCC recurrence and to identify a subset of patients who may benefit from more aggressive therapy.
Methods
Patients
A total of 64 patients with HCC recurrence post-LT from April 2016 to June 2018 were included in this study.Of these patients,HCC was diagnosed either before or after LT, which was confirmed by histopathological examination.Complete clinical and laboratory data were available before surgery and during follow-up.This study was approved by the local ethics committee, and informed consents were obtained from all of the patients.
Post-transplant immunosuppression
Post-transplant immunosuppression was tacrolimus-based (6-10 ng/mL within 3 months, 3-5 ng/mL within 6-12 months,and<3 ng/mL beyond 12 months) and a glucocorticoid was given 10 0 0 mg intraoperatively with a steroid-free regimen posttransplantation.Basiliximab was administered 20 mg on the first and fourth day post-operation.Mycophenolate mofetil (MMF)or mycophenolic acid (MPA) was administered in case of renal dysfunction or as an additional immunosuppressant.Thirtyone patients (48.4%) received tacrolimus-based immunosuppressive therapy, while 33 patients (51.6%) were converted to sirolimusbased therapy (sirolimus monotherapy or sirolimus with reduced tacrolimus) after HCC recurrence.
Follow-up
According to the follow-up course and diagnostic criteria of recurrence that have been described previously [7], the patients were followed up closely at the outpatient clinic from the date of operation to that of death or the last follow-up.Tumor recurrence was monitored by alpha-fetoprotein (AFP), vitamin K absence/antagonist-II (PIVKA-II), ultrasonography, and chest and abdominal computed tomography scans every 3 months for the first 2 years and every 6 months thereafter.Recurrence was identified by elevation of tumor biomarkers (AFP or PIVKA-II) and positive imaging findings.The median follow-up was 10.2 months (0.2-32.1 months) after HCC recurrence.
Management of tumor recurrence
Treatment options were discussed by a multidisciplinary team consisting of surgeons, hepatologists, radiologists and oncologists.Treatment modalities for recurrent HCC include surgical, nonsurgical locoregional and systemic therapies.Resection was proposed to each patient whenever feasible.Locoregional therapies such as TACE and/or RFA were proposed to patients with unresectable intrahepatic lesions.External beam radiotherapy was used as the first-line treatment for bone metastasis.Systemic chemotherapy and/or tyrosine kinase inhibitors (sorafenib, regorafenib, lenvatinib)were administered for multifocal recurrence in intrahepatic and extrahepatic locations.
Statistical analysis
For descriptive statistics, continuous variables were reported as medians and interquartile ranges, and categorical variables werereported as percentages.Overall survival (OS) and cumulative recurrence rates were analyzed by the Kaplan-Meier method, and the differences between groups were estimated by the log-rank test.Independent prognostic indicators were assessed in univariate and multivariate analyses using the Cox proportional hazard model.Statistical analyses were performed using SPSS for Windows (Version 16, SPSS Inc., Chicago, IL, USA).APvalue<0.05 was considered statistically significant.

Table 1Demographic characteristics of recurrence following liver transplantation in 64 patients.
Results
Characteristics of recurrence following LT
Of the 293 HCC patients who underwent LT during the study period, 64 (21.8%) developed recurrent HCC and were included in this study.Characteristics of HCC recurrence and post-LT treatment are summarized in Table 1.The median age was 48 years (41-55 years).Majority of the patients were male (n= 58; 90.6%).The underlying disease in all of the patients was HBV-related cirrhosis.Concerning the pathology of extracted liver, 54 (84.4%) patients had a total tumor size larger than 8 cm, 55 (85.9%) had multifocal tumor, 34 (53.1%) had poorly differentiated HCC, 15 (23.4%) had microvascular invasion, 49 (76.6%) had portal vein tumor thrombosis, and 57 (89.1%) were beyond the Hangzhou criteria.
