呼气试验对胃排空延迟诊断价值的meta分析
2020-07-04白颖高维丛佳琳程淑莉赵兴杰张力杨晓晖
白颖 高维 丛佳琳 程淑莉 赵兴杰 张力 杨晓晖
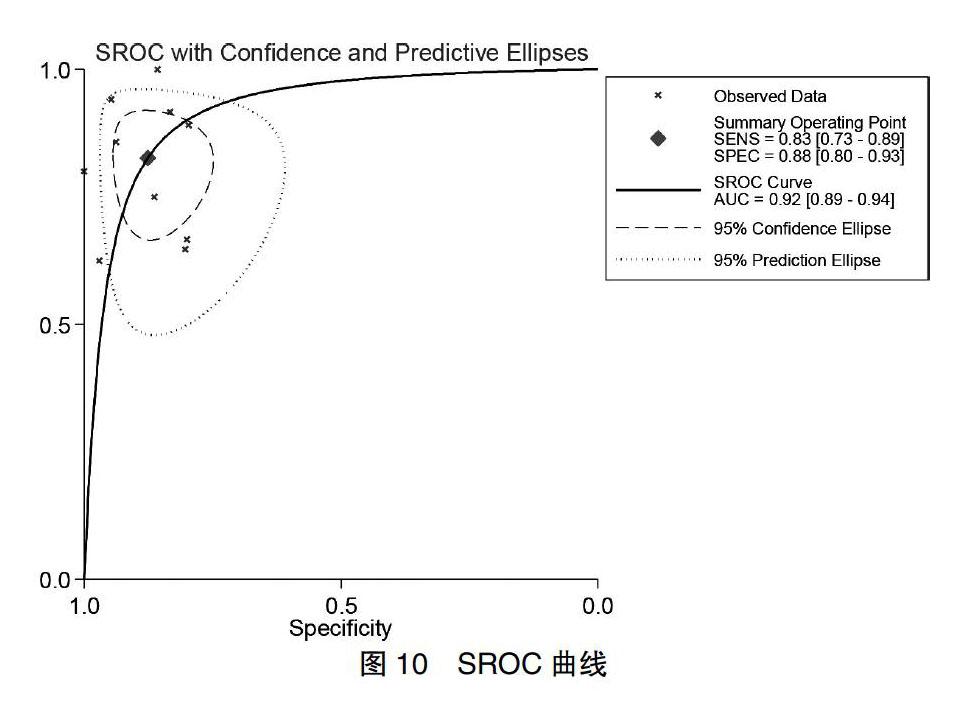

[摘要] 目的 評估呼气试验对胃排空延迟的诊断价值。 方法 检索PubMed、the Cochrane library、中国知网、万方、维普、中国生物医学文献等数据库,搜集国内外关于呼气试验诊断胃排空延迟的诊断性试验,检索时间均为建库至2018年4月。采用固定效应模型进行荟萃分析,研究指标包括敏感度、特异度、阳性似然比、阴性似然比、诊断比值比以及曲线下面积(AUC)。 结果 共纳入10项研究涉及434名研究对象。呼气试验对延迟胃排空的鉴别诊断敏感度为0.826(95%CI:0.728~0.894),特异度为0.876(95%CI:0.800~0.925),AUC为0.92。阳性似然比为6.640(95%CI:3.987~11.060),阴性似然比为0.198(95%CI:0.122~0.321)。 结论 呼气试验在胃排空延迟中有较高诊断价值,期待在临床进一步推广应用。
[关键词] 呼气试验;胃排空延迟;诊断价值;诊断性试验;meta分析
[中图分类号] R619 [文献标识码] A [文章编号] 1673-7210(2020)05(b)-0125-06
Diagnostic accuracy of breath test in detection of delayed gastric emptying: a meta-analysis
BAI Ying1 GAO Wei2 CONG Jialin2 CHENG Shuli2 ZHAO Xingjie3 ZHANG Li4 YANG Xiaohui5,6
1.College of Traditional Chinese Medicine, Beijing University of Chinese Medicine, Beijing 100029, China; 2.the Second Clinical Medical College, Beijing University of Chinese Medicine, Beijing 100078, China; 3.Department of Gastroenterology, Dongfang Hospital Affiliated to Beijing University of Chinese Medicine, Beijing 100078, China; 4.Department of Endocrinology, Dongfang Hospital Affiliated to Beijing University of Chinese Medicine, Beijing 100078, China; 5.Department of Endocrinology, Dongzhimeng Hospital Affiliated to Beijing University of Chinese Medicine, Beijing 100700, China; 6.Traditional Chinese Medicine Master LYU Heren Work Station at Dongfang Hospital Affilated to Beijing University of Chinese Medicine, Beijing 100078, China
