Infection within 2 weeks before liver transplantation closely related to prognosis of posttransplant infection: A single-center retrospective observational study in China
2020-09-21YueYingRuiDongLiJingWenAiYiMinZhuXinZhouYiYiQinXinChngChenXuYngWngHoChengZhngYngLiShnShnWengYiQiYuYiFengToYuXinHungZhengXinWngWenHongZhng
YueYingRui-DongLiJing-WenAiYi-MinZhuXinZhouYi-YiQinXin-ChngChenXu-YngWngHo-ChengZhngYngLiShn-ShnWengYi-QiYuYi-FengToYu-XinHungZheng-XinWngWen-HongZhng
a Department of Infectious Diseases, Huashan Hospital, Fudan University, Shanghai 20 0 040, China
b Department of General Surgery, Huashan Hospital, Fudan University, Shanghai 20 0 040, China
Keywords:
ABSTRACT
Introduction
Liver transplantation remains an effective procedure for multiple end-stage liver diseases.With the widespread use of potent immunosuppressive agents, the incidence of allograft rejection was reduced while opportunistic infections increased.Despite efficacious antimicrobial prophylaxis and vaccination to some pathogens, infections still represent the main factors influencing morbidity and mortality following liver transplantation [1-5].
In infections after liver transplantation, epidemiologic exposures included donor-derived infections and recipient-derived infections.Transplanted organs facilitate the transmission of infections from organ donors [1].Colonized or latent infections of recipients could be activated due to immunosuppression state after transplantation.However, the data about these were rare.
According to several previous reports, the spectrum of major infections occurring after transplantation has undergone a striking evolution [4 , 5].Knowledge of pathogen spectrum is very helpful for effective treatment.In this study, we surveyed infection rateand pathogen distribution after liver transplantation and analyzed the impact of donor or recipient factors on infection and survival.
Methods
General population
A total of 217 consecutive patients who underwent liver transplantation between April 2015 and October 2017 were enrolled.Seven patients died within 7 days after transplantation and were excluded from further analysis.Patient records were reviewed and follow-up information was obtained from referring physicians.Surveillance viral load testing for cytomegalovirus were performed every week for the first month after transplant.Bacterial cultures were ordered according to the clinical situation.The study was approved by the Ethics Committee of our hospital (No.2017-338).Written informed consent was obtained from all participants.
Surgery and immunosuppression
All patients underwent orthotopic liver transplantation either with primary anastomosis of the bile duct or choledochojejunostomy.Standard immunosuppression included tacrolimus (FK506),mycophenolate (MMF) and corticosteroids.FK506 was initially administered at a dosage of 3 mg every 12 h orally as soon as the patient was able to take oral medication, usually less than three days after surgery.FK506 was then adjusted according to blood levels.The target level for tacrolimus was 10-12 ng/mL during the first month after transplant, 8-10 ng/mL during the second and third month, and 5-10 ng/mL thereafter.Oral MMF was given at the dosage of 500 mg twice a day after 12 days of surgery.Methylprednisolone (240 mg) was administered intravenously on the day of surgery.This was reduced to 180 mg on the day after surgery and then rapidly tapered so that by day 6 the patient was receiving 40 mg of methylprednisolone.Oral medication with an equivalent dose of prednisone was given when the patient was able to take oral medicine.Basiliximab (20 mg) was given intravenously during surgery according to clinical situation.
Antimicrobial prophylaxis and treatment
Transplant recipients were treated with antibiotic prophylaxis immediately after transplantation.The antibiotic drug and course of treatment were based on donor situation and culture of preservation solution.Once recipients were diagnosed with infection,they received empirical antimicrobial treatment, then turning to etiological treatment after the results of culture and susceptibility were applicable.When viral load testing for cytomegalovirus was positive, intravenous ganciclovir 250 mg every 12 h was given until viral eradication was achieved, but not shorter than 2 weeks.
Definition of infections
We attempted to identify all infections which occurred after transplantation and categorize them according to time after transplantation, site of infection, type of pathogen, and outcomes.Strict criteria were employed to define infections as previously described [6 , 7].
Bloodstream infection was defined by the isolation in at least one blood culture ofListeriamonocytogenes,Staphylococcusaureus,Candidaspecies or aerobic gram-negative rods.For other pathogens, the isolation of the bacteria in two blood cultures or in one positive blood culture and in a culture from a known site of infection was required.