The median survival following recurrence was 306 days (149-579 days).At the time of tumor recurrence, the median AFP leveland neutrophil-to-lymphocyte ratio (NLR) was 93.3 ng/mL (4.5-1297.1) and 3.0 (1.9-5.1), respectively.81.3% of patients with recurrent HCC developed multiple recurrent nodules, and 18.8% developed only a single nodule.Tumor recurrence sites most commonly involved the lung (50%), followed by liver allograft (42.2%), abdomen (28.1%), bone (12.5%), chest (mediastinum, pleural) (4.7%),and brain (1.6%).The majority of patients developed extrahepatic recurrence (54.7%), followed by intrahepatic recurrence (23.4%) and both intrahepatic and extrahepatic locations (21.9%).

Fig.1.Overall survival following post-transplant HCC recurrence stratified by treatment modalities for the recurrent tumor.OS: overall survival; MS: median overall survival.
Management of post-LT recurrence
Treatment for recurrent HCC most commonly included tyrosine kinase inhibitors (67.2%), systemic chemotherapy (42.2%), surgical resection (25.0%), TACE (21.9%), external beam radiation (17.2%),RFA (9.4%), immunotherapy (3.1%) and best supportive care (15.6%).The majority of patients received only nonsurgical therapy (60.9%),followed by a combination of surgical and nonsurgical therapies(25.0%), and best supportive care without cancer treatment (14.1%).Patients receiving radical resection followed by nonsurgical therapy had a median OS of 20.9 months after HCC recurrence, which was significantly superior to patients receiving only nonsurgical therapy (9.4 months) or best supportive care (2.4 months).The oneand two-year OS following recurrence were favorable for patients receiving radical resection followed by nonsurgical therapy (93.8%,52.6%), poor for patients receiving only nonsurgical therapy (30.8%,10.8%), and dismal in recipients receiving best supportive care (0%,0%; overallP<0.001; Fig.1).
Median OS in sorafenib-tolerant patients treated with lenvatinib was 19.5 months, which was significantly better than sorafenib discontinuation or regorafenib after sorafenib failure patients (12 months,P<0.001).The one- and two-year OS after HCC recurrence were best in sorafenib-tolerant patients treated with lenvatinib (81.8%, 71.6%), followed by sorafenib discontinuation or regorafenib after sorafenib failure patients (46.9%, 15.4%) and those without tyrosine kinase inhibitors (14.3%, 4.8%;P<0.001).Median OS in sirolimus-based immunosuppressive patients was 12.8 months, which was significantly better than tacrolimus-based patients (7.3 months).Compared with tacrolimus-based immunosuppressive therapy, OS was significantly increased with sirolimusbased therapy at one and two years after HCC recurrence (54.5%,25.0% vs.29.0%, 14.5%;P= 0.035; Fig.2).
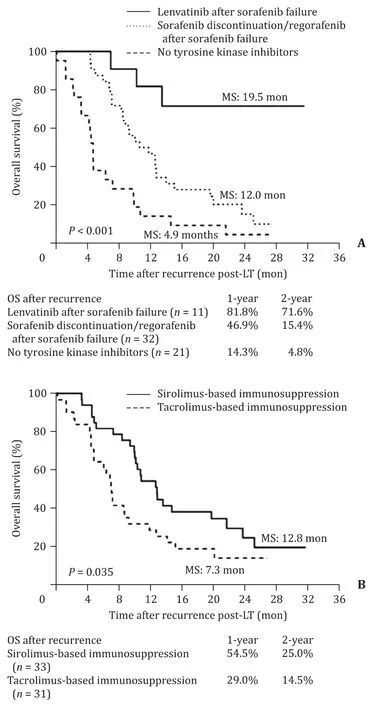
Fig.2.Overall survival following post-transplant HCC recurrence according to the administration of different tyrosine kinase inhibitors (A) and immunosuppressants(B).OS: overall survival; MS: median overall survival.
Of 16 patients who received surgery, interventions included lung resection (n= 7), hepatectomy (n= 4), abdomen (extrahepatic) (n= 2), liver and lung metastasis resection (n= 2), and liver and abdominal metastasis resection (n= 1).Seven sorafenibtolerant patients were treated with lenvatinib and 9 received regorafenib after sorafenib failure or discontinuation of sorafenib.Three patients underwent tacrolimus-based immunosuppressive therapy and 13 received sirolimus-based therapy.Of 6 patients who received surgery, followed by sorafenib-lenvatinib therapy and sirolimus-based immunosuppression, the two-year OS after HCC recurrence was 80%.