[Abstract] Objective To evaluate the diagnostic value of breath test for delayed gastric emptying. Methods Database include PubMed, the Cochrane Library, China National Knowledge Internet, WanFang Data, VIP, CBM were searched to collect exsiting diagnostic accuracy tests on delayed gastric emptying diagnosed, the retrieval time was from database construction to April 2018. The fixed effect model was used for meta-analysis, and the research indicators included sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, diagnostic odds ratio and the area under the curve (AUC). Results Ten studies with 434 objects were included. The sensitivity of breath test for diagnosis of delayed gastric emptying was 0.826 (95%CI: 0.728 to 0.894), and the specificity was 0.876 (95%CI: 0.800 to 0.925). The AUC was 0.92. The combined positive likelihood ratio was 6.640 (95%CI: 3.987 to 11.060), and the negative likelihood ratio was 0.198 (95%CI: 0.122 to 0.321). Conclusion Breath test is a useful tool for detecting delayed gastric emptying with a relatively high sensitivity and specificity. It is expected to be applied in clinic.
[Key words] Breath test; Delayed gastric emptying; Diagnostic value; Diagnostic test; Meta-analysis
胃排空延迟主要表现为早饱、食欲下降、腹胀、恶心、呕吐等症状[1-2],严重者甚至贫血、体重下降,严重影响患者的生活质量。除消化系统疾病外,糖尿病[3-4]、帕金森病[5]及一些手術[6-7]也可导致胃排空延迟。胃排空延迟的准确判定对临床上评价病情、决定治疗方案有重要指导意义。目前认为放射性核素扫描法是诊断胃排空延迟的金标准[8-9]。但该方法不足之处在于:检查时间过长,患者依从性低、可重复性较差[10];儿童、孕妇等特殊人群不适合放射性核素检查;核素扫描仪器昂贵,难以普及[11];世界各地缺乏统一的实施和评判标准,不同医疗中心在开展检测前须根据健康人群确定正常值范围。
