Hangzhou criteria as downstaging criteria in hepatocellular carcinoma before liver transplantation: A multicenter study from China
2020-09-21QiFnZhnSunBinLingYiNnDngQioNnShnQinWiShngJunXuGungJingJingDiLuXuYongWiLiZhungWuZhngTinShnBiNiCnHiYngXiJiMinLiuJinWuShuSnZhngYngYngXioXu
Qi-Fn Zhn Sun-Bin Ling Yi-Nn Dng Qio-Nn Shn Qin-Wi Y Shng-Jun Xu Gung-Jing Jing Di Lu Xu-Yong Wi Li Zhung Wu Zhng Tin Shn Bi-Ni Cn Hi-Yng Xi Ji-Min Liu Jin Wu Shu-Sn Zhng Yng Yng c Xio Xu
a Department of Hepatobiliary and Pancreatic Surgery, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310 0 03, China
b NHC Key Laboratory of Combined Multi-organ Transplantation, Key Laboratory of the Diagnosis and Treatment of Organ Transplantation, CAMS, Hangzhou 310 0 03, China
c Department of Hepatic Surgery and Liver Transplantation Center, the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou 510630, China
d Department of Hepatobiliary and Pancreatic Surgery, Shulan (Hangzhou) Hospital, Hangzhou 310 0 0 0, China
e Department of Pathology and Molecular Medicine, Faculty of Health Sciences, McMaster University, Hamilton, Ontario L8S 4K1, Canada
Keywords:Hepatocellular carcinoma Liver transplantation Downstaging
ABSTRACT
Introduction
Hepatocellular carcinoma (HCC) is the sixth most commonly diagnosed cancer and the fourth leading cause of cancer death worldwide in 2018, with approximately 841 0 0 0 new cases and 782 0 0 0 deaths annually [1].Approximately half of HCC related deaths are in China [2].For patients with unresectable HCC, liver transplantation (LT) is the only radical treatment [3].In 1996, Mazzaferro et al.proposed that patients who met the Milan criteria(MC) had a better prognosis after LT [4].However, the MC is too restricted and only used the tumor size and number as the selection criteria for LT.According to the MC, many patients would be excluded from LT.Physicians tried to explore the extended cri-teria.There are currently several criteria, such as the University of California, San Francisco (UCSF) criteria [5], the “up-to-seven”criteria [6], and others [ 7 , 8 ].We proposed the Hangzhou criteria(HC) (total tumor diameter ≤ 8 cm or>8 cm with grade I or II tumors and an alpha-fetoprotein (AFP) level ≤400 ng/mL) to select HCC patients for LT [7].The HC has been further validated to achieve similar final clinical outcomes as the MC at different studies by multiple centers with large sample size [ 6 , 8-11 ].
For patients beyond the LT criteria, downstaging of HCC prior to LT is an efficacious strategy to expand patient selection, which has generated much interest in recent years [9].Downstaging of HCC is defined as reducing the tumor size prior to LT by locoregional therapy (LRT), including transarterial chemoembolization (TACE) or radiofrequency ablation (RFA) specifically to meet acceptable criteria for LT [10].Studies demonstrated that HCC patients beyond the LT criteria could be qualified for LT after successful downstaging [ 9 , 11-14 ].In most of these studies, the MC was used as the endpoint of downstaging.LT patients who achieved successful HCC downstaging to meet the MC had an overall survival (OS)and disease-free survival (DFS) similar to those who were initially within the MC [ 9 , 14 ].
In addition, as recommended in the US national conference [15], high AFP ≥10 0 0 ng/mL is also an exclusion criterion unless there is a substantial drop in the level to<500 ng/mL with LRT [14], which indicates that the change in serum AFP, a tumor biomarker, can also influence downstaging patients' eligibility for LT.In contrast, the HC combined different covariables of tumor grading and AFP, in addition to tumor size and number.Theoretically, the HC as the endpoint of LRT may allow more patients to gain an access to LT.
Recently, we published the clinical practice guidelines on LT for HCC in China (2018 edition) [16].The HCC patients exceeding the LT criteria who met the criteria after receiving downstaging treatment are recommended for LT [16].However, to date, no multicenter study from China's mainland has reported on the feasibility and advantage of using the MC or HC as downstaging criteria in Chinese population.Hence, in this study, we analyzed the data from three LT centers in China.Using the HC and MC as the endpoints of downstaging, we retrospectively analyzed the prognosis of the patients who underwent LRT before LT and eventually received LT.
Methods
Patients
Two hundred and seven LT patients were recruited from three transplantation centers in China [The First Affiliated Hospital of Zhejiang University School of Medicine, The Third Affiliated Hospital of Sun Yat-sen University, and Shulan (Hangzhou) Hospital]between January 2015 and July 2018.The patients' baseline data at the time of initial HCC diagnosis were collected from three centers; while the data after patients entered the waiting list were collected from the China Liver Transplant Registry (CLTR) database.This study was reviewed and approved by the ethical board in each center.
The diagnosis of HCC was based on the typical performance of at least two imaging examinations, including computed tomography (CT), magnetic resonance imaging (MRI) or angiography before LT and histology after LT.