Table 2Risk factors on overall survival after post-transplant HCC recurrence.
Predictors of mortality following post-LT HCC recurrence
This study attempted to identify factors that could predict mortality in patients with recurrent HCC after LT (Table 2).In the univariate analysis, factors associated with an increased rate of mortality following post-LT HCC recurrence included early recurrence (<6 months), multiple recurrent nodules, NLR at relapse>3.0, non-sorafenib-lenvatinib therapy, tacrolimus-based immunosuppression and best supportive care.In the multivariate analysis,independent beneficial factors of improved post-recurrence survival rate included surgical intervention for recurrent HCC [hazard ratio (HR), 0.012; 95% confidence interval (CI), 0.003-0.052;P<0.001]and sorafenib-lenvatinib sequential therapy (HR, 0.187;95% CI, 0.051-0.687;P= 0.012).
Discussion
After the application of stringent selection criteria of LT candidates, outcomes following LT for HCC have dramatically improved [8-11].Despite this, post-LT HCC recurrence still occurs in approximately 20% of patients and drastically affects their survival [8].Treatments for HCC recurrence have an immense impact on OS after LT [ 5 , 6 , 12-15 ].However, previous studies are sample size limited and mainly based on Western populations, and there is still considerable debate on the prevention and management of HCC recurrence in post-LT patients [16].Current treatment modalities include a wide range of various therapies, such as surgical resection, nonsurgical locoregional and systemic (cytotoxic or molecular targeted) therapies [4].
This study showed, for the first time, that aggressive surgical intervention followed by tyrosine kinase inhibitors and sirolimusbased immunosuppression significantly improved the survival after tumor recurrence in a Chinese HBV-related HCC LT cohort.In the present study, the majority of recipients developed advanced HCC,with 76.6% of patients having portal vein tumor thrombosis and 89.1% of patients being beyond the Hangzhou criteria [10](with absence of macrovascular invasion, patient should fulfill one of the following criteria: a) tumor burden ≤8 cm regardless of AFP and differentiation or tumor burden>8 cm but AFP ≤ 100 ng/mL and well-moderate differentiation or b) tumor burden>8 cm but AFP between 100 and 400 ng/mL and well-moderate differentiation).Therefore, HCC recurrence was diagnosed in 21.8% of patients following LT in this study cohort.
The characteristics of HCC recurrence following LT are welldescribed.The location of tumor recurrences after LT varies but is mainly extrahepatic.The most frequent sites are the lungs, abdomen (adrenal gland, peritoneum or lymph nodes) and bones.For recurrent HCC, meaningful long-term survival can be achieved in a subset of patients, with many of these patients benefiting from combined surgical and nonsurgical treatments.The post-recurrent survival rate was much higher in patients who received surgerycentered comprehensive management compared to that of conservative treatments.Furthermore, surgical therapy was much more likely to be pursued among patients who developed late recurrence and had fewer numbers of recurrent nodules.Our findings support previous studies advocating for aggressive treatment of post-LT HCC recurrence.In research conducted by UCLA, Bodzin et al.analyzed 106 patients who developed post-LT HCC recurrence and found that patients with surgical therapy had a median survival of 27.8 months, which was significantly superior to those with nonsurgical therapy (10.6 months) and best supportive care(3.7 months) [6].In France, 14.2% of patients developed post-LT HCC recurrence after a median disease-free interval of 17 months.The median survival for resected patients after LT was 35 months compared to 15 months for unresected patients.Surgery was identified as an independent favorable factor for post-recurrence survival [5].The previous series of studies reported a median survival of approximately 15-34 months for transplant recipients receiving curative surgical or ablation therapy after recurrence [ 5 , 6 , 12-15 ].Taken together, pursuing aggressive therapy for post-LT HCC recurrence in well-selected patients should be considered the first choice in both Western and Eastern populations.