1993年,Ghoos等[12]首先报道了应用13C辛酸呼气试验诊断胃排空延迟的方法,至今在诊断消化系统疾病中已运用数十年[13-14]。通过口服与食物结合的同位素13C,检测不同时段13C含量,就可间接反映胃肠道动力情况[15-16]。与核素扫描法比较,呼气试验简单、经济、可重复性高[17],有望成为诊断胃排空延迟的理想替代方法[18-19]。本研究对目前已报道的诊断性试验进行综合评价,为呼气试验诊断胃排空延迟提供更多的证据支持。
1 资料与方法
1.1 纳入与排除标准
1.1.1 研究类型 公开发表的关于呼气试验诊断胃排空延迟的诊断性试验研究。语种为中文或英文。
1.1.2 研究对象 病例组为为胃排空时间延迟的人群,对照组为健康人群。
1.1.3 诊断方法 待评价试验为呼气试验,以胃排空核素扫描法作为胃排空延迟诊断的金标准。
1.1.4 结局指标 敏感度(Sen)、特异度(Spe)、阳性似然比(+LR)、阴性似然比(-LR)、诊断比值比(DOR)以及SROC曲线下面积(AUC)。
1.1.5 排除标准 ①毕业论文;②无对照组或以非健康人群为对照组;③关键数据不全;④重复发表;⑤病例组诊断标准不明确。
1.2 文献检索策略
检索PubMed、the Cochrane library、CNKI、WanFang Data、VIP、CBM等数据库,搜集国内外关于呼气试验诊断胃排空延迟的诊断性试验,检索时间均为建库起至2018年4月。检索词为“呼气试验”“胃排空”“breath test”“gastric emptying”,采用主题词与自由词结合的方式进行检索,检索策略以PubMed为例列举如下。见图1。
1.3 资料提取
由两名评价员进行文献筛选和数据提取,相互核对结果,遇到分歧时由第三方决定或者小组内讨论决定。资料提取内容包括:①基本信息:题目、作者、发表时间、原始出处、诊断标准、试餐性质等;②基线特征:研究的样本量、病例组基本信息、对照组基本信息;③四格表数据:即真阳性(TP)、假阳性(FP)、真阴性(TN)、假阴性(FN);④灵敏度(%)=TP/(TP+FN)、特异度(%)=TN/(FP+TN)。
1.4 文献质量评价
由两名研究员进行文献质量评价,如有异议则第三方决定或者小组内讨论裁定。纳入研究的方法学质量评价选择QUADAS-2工具,各条目的评价标准包括“是”“否”“不清楚”3种,“是”为满足此标准;“否”为不满足此标准;“不清楚”为部分满足该标准或者从文献中不能得到充足的信息。如果QUADAS-2评分≥10分,则认为文献质量较高。
1.5 统计学方法
使用STATA 12.0软件进行meta分析。根据ROC曲线和Spearman相关系数判断是否存在阈值效应,如果存在阈值效应,则绘制拟合SROC曲线并计算AUC。采用Cochrane-Q检验判断是否存在非阈值效应所致异质性,从而决定采用固定效应模型还是随机效应模型。提取数据后计算所纳入研究的合并Sen、Spe、+LR、-LR、DOR等指标,绘制SROC曲线并计算AUC。以P < 0.05为差异有统计学意义。应用Deek′s漏斗图评估发表偏倚。
2 结果
2.1 文献检索结果
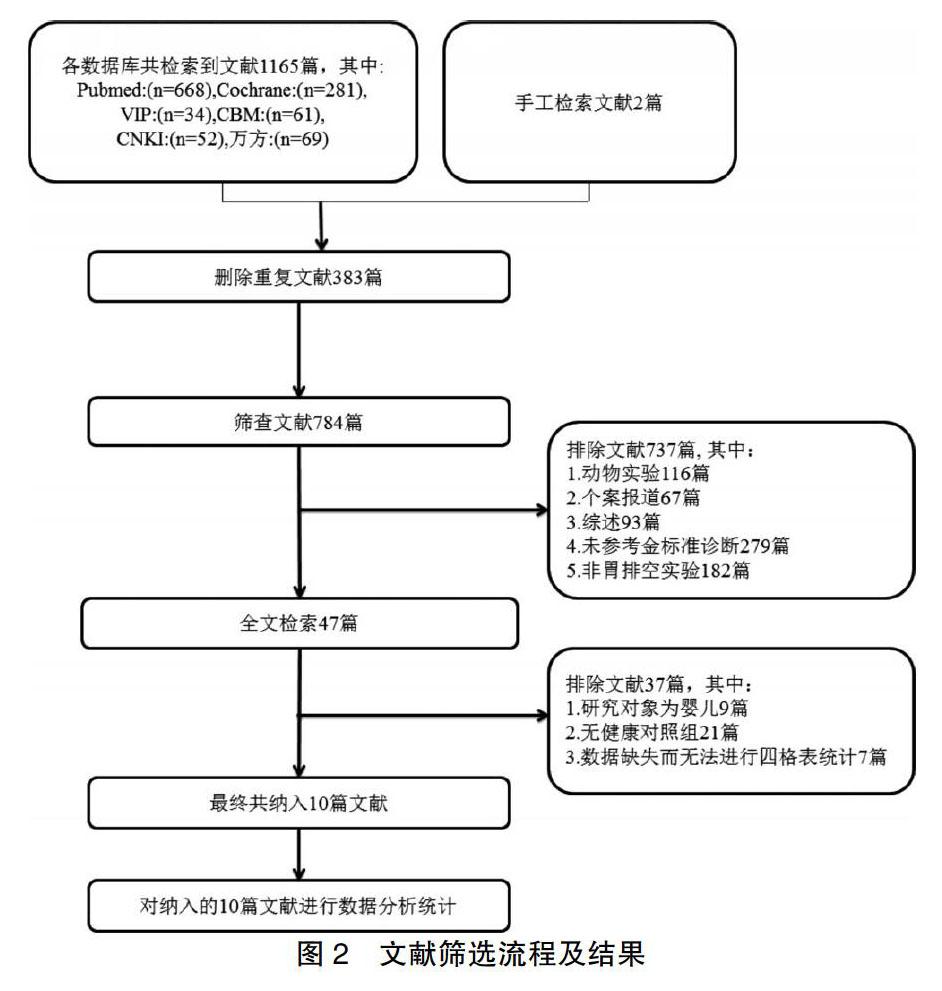