LRT in pre-LT patients
For tumor downstaging, majority HCC patients received TACE as the LRT.Patients were admitted and hydrated prior to the TACE treatment.After receiving antibiotics, TACE was performed using oxaliplatin or lobaplatin mixed with lipiodol as the drug carrier.After administration of the emulsion, embolization using drugeluting beads containing epirubicin hydrochloride was performed.It is generally recommended to review the CT and/or MRI, tumorrelated markers, etc.three to six weeks after the first TACE treatment.The regular follow-up time was 1 to 3 months or longer and the frequency of the follow-up was based on post-TACE results.The survival of liver tumor was evaluated by the CT and/or MRI dynamic enhancement scan to determine whether TACE needed to be repeated.
Downstaging
In this study, we explored the impact of using the HC as the endpoint of downstaging on the prognosis of LT HCC patients.Patients who met the HC at the time of initial HCC diagnosis and received LRT as bridging treatment were analyzed as a control group.The entry criteria for tumor downstaging included patients beyond the HC on initial HCC diagnosis but with no evidence of extrahepatic metastasis or vascular invasion.There were no upper limits on tumor size and number.Successful downstaging was defined as a reduction in total tumor diameter ≤ 8 cm or>8 cm with grade I or II tumor differentiation but AFP level ≤400 ng/mL (Table 1).The size and number of tumor before receiving the first LRT was evaluated based on the imaging data (CT/MRI).The diameter and number of tumor after LRT were evaluated based on the enhanced CT/MRI measured the maximal diameter of the viable tumors and did not include the area of necrosis (mRECIST criteria) [ 17 , 18 ].Explants were assessed pathologically for tumor size, tumor number and degree of tumor differentiation.
Statistical analysis
The Chi-squared and/or Mann-WhitneyUtest were used to compare differences between subgroups.Logistic regression was used to evaluate the predictors of successful downstaging.The cumulative probabilities of HCC recurrence were estimated and compared using the competing risk method by Fine and Gray.OS was estimated using the Kaplan-Meier analysis.Data were expressed as median (range).APvalue<0.05 was considered statistically significant.The software used for analysis was the Statistical Package for Social Science (Version 20, SPSS Inc., Chicago, IL, USA).Competing risk analyses were performed using SAS software (Version 9.4,SAS Institute Inc., Cary, NC, USA).
Results
Baseline information
In total, 207 patients in three centers were enrolled initially.One patient had incomplete clinical information and was excluded because the total diameter of tumor>8 cm before first LRT but after LRT the lesion showed completely necrosis and could not evaluated the degree of differentiation which preclude the judgement whether the tumor met the HC (Fig.1).The remaining 206 patients were divided into two groups: 130 patients met the HC on initial HCC diagnosis, and 76 patients beyond the HC on initial.The baseline characteristics of the two groups of patients before LT are summarized in Table 2.The two groups were not significantly different in age, sex, the number of LRTs or the time from the first LRT to LT.Compared to those within the HC, a significantly higher percentage of patients beyond the HC received only TACE as the means of LRT (78.9% vs.65.4%,P= 0.04).In total, 198 (96.1%)patients had chronic hepatitis B, and the remaining 8 (3.9%) had hepatitis C (1), non-A, B, C hepatitis (1), alcoholic liver disease (2),congenital liver disease (1) and others (3).Most patients (n= 145,70.4%) received only TACE treatment, 16 (7.8%) received only RFA treatment, and 45 patients (21.8%) received combined LRT.
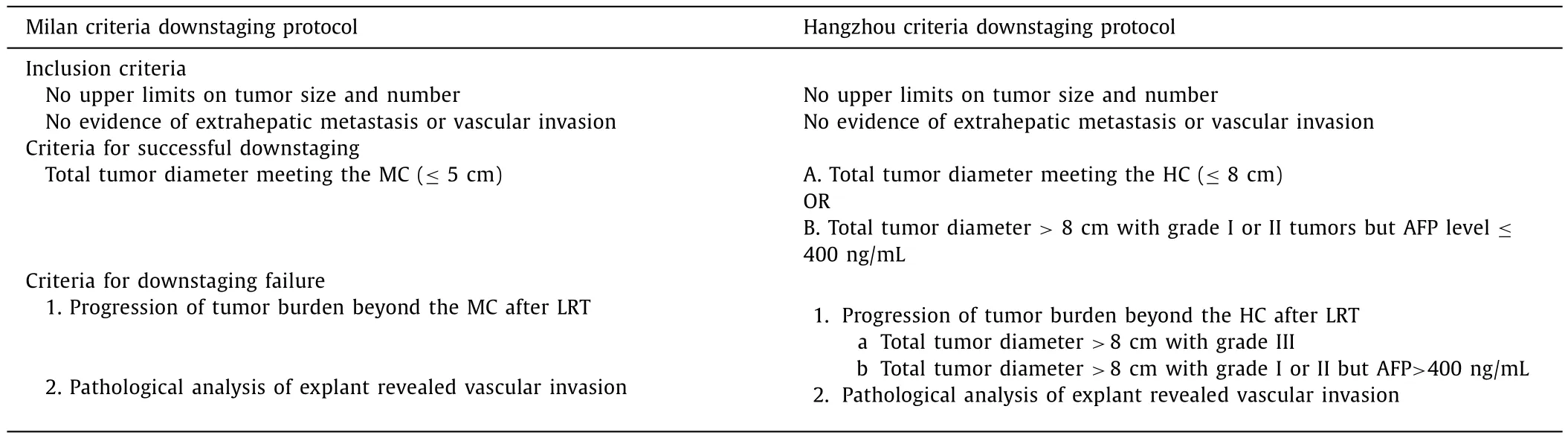
Table 1Successful and failure downstaging criteria.
