Impaired immune reaction and increased lactate and C-reactive protein for early prediction of severe morbidity and pancreatic fistula after pancreatoduodenectomy ☆
2020-03-03MarioRodriguezLopezFranciscoTejeroPintorMartinBailonCuadradoAsterioBarreraRebolloBaltasarPerezSaboridoDavidPachecoSanchez
Mario Rodriguez-Lopez , Francisco J. Tejero-Pintor , Martin Bailon-Cuadrado , Asterio Barrera-Rebollo, Baltasar Perez-Saborido, David Pacheco-Sanchez
General and Digestive Surgery Department, Rio-Hortega University Hospital, Dulzaina 2, 47012 Valladolid, Spain
Keywords: Pancreatoduodenectomy Morbidity Pancreatic fistula Biomarker Prediction Score
ABSTRACT Background: Prediction of complications after pancreatoduodenectomy (PD) remains of interest. Blood parameters and biomarkers during first and second postoperative days (POD1, POD2) may be early indi- cators of complications. Methods: This case-control study included 50 patients. Baseline, POD1 and POD2 values of leukocytes, neutrophils, lymphocytes, platelets, hemoglobin, C-reactive protein (CRP), procalcitonin and arterial lac- tate were compared between individuals presenting Clavien ≥III morbidity, pancreatic fistula (PF) or clinically relevant PF (CRPF) and those without these morbidities. Common variables reaching significance were further analyzed in order to calculate a predictive score. Results: Severe morbidity, PF and CRPF rates were 28.0%, 26.0% and 14.0%, respectively. Patients with severe morbidity had lower leukocytes on POD2 ( P = 0.04). Patients with PF presented higher CRP on POD2 ( P = 0.001), higher lactate on POD1 ( P = 0.007) and POD2 ( P = 0.008), and lower lymphocytes on POD1 ( P = 0.007) and POD2 ( P = 0.008). Patients with CRPF had lower leukocytes and neutrophils on POD1 ( P = 0.048, P = 0.038), lower lymphocytes on POD1 ( P = 0.001) and POD2 ( P = 0.003), and higher CRP on POD2 ( P = 0.001). Baseline parameters and procalcitonin obtained no statistical associations. Score was defined according to lymphocytes on POD1 < 650/μL and CRP on POD2 ≥250 mg/L allocating patients in 3 risk categories. PF and CRPF rates were statistically higher as risk category increased ( P < 0.001). Receiver operating characteristic curves and Hosmer-Lemeshow tests showed a good accuracy. Conclusions: Impaired immunological reaction during early postoperative period (lower leukocytes and, particularly, lymphocytes) in response to surgical aggression would favor complications after PD. Likewise, acidosis (higher arterial lactate) could behave as risk factor of PF. An elevated CRP on POD2 is also an early biomarker of PF. Our novel score based on postoperative lymphocyte count and CRP seems reliable for early prediction of PF.
Introduction
Pancreatoduodenectomy (PD) is the cornerstone for treatment of malignant tumors located at the head of the pancreas and pe- riampullary region. However, postoperative morbidity rate in these patients remains high. According to the Dindo-Clavien classifica- tion [1] , overall severe complications (grade ≥III) and mortality can reach 29.1% and 4.2%, respectively, as recently reported in the national Danish series [2] . Besides, pancreatic fistula (PF) ranges from 3% to 45%, according to the International Study Group for Pancreatic Surgery (ISGPS) definition [3,4] . Biochemical leak (for- merly, grade A) is defined by quantifying amylase in drain. Thus, it is not possible to determine this complication in patients in whom no operative drain was left. The concept of clinically relevant pan- creatic fistula (CRPF) has been commonly used in literature and it includes PF grades B and C. The Danish series showed a CRPF rate of 13.6% [2] .
An impaired preoperative clinical condition, demonstrated by disturbance in some blood parameters, has been associated to complications after PD. Nonetheless, many different variables have been tested in several studies and diverse cut-off levels were obtained across them [5-8] ( Table 1 ). On the other hand, physiological response after a major surgical procedure results in an increase of acute phase reactants, white blood cell counts, platelets and other biomarkers [9] . However, we have found only 15 articles analyzing postoperative values of these parameters as predictors of complications after PD, with methodological hetero- geneity, as described in Table 2 [10-25] . White blood cells and C-reactive protein (CRP) are the most common ones among them, as well as plasmatic and drainage amylase. Conversely, there are scarce data about procalcitonin (PCT) or lactate. Time evolution during early postoperative period compared with preoperative values also has relevance (differential value, Δ), since those pa- rameters which behave as predictors should demonstrate their accuracy before complications become clinically evident.

Table 1 Preoperative parameters and biomarkers from blood analysis associated with morbidity after PD.