As recurrent HCC following LT is a systemic disease, tyrosine kinase inhibitors are usually prescribed in combination with other interventional therapies as a standard treatment for such patients [17-19].Iavarone et al.proposed a multicenter retrospective study describing the efficacy of regorafenib in patients with recurrent HCC after LT who progressed on sorafenib treatment.Median OS for regorafenib initiation was 12.9 months, while it was 38.4 months for sorafenib initiation, with the one- and three-year OS reaching 68% and 23%, respectively [20].However, the available data are quite limited as they are generally based solely on Western countries experi-ences and application of only sorafenib and regorafenib treatments.Lenvatinib has been approved as a first-line treatment for patients with unresectable HCC, as recently shown in the international randomized controlled phase III trial REFLECT [21].Our data showed that the OS in sorafenib-tolerant patients treated with lenvatinib was much higher than in those that discontinued sorafenib or switched to regorafenib due to unresponsiveness to sorafenib.In addition, in patients with recurrent HCC who received surgery followed by sorafenib-lenvatinib therapy and sirolimus-based immunosuppression, the two-year OS could reach 80%.Therefore, lenvatinib may be considered an option for the second-line treatment of recurrent HCC after LT as it can improve the OS of sorafenib-tolerant patients with progressive disease.
mTOR inhibitor-based immunosuppression may be a preferable option for liver transplant recipients with HCC [ 22 , 23 ].The SILVER trial suggested that the survival benefit of sirolimus was greater for low-risk patients compared to high-risk patients [24].Nonetheless, the effects of mTOR inhibitors on the outcomes of patients with recurrent HCC after LT have not been clarified.Our results demonstrated that sirolimus-based immunosuppression could improve the two-year OS after HCC recurrence compared with standard calcineurin inhibitor-based therapy.Invernizzi et al.[25]evaluated the safety and effectiveness of early sorafenib treatment with mTOR inhibitors in recurrent HCC after LT.Through implementation of early and combined treatment with sorafenib and mTOR inhibitors, objective response and stable disease were obtained in 16% and 50% patients, respectively.Therefore, conversion from tacrolimus to sirolimus-based immunosuppression may be a promising option in LT patients with recurrent HCC.
The limitations of this study include its retrospective design,limited size of the study population and relatively short follow-up period.This study should therefore be viewed as hypothesis generating and followed by larger prospective and multicenter studies to confirm our findings.
In summary, aggressive surgical intervention in well-selected patients with recurrent HCC after LT significantly improves the OS rate and should be pursued.Patients with unresectable recurrent HCC would benefit from a multidisciplinary treatment approach to slow down disease progression.
Acknowledgments
We would like to thank Chang Kai Wun and Bulat Abdrakhimov for correcting this article.
CRediT authorship contribution statement
Zhe Yang :Conceptualization, Investigation, Writing - original draft.Shuo Wang :Investigation, Writing - original draft.Xin-Yao Tian :Data curation, Formal analysis.Qin-Fen Xie :Data curation, Formal analysis.Li Zhuang :Formal analysis, Writing - review & editing.Qi-Yong Li :Data curation, Formal analysis.Cheng-Ze Chen :Data curation, Formal analysis.Shu-Sen Zheng :Conceptualization, Funding acquisition, Writing - review & editing.
Funding
This study was supported by the grants from National S&T Major Project (2017ZX10203205), the Medical Science and Technology Project of Zhejiang Province (2014KYA082), the Fundamental Research Funds for the Central Universities (2018FZA7002), and the Shulan Talent Foundation.
Ethical approval
This study was approved by the local ethics committee, and informed consents were obtained from all of the patients.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Recent evolution of living donor liver transplantation at Kyoto University: How to achieve a one-year overall survival rate of 99%?
- Endoscopic papillary large balloon dilation with or without sphincterotomy for large bile duct stones removal: Short-term and long-tem outcomes
- Optimizing biliary outcomes in living donor liver transplantation:Evolution towards standardization in a high-volume center
- Hepatic vein in living donor liver transplantation
- Hepatobiliary&Pancreatic Diseases International
- Hepatic artery reconstruction in pediatric liver transplantation:Experience from a single group