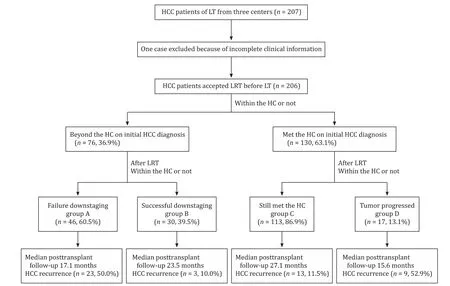
Fig.1.Maintenance and downstaging of the study population to the HC.LT: liver transplantation; HCC: hepatocellular carcinoma; LRT: locoregional therapy; HC: Hangzhou criteria.
Patients successful downstaging to the HC could achieve an ideal prognosis
In order to study the effect of the outcome of downstaging on the prognosis, we analyzed the 206 patients accepted LRT before LT.Of the 76 patients beyond the HC, 46 (60.5%) were still beyond the HC after LRT (group A), and 30 (39.5%) were successfully downstaged to HC after LRT (group B).In group B, 7 patients were downstaged to the MC.Of the 130 patients who initially met the HC, 113 (86.9%) remained within the HC after LRT (group C), and 17 (13.1%) progressed and exceeded the HC (group D) (Fig.1).
Next we analyzed the prognosis of the four subgroups to explore the effect of the HC as the endpoint of downstaging on the prognosis after LT.The median posttransplantation follow-up in group A was 17.1 months (range 0.5 to 51.7 months), and 23 of 46 patients (50.0%) developed HCC recurrence.For patients in group B, the median posttransplantation follow-up was 23.5 months (range 0.8 to 64.4 months) (P= 0.048 to group A), and 3 of 30 patients (10.0%) developed HCC recurrence.In group C,the median posttransplantation follow-up was 27.1 months (range 0.2 to 57.9 months,P= 0.68 compared to group B,P<0.01 to group A), during which 13 of 113 patients (11.5%) developed HCC recurrence.The median posttransplantation follow-up in group D was 15.6 months (range 0.1 to 54.2 months,P= 0.025 compared to group C;P= 0.092 to group B;P= 0.85 to group A),and 9 of 17 (52.9%) patients developed HCC recurrence (Fig.1).The other clinical data of the four groups are summarized in Table 3 , the four groups were not significantly different in age, sex and the Child-Pugh classification.

Table 2Baseline characteristics of the 206 patients before the first LRT (grouping based on whether meeting HC).
Based on competing risk analysis, the 3-year HCC recurrence probabilities in groups A, B, C and D were 52.3%, 10.3%, 11.6% and 59.4% (group B vs.group C,P= 0.87).The Kaplan-Meier 3-year post-LT survival probabilities in groups A, B, C and D were 41.2%,70.7%, 73.5% and 26.5% (group B vs.group C,P= 0.66) (Fig.2).
Patients downstaging to the HC but not meeting the MC had equal outcome to MC
Furthermore, in group B, 23 patients remained beyond the MC after LRT, and we also analyzed the difference in OS and HCC recurrence probabilities of these 23 patients (downstaging to HC-MC group) with those within the MC in group C (within MC group,n= 90).Using competing risk analysis, the cumulative probabilities of HCC recurrence at 3 years in the two groups were 12.4% and 9.1% (P= 0.61).The Kaplan-Meier 3-year post-LT survival probabilities in the two groups were not statistically significant (P= 0.39,Fig.3).Notably, in these 23 patients, the total tumor diameter of 13 patients was still>8 cm after LRT, but their serum AFP dropped to a level of<400 ng/mL and with grade I or II tumors.These results showed that for those failing downstaging to the MC, if their tumor could meet the HC after LRT, they could also achieve a good outcome.Hence, the HC could also serve as a favorable downstaging criteria in these patients and here we defined it as Hangzhou downstaging criteria (Hangzhou-DS criteria).
Besides, we also divided these 206 patients based on the MC,and the baseline characteristics of the groups are summarized in Table 4.The situation of tumor response to the MC as the endpoint of downstaging was summarized in Fig.4 , the rate of successful downstaging to the MC was 20.3% (25/123).And we also analyzed the prognosis using the MC as the endpoint of downstaging.The OS and the cumulative probabilities of HCC recurrence in those successfully downstaged to the MC were not significantly different from those within the MC initially (Fig.5).
Patients with highly/medium differentiated HCC are more likely to be successful downstaged
Based on the above data, we proved that the outcome of downstaging could significantly affect the prognosis of LT HCC patients.Hence, next we explored the predictors of downstaging to the HC.We used logistic regression to analyze the characteristics of the patients beyond the HC initially (n= 76).In the univariate logistic regression analysis, age>50 years and highly/medium differentiated HCC were the statistically significant predictors for successful downstaging into the HC.In the multivariable logistic analysis, age>50 years (OR = 3.13; 95% CI: 1.01-9.16;P= 0.04) and highly/medium differentiated HCC (OR = 8.36; 95% CI: 2.60-26.84;P<0.01) were the statistically significant predictors for successful downstaging (Table 5).