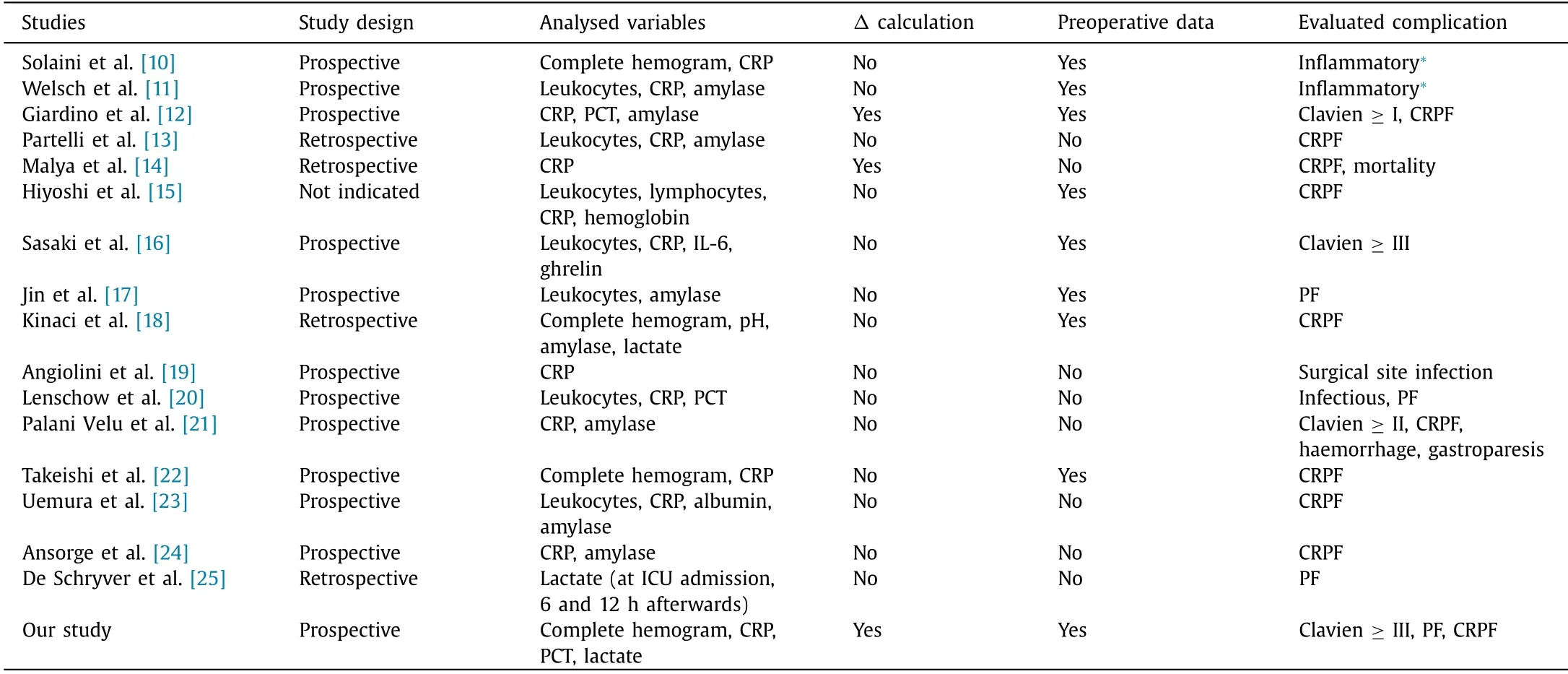
Table 2 Methods and characteristics of published studies analyzing postoperative blood parameters and biomarkers as predictors of complications after PD.
Thus, we hypothesize that patients with complications will present a different value and time pattern in blood parameters and biomarkers, compared to patients with a normal postoperative pe- riod. It could be early demonstrated on the first and second post- operative days (POD1 and POD2), as well as by calculating differ- ential values with preoperative blood analysis.
Methods
An observational case-control study was conducted at the Hepato-Biliary-Pancreatic Surgery Unit (Rio-Hortega University Hospital, Valladolid, Spain) from January 2015 to March 2018. Helsinki ethical principles for medical research involving human subjects were followed.
The inclusion criteria were ≥18 year-old patients who under- went PD and signed informed consent, regardless of diagnosis. We excluded those individuals in whom procedure was aborted due to unresectability and those who required emergency pancreatic surgery. Sample selection was made by non-probabilistic recruit- ment of all consecutive cases according to the inclusion and exclu- sion criteria.
Our established protocol for lesions located at the head of the pancreas and the periampullary region was followed in all patients. Indication of surgical treatment was decided by a multidisci- plinary committee (including surgeons, oncologists, gastroenterol- ogists, radiologists, and pathologists) after evaluating the comple- mentary tests performed in each case (usually computed tomog- raphy, magnetic resonance, endoscopic ultrasound, biopsy sam- ples and/or cytology). Neoadjuvancy was performed in case of borderline resectability. Regarding surgical technique, classical PD was completed in all individuals, associating lymphadenectomy and vascular resection when necessary. We performed end-to-side duct-to-mucosa pancreatico-jejunostomy in all patients, followed by hepaticojejunostomy and gastrojejunostomy (without pylorus- preserving), usually in a single loop fashion. Surgical drainage was routinely placed in the operative field next to the anastomosis, ex- cept in 3 patients by decision of their surgeons. All patients were transferred to intensive care unit after surgery until POD2.