初检共获得相关文献1165篇,其中PubMed检索得到668篇,Cochrane library 281篇,CNKI 52篇,WanFang Data 69篇,VIP 34篇,CBM 61篇,通过其他途径补充得到文献2篇,通过阅读题目与摘要、排除重复研究后,最终纳入10篇研究[12,21-29]。见图2。
2.2 纳入研究基本特征及质量评价
共纳入来自8个国家的10篇研究[12,21-29],其中2篇[25-26]来自美州,2篇[23-24]来自亚洲,1篇[25]来自澳洲,5篇[12,26-29]来自欧洲。所有文献均以核素闪烁扫描法作为诊断胃排空延迟的金标准。10篇文献[12,21-29]共纳入胃排空延迟患者149例,健康对照者285名,具体信息、纳入研究质量评价见表1,图3。
2.3 异质性检验
进行异质性检验,ROC曲线图不呈“肩臂状”分布,Spearman相关系数为0.025(P = 0.05),提示不存在阈值效应。异质性检验所得Q = 1.332,P = 0.257,Sen、Spe、+LR、-LR、DOR的Q值分别为14.94(P = 0.09)、13.37(P = 0.15)、12.65(P = 0.18)、16.37(P = 0.06)、12.92(P = 0.17),各研究间无异质性。
2.4 meta分析
BT診断胃排空延迟合并Sen为0.826(95%CI:0.728~0.894)、合并Spe为0.876(95%CI:0.800~0.925)、合并+LR为6.640(95%CI:3.987~11.060)、合并-LR为0.198(95%CI:0.122~0.321)、合并DOR为33.506(95%CI:14.671~76.525)。见图4~8。由验前概率(20%)和+LR(7)推算出62%的验后概率,由验前概率和0.20的-LR推算出5%的验后概率(图9)。SROC AUC=0.92(图10)。
2.5 发表偏倚
Deek′s漏斗图得到P = 0.443,提示本meta分析结果不存在发表偏倚。见图11。
3 讨论
本研究纳入10项研究[12,21-29](胃排空延迟患者149例,健康对照者285例),对呼气试验诊断胃排空延迟进行系统评价,结果显示各研究的合并Sen为0.83,合并Spe为0.88,AUC为0.92,提示呼气试验对诊断胃排空延迟具有很高的临床价值。通过研究也可发现呼气试验的一些缺陷,如呼气试验所得半排时间与核素扫描不一致,这可能与13C在体内的代谢有关,可通过相关公式对结果进行矫正[30]。
截至目前,作者尚未检索到其他同类研究,本研究可能是首个判断胃排空延迟呼气试验诊断准确性的meta分析。然而本研究仍存在一定局限性:研究者缺乏部分数据库的访问权限和灰色文献的获取方式;纳入研究较少、各研究中的样本量也较小;研究对象以白人为主且年龄跨度较大,基础疾病存在差异;各医疗中心在试验时试餐的固相或液相的选择不同,以上因素均限制了研究结果的普适性。
综上,呼气试验是检测胃排空延迟的有效方法,具有较高的Sen和Spe,未来需要更多关于呼气试验的大样本、多中心、设计优良的诊断试验,以客观评估其诊断价值,推广临床应用。
[参考文献]
[1] Camilleri M,Parkman HP,Shafi MA,et al. Clinical guideline: management of gastroparesis [J]. Am J Gastroenterol. 2013,108(1):18-37.