Abdominal infection was diagnosed if the peritoneal polymorphonuclear cells were>200/μL and if a pathogen was isolated.Incases where no cell counts were obtained, a Gram stain of peritoneal fluid showing ≥1 polymorphonuclear cell per oil field was sufficient.

Table 1Recipient characteristics.
Biliary tract infection was diagnosed if the patient had fever,right upper quadrant pain, and elevation of liver chemistry together with either evidence of cholangitis on liver biopsy or isolation of the same organism from both the T-tube drain and blood.
Pneumonia was diagnosed if chest X-ray showed new infiltrates with new onset of respiratory symptoms (cough, dyspnea) or hypoxemia, and the isolation of bacteria in heavy growth from purulent sputum.A diagnosis of cytomegalovirus pneumonia was based on the criteria of pneumonia plus fever ≥ 38 °C for at least 2 days within a 4-day period, the presence of neutropenia or thrombocytopenia, and the detection of cytomegalovirus DNA in blood [8].
Statistical analysis
All analyses were performed using SPSS, version 17.0 (SPSS Inc.,Chicago, IL, USA) and Graphpad Prism, version 6.02 (Graphpad Software, San Diego, CA, USA).Univariate and multivariate analyses were used to find the risk factors and prognostic factors for infection after transplantation.Continuous variables were expressed as median (range) and categorical data were expressed as number with percentage.We used Mann-WhitneyUtest or Chi-square test for the univariate analysis.We further conducted logistic regression for the multivariate analysis with factors proved to be significant.The Kaplan-Meier method was used to calculate the overall survival in the recipients who got infection after transplantation.APvalue<0.05 was defined as statistically significant.
Results
Spectrum of patient information and incidence of postoperative infection
Of all the 210 patients included, the most common underlying disease was viral hepatitis (139, 66.2%), followed by inherited liver diseases (24, 11.4%) and toxic-related liver disease (13, 6.2%).The median value of duration of hospitalization before transplant was 6 (range 0-78) days.Proportion of donation after circulation death was 87.6% (Table 1).In all, 98 patients were defined as postoperative infection, and the incidence of infection reached 46.7% (Fig.1).
In total, 196 episodes of infection occurred after transplantation during the median following of 214 days.Every patient experienced on average 0.93 episodes of infection.Timeline of post-transplant infection showed that most infection occurred in 1 month after transplantation (n= 153, 78.1%).The most frequent pathogen wasEnterobacteriaceaewith 41 episodes, includingKlebsiellapneumoniae,EnterobactercloacaeandSerratiamarcescens.The second most common isolated organism wasAcinetobacterbaumanii(27 cases), which only found in 1 month after transplantation.PseudomonasaeruginosaandStenotrophomonasmaltophiliawas isolated in 21 and 22 cases, respectively.Resistant organisms were also reviewed.AmongEnterobacteriaceae, extended spectrumβ-lactamase (ESBL) was founded in 26 strains (63.4%).Multidrug resistantAcinetobacterbaumaniiwas isolated in 22 strains(81.5%).The prevalence of multidrug resistantPseudomonasaeruginosawas 81.0% (17/21).As in multidrug resistantStenotrophomonas maltophilia, 36.4% (8/22).In Gram-positive bacteria, methicillinresistantStaphylococcusaureuswas observed in 40% (2/5), while in methicillin-resistant coagulase negativeStaphylococcuswas 84.6%(11/13).All theEnterococcuswas not found resistant to vancomycin.