Table 3 Blood parameters and biomarkers included for analysis in the whole sample (median, IQR).
Demographic variables (age, sex) were registered, as well as postoperative morbidity up to discharge, including: severe compli- cations according to the Dindo-Clavien classification (grade ≥III), overall PF rate (including biochemical leak, grade B and grade C following ISGPS) and CRPF rates (grades B and C). For diagnosis of biochemical leak, amylase-rich fluid ( > 300 IU/L, since upper limit set by our laboratory is 100 IU/L) was required to be present in drainage sample on POD4, as defined by ISGPS [3,4] .
Several pre- and postoperative clinical and analytic variables were registered in our prospective database of pancreatic surgery. The following blood parameters and biomarkers were selected for analysis: leukocytes per microliter (μL), neutrophils/μL, lympho- cytes/μL, platelets/μL, hemoglobin (g/dL), CRP (mg/L), PCT (ng/mL) and arterial lactate (mmol/L). Baseline data of these variables were collected from a preoperative blood sample obtained at the ward (immediately before operation per protocol) and from blood sam- ples at 8:00 a.m. on POD1, POD2. Only exceptions were preop- erative arterial lactate and preoperative PCT, due to ethic and cost-efficiency reasons, respectively. Moreover, three new variables named differentials ( Δ) were calculated by subtracting figures be- tween POD1 and baseline ( ΔPOD1), between POD2 and baseline ( ΔPOD2), and between second and first day (POD2-POD1) for each biomarker in each patient. Additionally, albumin (g/dL) was regis- tered but only from preoperative blood sample.
Our patients were defined as controls or cases, according to lack or presence of each one of the aforementioned complications, respectively.
Statistical analysis
Descriptive data were reported as percentage for categorical variables and median with its interquartile range (IQR) for contin- uous ones. Univariate statistical analysis using Mann-Whitney test was performed with SPSS software (Version 22.0, IBM Corporation, Armonk, NY, USA) in order to find differences in median values of specified blood parameters, biomarkers and Δ between cases and controls. Those variables obtaining statistical significance were in- cluded for discrimination analysis using receiver operating charac- teristic (ROC) curve and reporting area under curve (AUC) with its 95% confidence interval (95% CI), with the aim of finding the most accurate one for each complication. The significance level was set at P < 0.05. In case of finding common significant variables for the studied complications, cut-off values will be set and a risk cat- egory system will be established, in order to preliminary define a new predictive score based on postoperative blood parameters and biomarkers. Validation was tested by searching for univariate statistical differences in complication rates among score categories and by using ROC curve as well as Hosmer-Lemeshow “goodness of fit” test for detecting accuracy in terms of correct prediction.
Results
Fifty patients were included for analysis. Median age was 67 years (IQR: 55-70) and 29 patients were males (58.0%). Patients received neoadjuvant therapy were excluded. Severe complications (Clavien ≥ III) occurred in 14 patients (28.0%), three (6.0%) of whom died. Reoperation rate was 12.0% (4 cases of hemorrhage grade B/C and 2 cases of CRPF) and 13 patients (26.0%) suffered PF, of whom 7 (14.0%) were CRPF. Median in-hospital length of stay was 12 days (IQR: 10-20).
Blood parameters, biomarkers and Δ are shown in Table 3 . Sta- tistical analysis of each complication (severe morbidity, PF, CRPF) found no significant differences between cases and controls for baseline parameters and biomarkers. Preoperative albumin was not statistically different either.
We found that patients suffering severe morbidity had a sig- nificant lower median of leukocytes on POD2 ( Fig. 1 ), as well as its ΔPOD2 than control patients ( P = 0.040 and P = 0.049, respectively) ( Table 4 ). ROC curves showed AUC of 0.685 (95% CI: 0.529-0.840, P = 0.044) and 0.681 (95% CI: 0.527-0.834, P = 0.049), respectively. No other variables were statistically significant.
Cases with PF presented a statistical higher value of CRP on POD2 ( P = 0.001) ( Fig. 2 A) and its ΔPOD2 ( P = 0.002). Lactate was also higher on POD1 and POD2 among cases ( P = 0.007 and P = 0.008, respectively) ( Fig. 2 B). Conversely, lymphocyte counts on POD1 and POD2 were inferior in patients with PF ( P = 0.007 and P = 0.008, respectively) ( Fig. 2 C and Table 5 ). AUC of ROC curves for these variables obtaining significance were:
- CRP on POD2: AUC = 0.790 (95% CI: 0.636-0.944, P = 0.002).