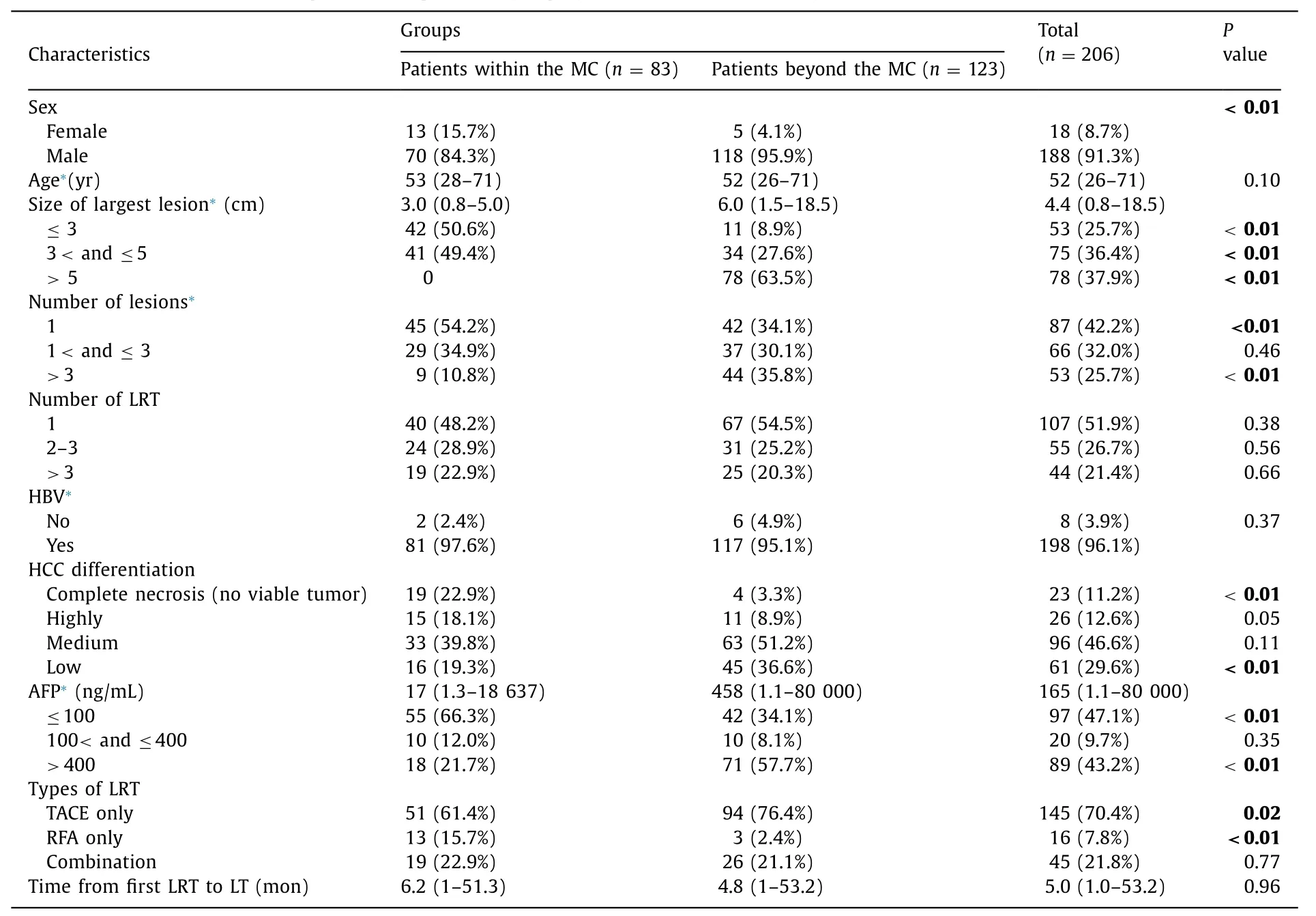
Table 4Baseline characteristics of the 206 patients accepted LRT (grouping based on whether meeting the MC).
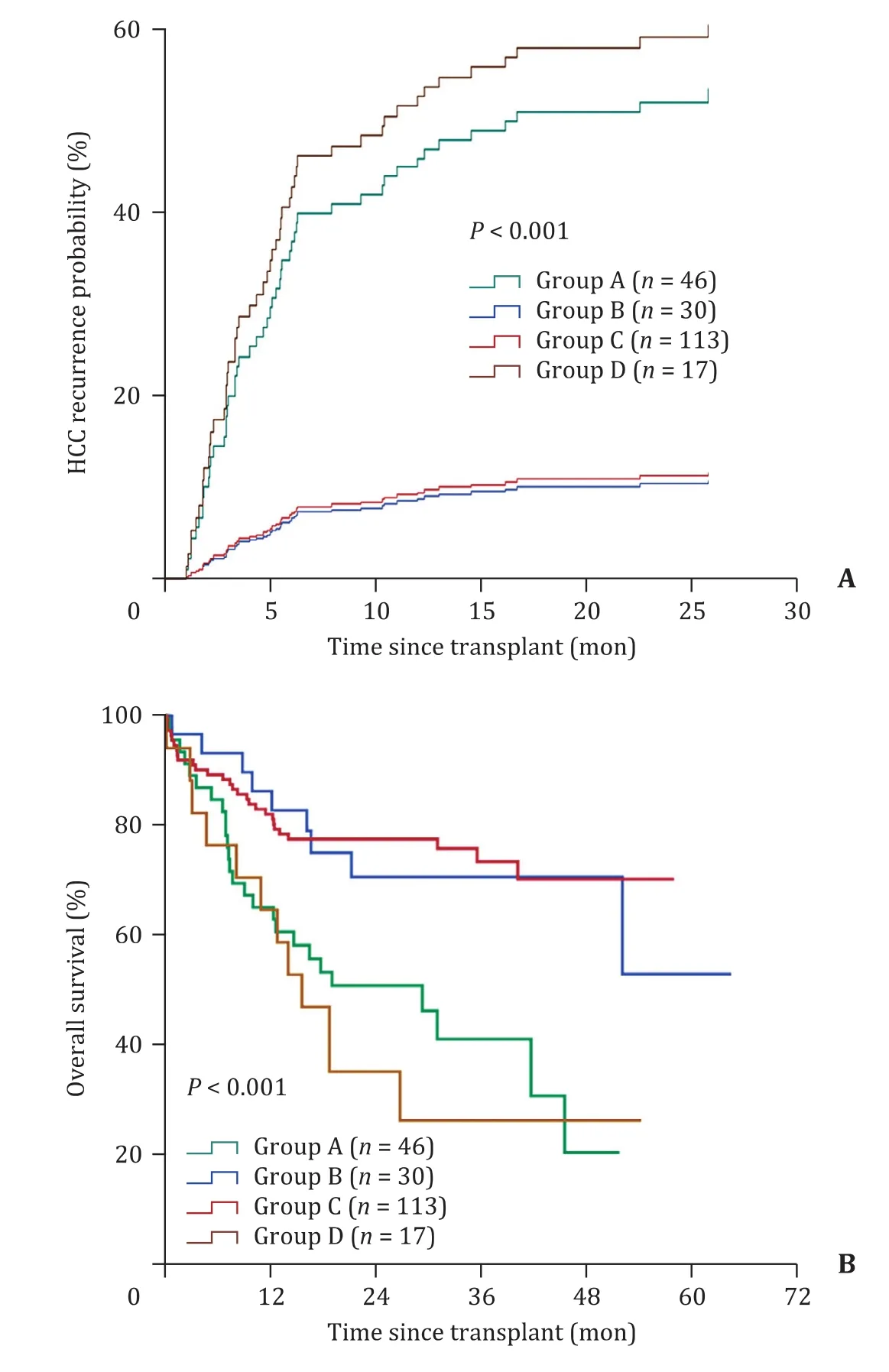
Fig.2.Competing risk analysis of the probabilities of HCC recurrence and Kaplan-Meier post-transplantation OS of groups A, B, C and D.Time zero represents the date of liver transplantation in all groups.A: The probabilities of HCC recurrence of groups A, B, C and D, the difference was not statistically significant between groups B and C (P = 0.87) but was statistically significant between groups A and B (P = 0.002); B: The OS of groups A, B, C and D, the difference in OS was not statistically significant between groups B and C (P = 0.66) but was statistically significant between groups A and B (P = 0.01).HCC: hepatocellular carcinoma; OS:overall survival.
Discussion
In 1997, Majno and colleagues first reported that the response of tumors to TACE was associated with improved disease-free survival after both liver resection and transplantation [19].Recently, a number of studies have further identified the effect of LRT in the downstaging of preLT, and all these studies used the MC as the endpoint for downstaging [ 9 , 12 , 13 , 20-23 ].These studies supported the notion that downstaging selected a subset of patients who could achieve posttransplantation survival similar to those meeting the LT criteria without downstaging [14].