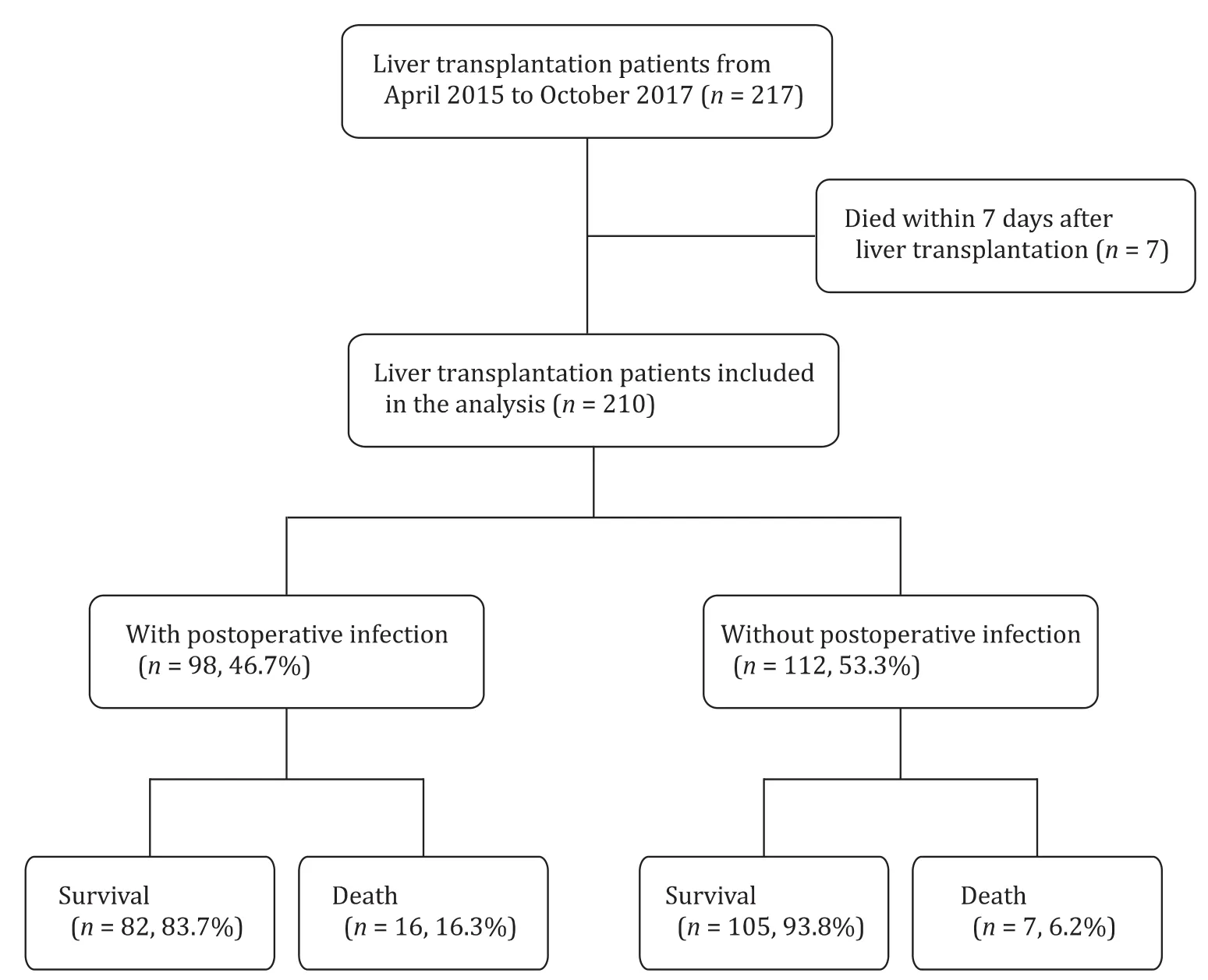
Fig.1.Flow chart of infections and survival after liver transplantation.
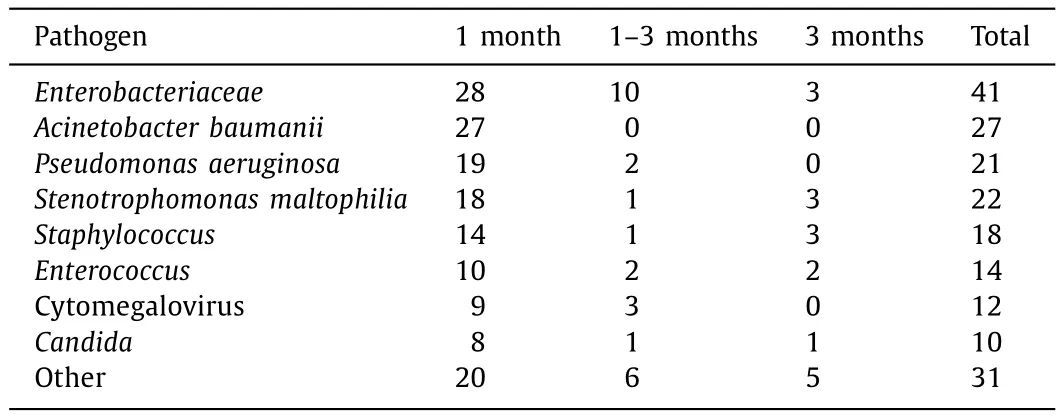
Table 2Common pathogens of different periods after liver transplantation.