- ΔPOD2 for CRP: AUC = 0.763 (95% CI: 0.590-0.936, P = 0.005).
- Lymphocyte on POD1: AUC = 0.709 (95% CI: 0.546-0.872, P = 0.026).
- Lymphocyte on POD2: AUC = 0.741 (95% CI: 0.583-0.900, P = 0.01).
- Lactate on POD1: AUC = 0.755 (95% CI: 0.602-0.908, P = 0.007).
- Lactate on POD2: AUC = 0.748 (95% CI: 0.610-0.887, P = 0.008).
Finally, we found statistically lower counts of leukocytes ( Fig. 3 A) and neutrophils on POD1 among patients who suffered CRPF ( P = 0.048 and P = 0.038, respectively). Moreover, ΔPOD1 for neutrophils was also significantly lower ( P = 0.036). Similarly, lym- phocytes were decreased both on POD1 and POD2 ( P = 0.001 and P = 0.003, respectively) ( Fig. 3 B). On the contrary, CRP value was higher among cases with CRPF on POD2 ( Fig. 3 C) and ΔPOD2 ( P = 0.001 and P = 0.003, respectively) ( Table 6 ). AUCs for these variables were:
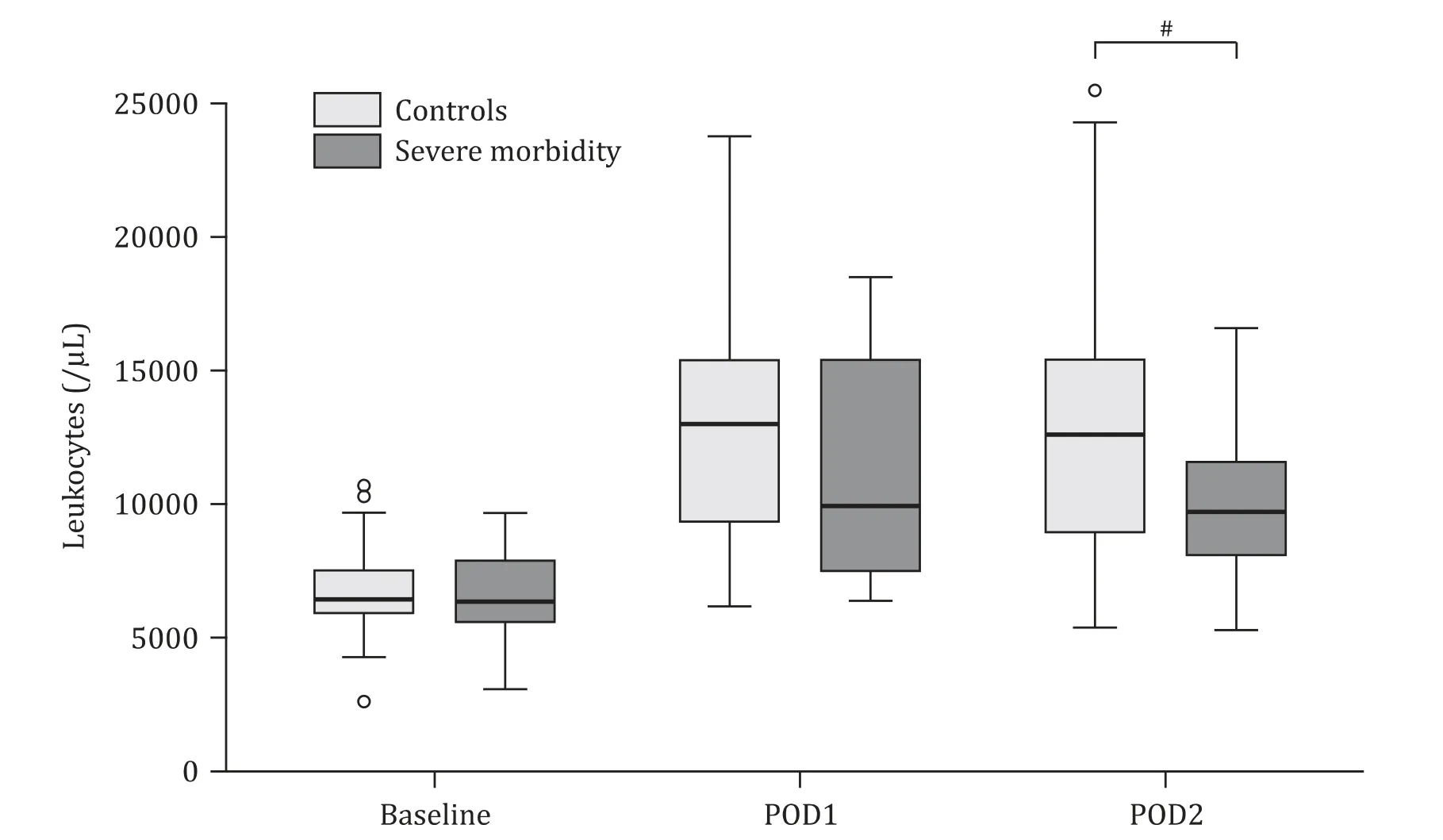
Fig. 1. Box-graphic showing temporal evolution (baseline, POD1, POD2) for median value of leukocytes/μL between patients with and without severe morbidity (Clavien ≥III). #: P < 0.05. POD: postoperative day.