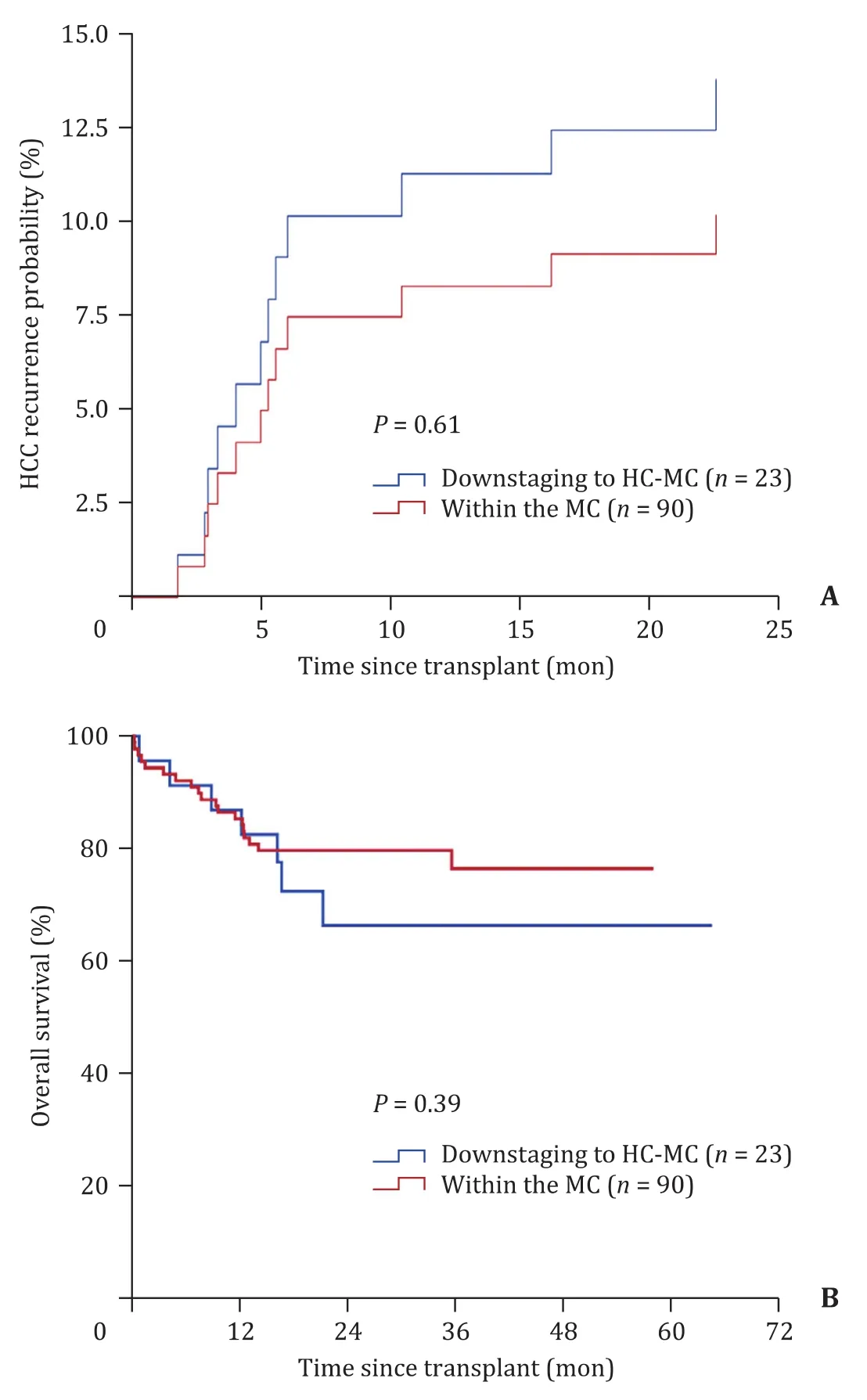
Fig.3.Competing risk analysis of the probabilities of HCC recurrence and Kaplan-Meier post-transplantation OS of the downstaging to HC-MC group and within MC group.Time zero represents the date of liver transplantation in all patients.A: The probabilities of HCC recurrence of the downstaging to HC-MC group and within MC group; B: The OS of the downstaging to HC-MC group and within MC group.HCC:hepatocellular carcinoma; OS: overall survival; MC: Milan criteria; HC: Hangzhou criteria.
In China, for some reason, finally more than 30% HCC recipients exceeded the HC [7].In the present study, the retrospective analysis showed that only 9.2% (7/76) recipients exceeding the HC were successfully downstaged to the MC, while 39.5% (30/76) to the HC.Patients exceeding the HC are much harder to be downstaged to the MC than to the HC.Significantly, recipients successfully downstaged to the HC could achieve an ideal prognosis as recipients within the HC or MC.Thus, the MC, as the endpoint of downstaging, is comparatively restrictive, while the HC, on the other hand, appears to be more appropriate as the downstaging criteria in China, defined as Hangzhou-DS criteria.