Regarding viral infection, cytomegalovirus was the most common with 12 episodes.In total, 12 episodes of fungal infection were noted, and the most frequent pathogen wasCandida(10 cases), while 3 of them wereCandidaalbicans(Table 2).The other 2 fungal species wereaspergillusand unclassified fungus, respectively.
Sites of infection and microbial etiology
Respiratory tract was the most common site of infection (43.4%), followed by biliary tract (21.9%), abdomen (21.4%)and bloodstream (7.6%).Among the pathogen in pneumonia, the most frequently isolated wasAcinetobacterbaumanii(23.5%) andKlebsiellapneumoniae(21.2%).Pseudomonasaeruginosa,Stenotrophomonasmaltophilia, andKlebsiellapneumoniaeaccounted for 20.9%, 11.6% and 11.6% of pathogens in peritonitis, respectively.For biliary tract infection, the first rank wasStenotrophomonas maltophilia(14.0%), thenKlebsiellapneumoniae(11.6%), whilePseudomonasaeruginosaandEnterococcusfaecium(9.3%) were in the equal third place.Only 15 episodes of bloodstream infection occurred, andStaphylococcuswas the most common pathogen (40.0%,Fig.2).
Risk factors for infection after liver transplantation
The median hospital stay of patients with posttransplant infection was 40.5 days, which was longer than those without infection (28 days).In univariate analysis, we found that the infectionrelated preoperative and intraoperative factors were: age, model for end-stage liver disease (MELD) score, infection within 2 weeks before transplantation (especially pneumonia other than peritonitis), donor after circulation death, cold ischemic time (Table 3).The 11.2% of patients with infection after liver transplantation had pneumonia within 2 weeks before transplantation, while it was 2.7% of patients without infection after liver transplantation (P= 0.023).For postoperative factors, more prevalent biliary complication (14.3% vs.2.7%,P= 0.002) and longer duration of drainage tube (18 days vs.12 days,P<0.001) were found in patients with postoperative infection (Table 4).In multivariate analy-sis, the independent risk factors of infection after liver transplantation were MELD before transplantation (OR = 1.083, 95% CI: 1.045-1.123;P<0.001), biliary complication (OR = 4.725, 95% CI: 1.119-19.947;P= 0.035) and duration of drainage tube (OR = 1.040, 95%CI: 1.007-1.074;P= 0.017).
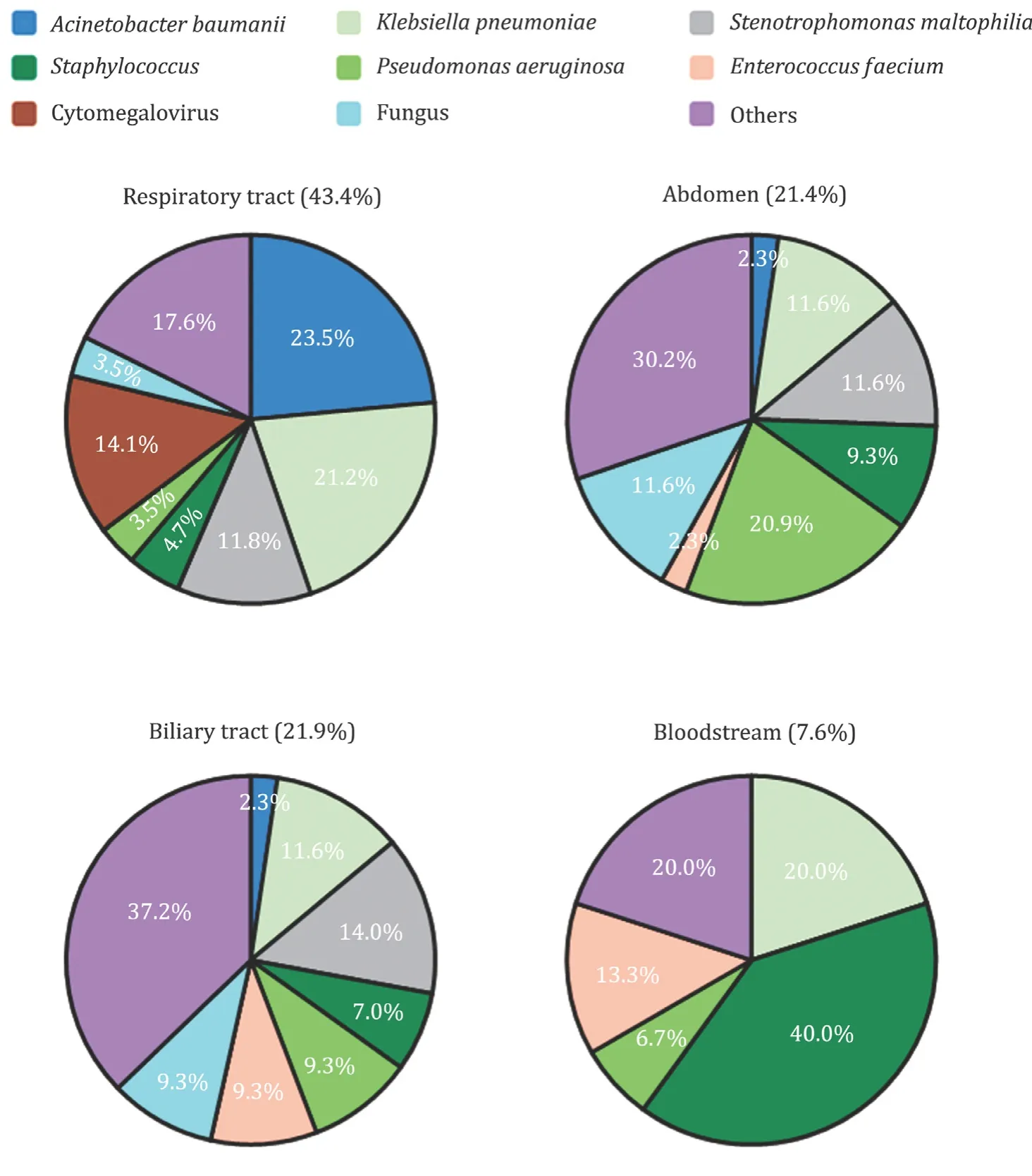
Fig.2.Frequency of different pathogens and sites of infections after liver transplantation.

Table 3Preoperative and intraoperative risk factors of infection after liver transplantation.
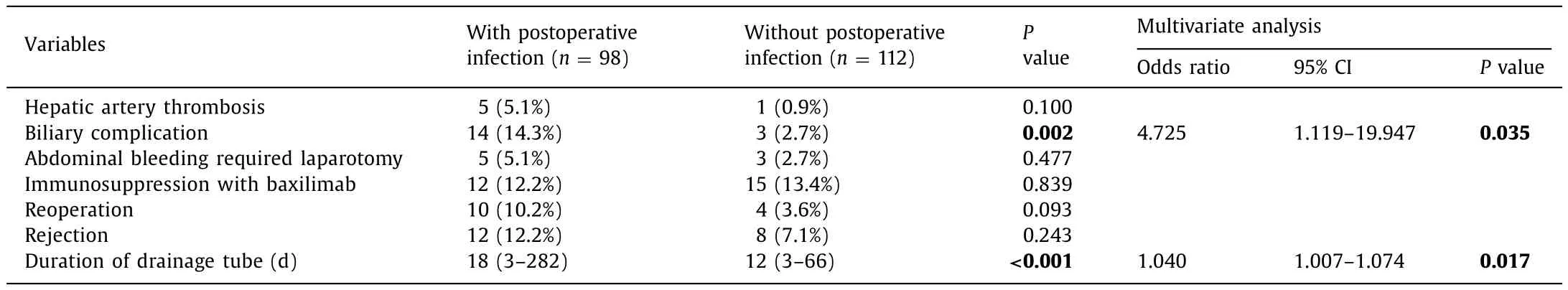
Table 4Postoperative risk factors of infection after liver transplantation.