Table 4 Blood parameters and biomarkers among patients with Clavien ≥III morbidity and controls (median, IQR).
- Leukocytes on POD1: AUC = 0.749 (95% CI: 0.553-0.945, P = 0.036).
- Neutrophils on POD1: AUC = 0.754 (95% CI: 0.544-0.964, P = 0.032).
- ΔPOD1 for neutrophils: AUC = 0.759 (95% CI: 0.575-0.943, P = 0.029).
- CRP on POD2: AUC = 0.756 (95% CI: 0.571-0.940, P = 0.031).
- ΔPOD2 for CRP: AUC = 0.761 (95% CI: 0.590-0.932, P = 0.028).
- Lymphocytes on POD1: AUC = 0.872 (95% CI: 0.776-0.968, P = 0.002). This is the highest AUC of all analyzed blood param- eters and biomarkers ( Fig. 4 ).
- Lymphocytes on POD2: AUC = 0.839 (95% CI: 0.720-0.958, P = 0.004).
Lymphocytes on POD1 and CRP on POD2 were selected as the two most reliable variables associated with both PF and CRPF. Cut- off values were set as follows:
- Lymphocytes on POD1 = 650/μL. Sensitivity and specificity for PF were 0.69 and 0.78, and for CRPF were 1 and 0.77, respectively.
- CRP on POD2 = 250 mg/L. Sensitivity and specificity values for PF were 0.69 and 0.87, and for CRPF were 0.71 and 0.79, respectively.
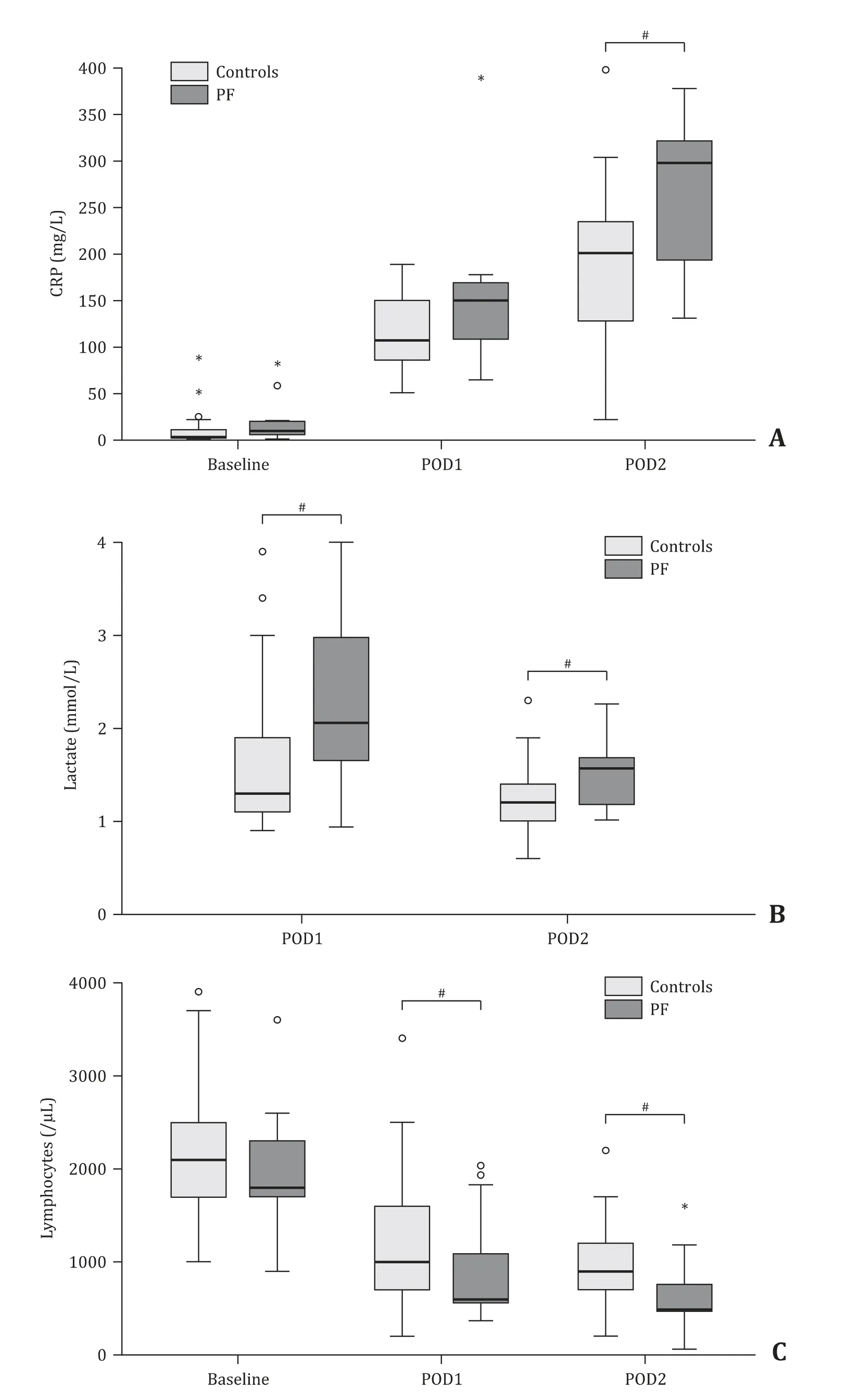
Fig. 2. Graphics showing temporal evolution (baseline, POD1, POD2) for median value of CRP (mg/L) ( A ), lactate (mmol/L) ( B ) and lymphocytes/μL ( C ) between patients with and without PF. #: P < 0.05. CRP: C-reactive protein; POD: postoperative day; PF: pancreatic fistula.