[2] Dibaise JK,Patel N,Noelting J,et al. The relationship among gastroparetic symptoms,quality of life,and gastric emptying in patients referred for gastric emptying testing [J]. Neurogastroenterol Motil,2016,28(2):234-242.
[3] 徐菁菁,曹忠耀,范志勇,等.高血糖与糖尿病胃轻瘫发生机制的研究现状[J].中国中西医结合消化杂志,2011, 19(5):338-341.
[4] Zhao X,Mashimo H. Current and Emerging Medical Therapies for Gastroparesis [J]. Curr Treat Options Gastroenterol,2015,13(4):452-72.
[5] Bestetti A,Capozza A,Lacerenza M,et al. Delayed Gastric Emptying in Advanced Parkinson Disease:Correlation with Therapeutic Doses [J]. Clin Nucl Med,2017,42(2):83-87.
[6] Nojiri M,Yukihiro Y,Takashi M,et al. Impact of the gastrojejunal anatomic position as the mechanism of delayed gastric emptying after pancreatoduodenectomy [J]. Surgery,2018,163(5):1063-1070.
[7] Hanjay W,Adam D,Ronald F,et al. Delayed gastric emptying after living donor hepatectomy for liver transplantation [J]. Case Rep Transplant,2014,2014:582183.
[8] Abell TL,Camilleri M,Donohoe K,et al. Consensus Recommendations for Gastric Emptying Scintigraphy:A Joint Report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine [J]. Am J Gastroenterol,2008,103(3):753-763.
[9] Hejazi RA,Sarosiek I,Roeser K,et al. Does grading the severity of gastroparesis based on scintigraphic gastric emptying predict the treatment outcome of patients with gastroparesis? [J]. Digest Dis Sci,2011,56(4):1147-1153.
[10] Pathikonda M,Sachdeva P,Malhotra N,et al. Gastric emptying scintigraphy:is four hours necessary? [J]. J Clin Gastroenterol,2012,46(3):209-215.
[11] Surdea-Blaga T,David L,Dumitrascu DL. The Use of Breath Test for the Assessment of Gastric Emptying Rate in Clinical Practice [A]. International Conference on Advancements of Medicine and Health Care through Technology; 5th-7th June 2014,Cluj-Napoca,Romania. Springer International Publishing,2014:53-56.
[12] Ghoos YF,Maes BD,Geypens BJ,et al. Measurement of gastric emptying rate of solids by means of a carbon-labeled octanoic acid breath test [J]. Gastroenterology,1993,104(6):1640-1647.
[13] Barzakova Emona S,Schulze-Hagen M,Zimmermann M,et al. Monitoring Liver Function of Patients Undergoing Transarterial Chemoembolization (TACE) by a 13C Breath Test (LiMAx)[J]. Cardiovasc Inter Rad,2019,42(12):1702-1708.
[14] Leonilde B,Ignazio G,Giuseppe P,et al. Dynamic carbon 13 breath tests for the study of liver function and gastric emptying [J]. Gastroenterol Rep,2014,3(1):12-21.
[15] 王莎莎,王永席,翟紅兵,等.13C-辛酸呼气试验对反流性食管炎患者胃排空功能的检测[J].中国中西医结合消化杂志,2011,19(4):247-248.