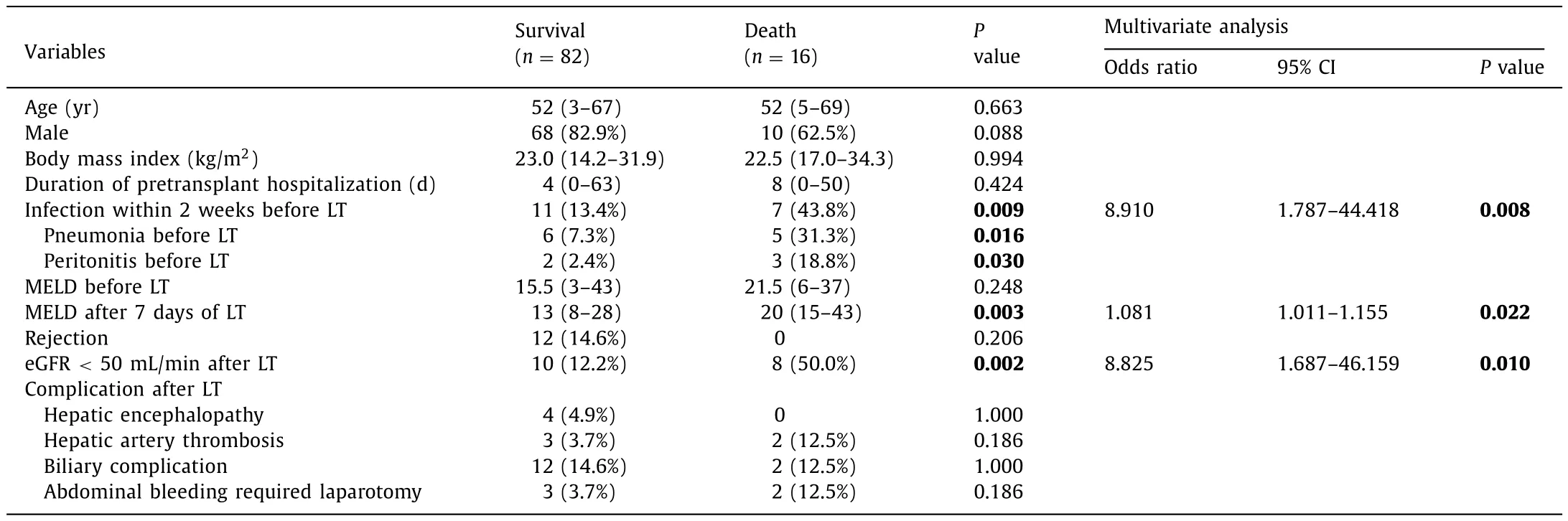
Table 5Risk factors of mortality in 98 patients with postoperative infection.
Recipient survival and prognostic factors for infection after liver transplantation
During the follow-up, all-cause mortality was 11.0% (23/210).The causes of death included three main categories: infection,poor graft function and others.42% was infection-associated death,while poor graft function accounted for 29%.In a total of 98 patients with infection after transplantation, 82 patients survived(Fig.1).In the univariate analysis, infection within 2 weeks before transplantation (especially pneumonia other than peritonitis), estimated glomerular filtration rate (eGFR)<50 mL/min after transplantation and MELD score after 7 days of transplantation were identified as prognostic factors (Table 5).Multivariate analysis revealed that independent prognostic factors were infection within 2 weeks before transplantation (OR = 8.910, 95% CI: 1.787-44.418;P= 0.008), MELD score after 7 days of transplantation (OR = 1.081,95% CI: 1.011-1.155;P= 0.022) and estimated glomerular filtration rate (eGFR)<50 mL/min after transplantation (OR = 8.825, 95% CI:1.687-46.159;P= 0.010).When recipients suffered from infection within 2 weeks before transplantation, although infection was controlled on the day of transplantation, they had a significantly lower 1- and 2-year survival compared to those not infected in Kaplan-Meier analysis (65.2% vs.90.0%; hazard ratio: 4.480;P<0.001;Fig.3).
Discussion
Among all the liver transplant recipients, infection is serious complication.The diagnosis of infection is commonly delayed because of the lack of signs and symptoms.Also, the spectrum of potential pathogens is broader and infection often progress more rapidly [1].It is very important to learn the risk and prognostic factors of infection after liver transplantation.In our study, MELD score are the major risk and prognostic factor regarding infection after transplantation, which is similar to other studies [9-11].MELD or PELD scores are used to evaluate the liver function of patients waiting to process liver transplantation, either in adult or pediatric [12 , 13].Patients with extreme poor liver function might have a lower level of immune defense against invasive microbial.We also found that MELD score after transplantation is associated with survival rate, like other studies reported [14 , 15].Patient failed to recover liver function after liver transplantation are more likely to have infections and die.