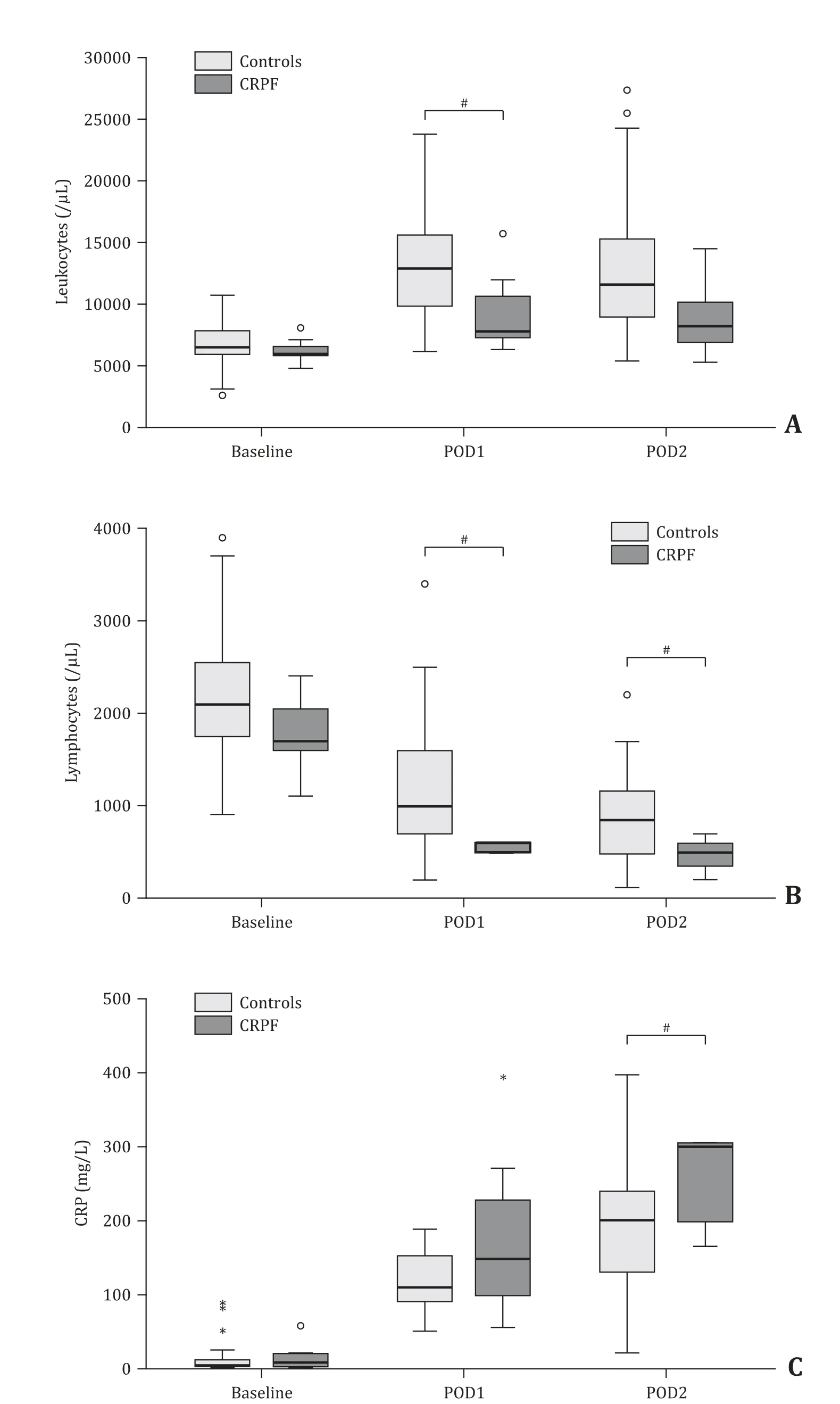
Fig. 3. Graphics showing temporal evolution (baseline, POD1, POD2) for median value of leukocytes/μL ( A ), lymphocytes/μL ( B ) and CRP (mg/L) ( C ) and between patients with and without CRPF. #: P < 0.05. POD: postoperative day; CRP: C-reactive protein; CRPF: clinically relevant pancreatic fistula.