The main difference between the HC and MC is that the HC introduce the covariables of tumor grading and AFP in addition to tumor size and number, which are of known prognostic relevance.Significantly, for patients with a total tumor diameter greater than 8 cm, an AFP over 400 ng/mL, and highly/medium tumor differentiation, as long as their AFP levels dropped below 400 ng/mL, and even if the tumor diameter did not significantly decrease, it could still be considered successful downstaging.Given the excessive tumor size has become one of the factors limiting the success rate of downstaging [24], the HC combining AFP and HCC differentiation with tumor burden may be a more ideal downstaging end-point.Theoretically, the advantage of the HC as the end point of the downstaging treatment is that it may give more LT opportunities to HCC patients who have poor initial tumor biological features.

Table 5Univariate and multivariate analysis of predictor for successful downstaging to HC.
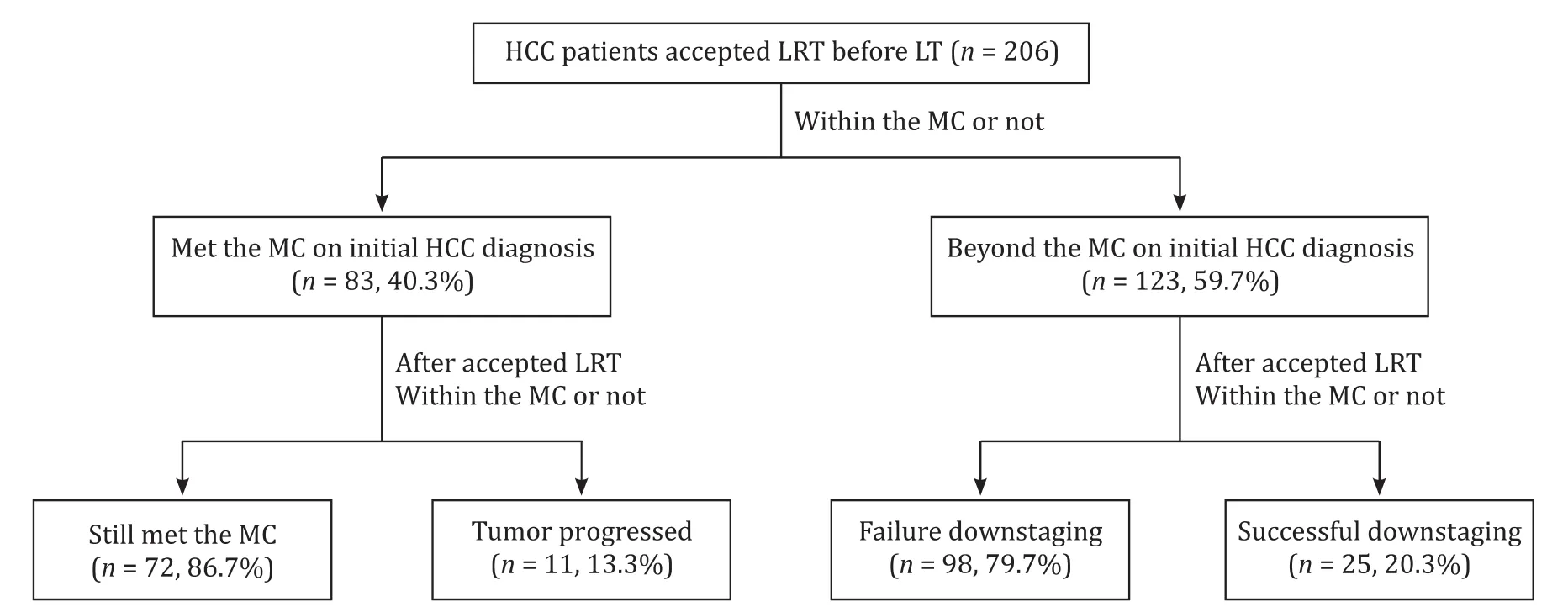
Fig.4.Maintenance and downstaging of the study population to the MC.LT: liver transplantation; HCC: hepatocellular carcinoma; LRT: locoregional therapy; MC: Milan criteria.