The incidence of infection after liver transplantation in our hospital reached 46.7%.It was consistent with the previous reports in China, in which 15% -69% of patients acquired postoperative infection [16-20].Most infection (78.1%) occurred in the first month after liver transplantation, which is related to surgical complications as for traditional view [3].However, the most common site of infection is not surgical site, but the respiratory tract and Gramnegative bacteria are major pathogens.Our findings were supported by other studies in China [17 , 18].These indicated that the pattern of posttransplant infection was changed and nosocomial infection might be the most important epidemiological exposure in the first month after transplantation.
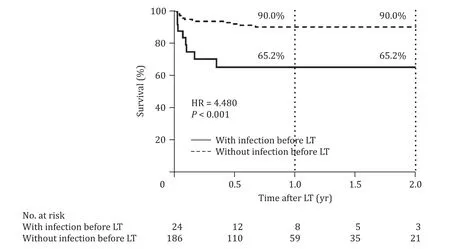
Fig.3.The survival rates of patients with posttransplant infection.Patients with pretransplant infection had a significantly lower 1- and 2-year survival compared to those without pretransplant infection.LT: liver transplantation.
The reason for most Chinese patients receiving liver transplantation is cirrhosis based on chronic hepatitis B [21].As we found in the study, viral hepatitis accounts for 66.2% of underlying disease.Spontaneous bacterial peritonitis is a common complication of cirrhosis.Meanwhile, pneumonia and biliary tract infection are also not rare in the case of cirrhosis.As a result, a large number of patients got infection before transplantation.
It is recommended that active infection in transplant candidates should be controlled before transplantation, since immunosuppression will exacerbate the infectious process [1].In this study, 24 patients (11.4%) had infections within 2 weeks before transplantation.Although their infections were all controlled on the day of transplantation, the recent infection history was a risk factor for infection after transplantation.Among all the infections, pneumonia within 2 weeks before transplantation seemed to be more related to infection after transplantation, although the pathogens were not the same.We assume that the pathogens were not eradicated thoroughly due to lack of treatment course, so they broke the innate barrier function of respiratory tract, thus leading to other pathogens more easily invade to cause infection in the immunosuppressed state after transplantation.Although we cannot prove that these infections are exactly recipient-derived, infections within 2 weeks before transplantation should be paid close attention.
This study had some limitations.First, this is a single-center study, and the results can be biased because of different pathogen distribution and higher antibiotic resistance rate than other medical institutions in China.Second, our study was retrospective, and the lack of some information, such as bile complication other than infection, might cause some biases in data analysis.
In conclusion, the prognostic factor for postoperative infection in liver transplant recipients was infection, especially pneumonia within 2 weeks before transplantation.
Acknowledgments
None.
CRediT authorship contribution statement
Yue Ying:Formal analysis, Investigation, Writing - original draft.Rui-Dong Li:Formal analysis, Writing - original draft.Jing-Wen Ai:Formal analysis, Methodology.Yi-Min Zhu:Data curation, Investigation, Methodology.Xian Zhou:Data curation, Investigation, Methodology.Yi-Yi Qian:Data curation, Investigation.Xin-Chang Chen:Data curation, Investigation.Xu-Yang Wang:Data curation, Investigation.Hao-Cheng Zhang:Data curation,Investigation.Yang Li:Data curation, Investigation.Shan-Shan Weng:Data curation, Investigation.Yi-Qi Yu:Data curation, Formal analysis, Investigation.Yi-Feng Tao:Resources.Yu-Xian Huang:Funding acquisition, Project administration, Writing - review &editing.Zheng-Xin Wang:Conceptualization, Resources, Supervision, Writing - review & editing.Wen-Hong Zhang:Supervision.
Ethical approval
The study was approved by the Ethics Committee of Huashan Hospital, Fudan University (No.2017-338).Written informed consent was obtained from all participants.
Funding
This study was supported by a grant from the National Natural Science Foundation of China (81670560).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Recent evolution of living donor liver transplantation at Kyoto University: How to achieve a one-year overall survival rate of 99%?
- Endoscopic papillary large balloon dilation with or without sphincterotomy for large bile duct stones removal: Short-term and long-tem outcomes
- Optimizing biliary outcomes in living donor liver transplantation:Evolution towards standardization in a high-volume center
- Hepatic vein in living donor liver transplantation
- Hepatobiliary&Pancreatic Diseases International
- Hepatic artery reconstruction in pediatric liver transplantation:Experience from a single group