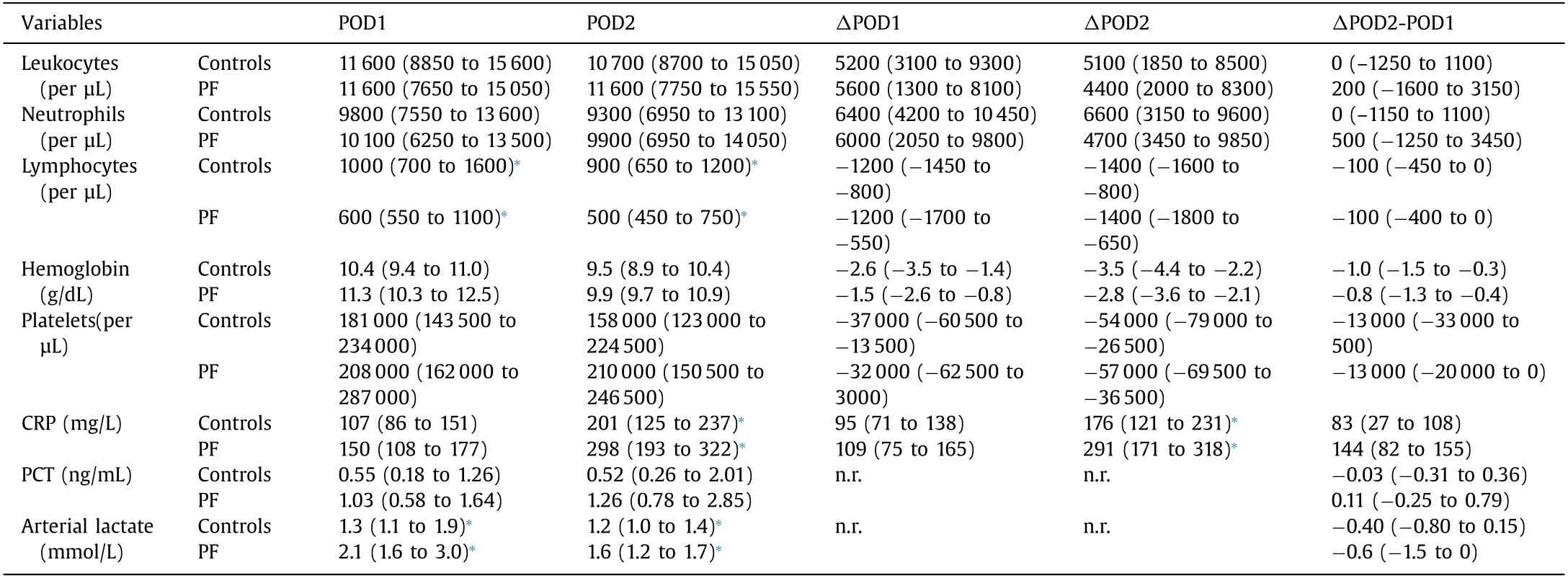
Table 5 Blood parameters and biomarkers among patients with PF and controls (median, IQR).