[16] Parkman HP. Assessment of gastric emptying and small-bowel motility:scintigraphy,breath tests,manometry,and Smart Pill [J]. Gastrointest Endosc Clin N Am,2009,19(1):49-55.
[17] Navas CM,Patel NK,Lacy BE. Gastroparesis:Medical and Therapeutic Advances [J]. Dig Dis Sci,2017,62(9):2231-2240.
[18] Choi MG,Camilleri M,Burton DD,et al. [13C] octanoic acid breath test for gastric emptying of solids: Accuracy,reproducibility,and comparison with scintigraphy [J]. Gastroenterology,1997,112(4):1155-1162.
[19] Ghoos YF,Maes BD,Geypens BJ,et al. Measurement of gastric emptying rate of solids by means of a carbon-labeled octanoic acid breath test [J]. Gastroenterology,1993, 104(6):1640-1647.
[20] Sanaka M,Yamamoto T,Kuyama Y. Theoretical flaws in gastric emptying breath test:Why is it dubious? [J]. Dig Dis Sci,2005,50(1):15-17.
[21] Szarka LA,Camilleri M,Vella A,et al. A Stable Isotope Breath Test with a Standard Meal for Abnormal Gastric Emptying of Solids in the Clinic and in Research [J]. Clin Gastroenterol H,2008,6(6):635.
[22] Bromer MQ,Kantor SB,Wagner DA,et al. Simultaneous Measurement of Gastric Emptying with a Simple Muffin Meal Using [13C] Octanoate Breath Test and Scintigraphy in Normal Subjects and Patients with Dyspeptic Symptoms [J]. Dig Dis Sci,2002,47(7):1657-1663.
[23] Dickman R,Steinmetz A,Bernnstine H,et al. A novel continuous breath test versus scintigraphy for gastric emptying rate measurement [J]. J Clin Gastroenterol,2011,45(1):22-25.
[24] Dickman R,Zilper T,Steinmetz A,et al. Comparison of continuous breath test and gastric scintigraphy for the measurement of gastric emptying rate in healthy and dyspeptic individuals [J]. Eur J Gastroen Hepat,2013,25(3):291-295.
[25] Chapman MJ,Besanko LK,Burgstad CM,et al. Gastric emptying of a liquid nutrient meal in the critically ill: relationship between scintigraphic and carbon breath test measurement [J]. Gut,2011,60(10):1336-1343.
[26] Pfaffenbach B,Wegener M,Adamek RJ,et al. Non-invasive 13C octanoic acid breath test for measuring stomach emptying of a solid test meal--correlation with scintigraphy in diabetic patients and reproducibility in healthy probands [J]. Z Gastroenterol,1995,33(3):141.
[27] Ziegler D,Schadewaldt P,Pour MA,et al. [13C] octanoic acid breath test for non-invasive assessment of gastric emptying in diabetic patients: validation and relationship to gastric symptoms and cardiovascular autonomic function [J]. Diabetologia,1996,39(7):823.
[28] Delbende B,Perri FO,Leodolter A,et al. 13C-octanoic acid breath test for gastric emptying measurement [J]. Eur J Gastroenterol Hepatol,2000,12(1):85-91.
[29] Nastou D,Owen E,Jaboli FM,et al. PTU-146 The Trinity of Gastric Emptying Scintigraphy,13C Acetate Gastric Emptying Breath Testing,and Real Time Gastric Ultrasonography Indicates High Prevalence of Gastric Motor Dysfunction In Functional Dyspepsia [J]. Gastroenterology,2014,63(Suppl 1):A102-A103.
[30] Sanaka M,Nakada K,Nosaka C,et al. The Wagner-Nelson method makes the [13C]-breath test comparable to radioscintigraphy in measuring gastric emptying of a solid/liquid mixed meal in humans [J]. Clin Exp Pharmacol Physiol,2007,34(7):641-644.
(收稿日期:2019-10-21 本文編辑:刘永巧)