The present study showed that the prognosis of patients who successfully downstaged to the HC after receiving LRT was similar to that of patients who met the HC before and after LRT.More importantly, using the HC as the endpoint of downstaging treatment allowed the selection of patients who would benefit from LT despite their stage still being beyond the MC after the downstaging treatment.Interestingly, of the 23 patients who were successfully downstaged to the HC but were still beyond the MC after LRT, the HCC recurrence probabilities and OS were not significantly different from those of the patients within the MC.These 23 patients, according to the MC, were not recommended for LT even though they had accepted LRT and their tumor biology had changed.Therefore, our study proved that the HC could be used as the endpoint of LRT to screen out those patients who exceed the traditional MC but can still benefit from LT.That means, at least,for patients exceeding the HC, downstaging to HC are good candidates for LT.
In the multivariate logistic regression analysis, older age,highly/medium degree of tumor differentiation were significant predictive factors of successful downstaging.According to the definition of the HC, for patients with a total tumor diameter greater than 8 cm and a low degree of tumor differentiation, the only way they can accept successful downstaging is dropping the tumor diameter to 8 cm; therefore, these patients are more difficult to be downstaged than those with high tumor differentiation.The elderly HCC patients have been reported to have better histological differentiation, earlier TNM staging and relatively lower tumor metastasis rate [ 25-27 ], indicating that the tumor of elderly patients may have a better biological behavior and thus better response to TACE and other treatments.
Some limitation of this study should be addressed.Firstly,though this was a multicenter study, the patients were only from two cities in China.Second limitation is the CLTR database.We only recruited those patients received LT in this study hence there was a bias and we did not study those patients who "dropped-off"from list.Besides, given the HCC differentiation was determined by explant pathology, it is hard to determine the accurate pathological type before LT.Thus, for patients with HCC over 8 cm and AFP≤400 ng/mL, whether they are fulfilling HC are uncertain.It may require further development of puncture technology or imaging to promote the Hangzhou-DS criteria towards clinical applications.
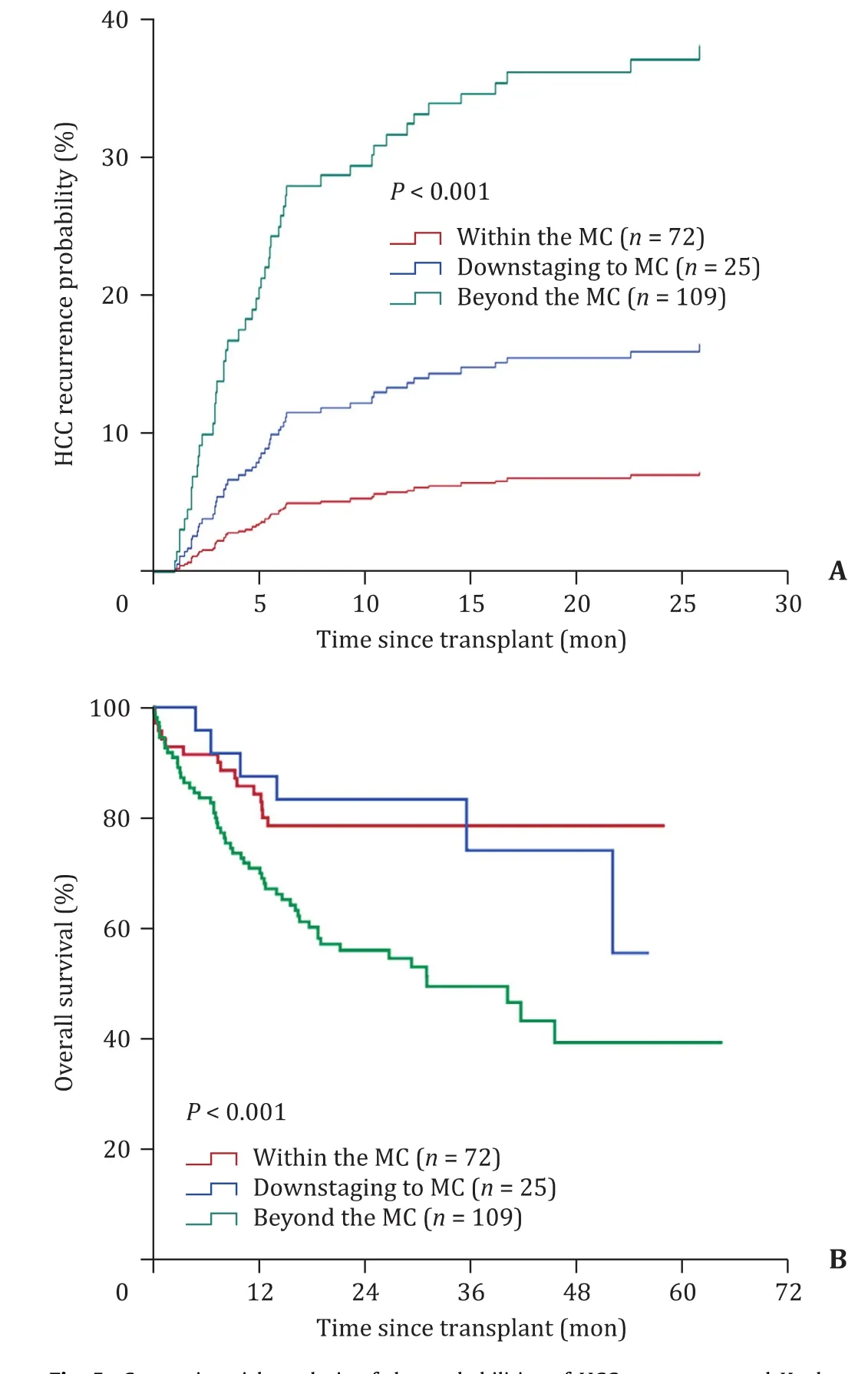
Fig.5.Competing risk analysis of the probabilities of HCC recurrence and Kaplan-Meier post-transplantation OS of the downstaging to MC group, within MC group and beyond MC group.Time zero represents the date of liver transplantation in all groups.A: The probabilities of HCC recurrence of the three groups, the difference was not statistically significant between the downstaging to MC group and within MC group (P = 0.24), but was statistically significant between the beyond MC group and downstaging to MC group (P = 0.035); B: The OS of the three groups was not statistically significant different between the downstaging to MC group and within MC group (P = 0.92), but was statistically significant between the beyond MC group and downstaging to MC group (P = 0.023).OS: overall survival; MC: Milan criteria;HC: Hangzhou criteria.
In conclusion, we report a large, long-term and multicenter clinical study that analyzed the outcomes of different subgroups of HCC patients for LT when using the HC as the endpoint of downstaging.Our study showed that the HC, as the end point of LRT, can give more patients access to LT, serve as a favorable selection criterion, and provide an ideal prognosis.In the traditional MC, these patients are not recommended for LT, even if the biological behavior of the tumor changes after LRT.This information will be helpful in selecting more LT candidates with low recurrence potential in the context of HCC downstaging.As the MC based downstaging criteria has been officially accepted as United Network for Organ Sharing down-staging (UNOS-DS) inclusion criteria in United States [9], we plan to initiate a larger multicenter clinical study to support Hangzhou-DS criteria and propose a standardized downstaging protocol which is based on Hangzhou-DS criteria in China.
Acknowledgments
None.
CRediT authorship contribution statement
Qi-Fan Zhan:Conceptualization, Data curation, Writing - original draft, Writing - review & editing.Sun-Bin Ling:Conceptualization, Data curation, Funding acquisition, Writing - original draft,Writing - review & editing.Yi-Nan Deng:Conceptualization, Data curation.Qiao-Nan Shan:Data curation.Qian-Wei Ye:Data curation.Sheng-Jun Xu:Data curation.Guang-Jiang Jiang:Data curation.Di Lu:Data curation.Xu-Yong Wei:Data curation.Li Zhuang:Data curation.Wu Zhang:Data curation.Tian Shen:Data curation.Bei-Ni Cen:Software.Hai-Yang Xie:Software.Ji-Min Liu:Writing- review & editing.Jian Wu:Data curation.Shu-Sen Zheng:Conceptualization.Yang Yang:Conceptualization.Xiao Xu:Conceptualization, Funding acquisition, Writing - review & editing.
Funding
This work was supported in part by grants from the National Science and Technology Major Project of China (No.2017ZX10203205), the National Natural Science Founds for Distinguished Young Scholar of China (No.81625003), the State Key Program of National Natural Science Foundation of China (No.81930016), and the National Natural Science Foundation of China(No.81902407).
Ethical approval
This study was approved and reviewed by the ethical board in each center.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Recent evolution of living donor liver transplantation at Kyoto University: How to achieve a one-year overall survival rate of 99%?
- Endoscopic papillary large balloon dilation with or without sphincterotomy for large bile duct stones removal: Short-term and long-tem outcomes
- Optimizing biliary outcomes in living donor liver transplantation:Evolution towards standardization in a high-volume center
- Hepatic vein in living donor liver transplantation
- Hepatobiliary&Pancreatic Diseases International
- Hepatic artery reconstruction in pediatric liver transplantation:Experience from a single group