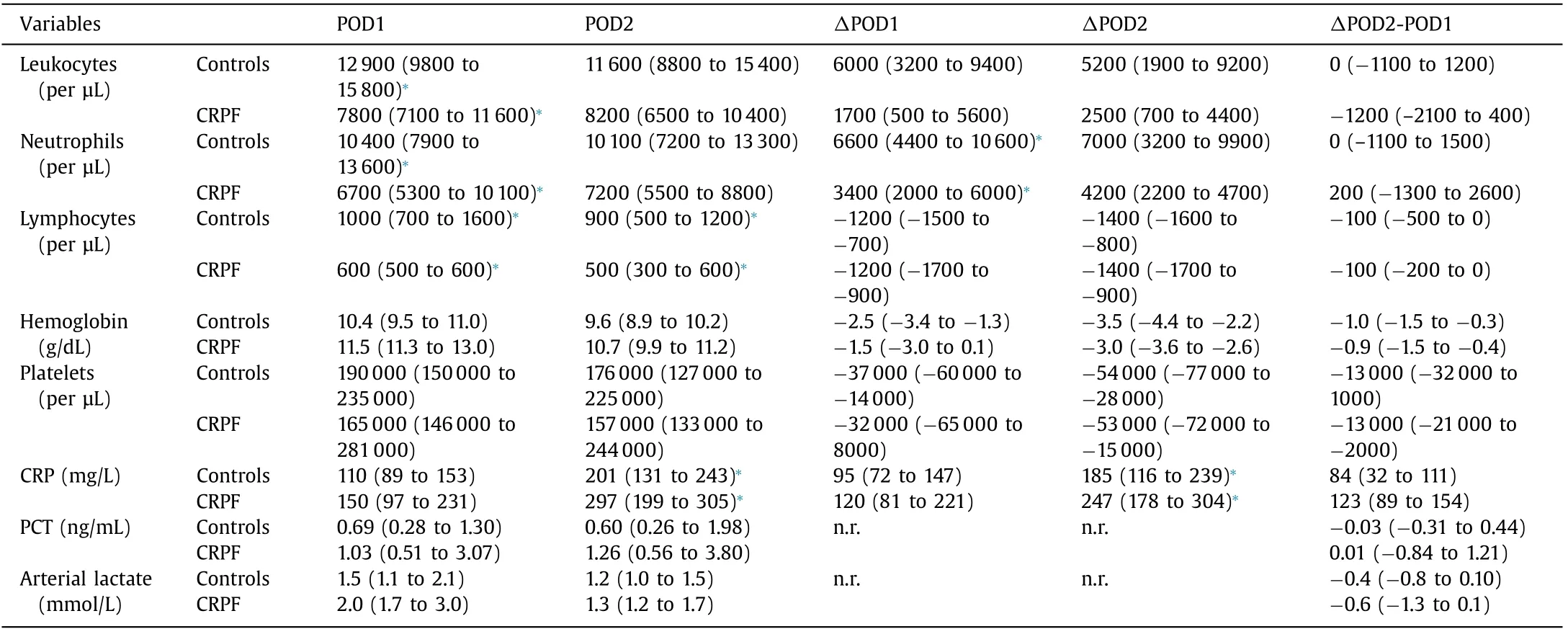
Table 6 Blood parameters and biomarkers among patients with CRPF and controls (median, IQR).
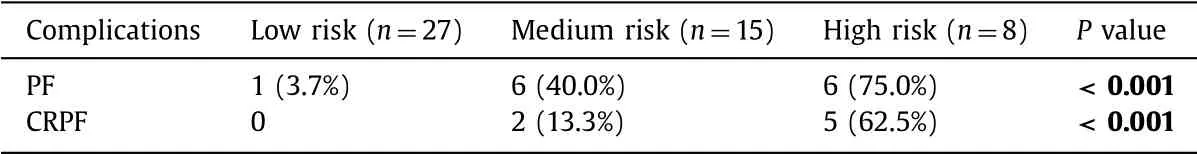
Table 7 PF and CRPF rates according to our score categories based on lymphocytes on POD1 and CRP on POD2.
According to these values, we defined those as high-risk pa- tients who had lymphocytes on POD1 < 650 /μL and CRP on POD2 ≥ 250 mg/L. Medium-risk group were those with either lymphocytes on POD1 < 650 /μL or CRP on POD2 ≥250 mg/L. Low-risk patients met none of these criteria. Consequently, risk category distribution was: 27 low-risk patients (54%), 15 medium- risk patients (30%) and 8 high-risk patients (16%). PF and CRPF rates were statistically higher as risk category increased ( P < 0.001) ( Table 7 ). Low and high risk groups included 70% of the sample size. Discrimination analysis for PF and CRPF of this new score was performed by ROC curves, obtaining AUC = 0.857 (95% CI: 0.738-0.975, P < 0.001) and AUC = 0.912 (95% CI: 0.819-1.0 0 0, P = 0.001) ( Fig. 5 ), respectively. Hosmer-Lemeshow test showed an accuracy for correctly predicted risk of 82.0% ( P = 0.416) and 90.0% ( P = 0.558) for PF and CRPF, respectively.

Fig. 4. ROC curve obtained for discrimination analysis of lymphocytes on POD1 in relation to CRPF. AUC = 0.872 (95% CI = 0.776-0.968, P = 0.002). ROC: receiver op- erating characteristic; POD: postoperative day; CRPF: clinically relevant pancreatic fistula; AUC: area under curve.
Discussion
Severe morbidity rate (defined as grade ≥III according to the Dindo-Clavien classification [1] ) after PD remains high: around 30%, as reported by large multicentric series [2,26] . Regarding PF and CRPF (following ISGPS definitions), their incidences reach rates up to 45% and 15-20%, respectively [2-4,26] . Therefore, predic- tion of these complications is of notorious interest. Some blood parameters and biomarkers from preoperative samples have been associated to an increased risk of morbidity and mortality [5-8] . Nonetheless, we have found very few studies to date, analyzing their numeric evolution after PD (preoperative and during initial postoperative period), with the aim of detecting trends which may early predict appearance of complications [10-24] .
Our demographic results are similar to those reported in litera- ture, with a slightly higher proportion of male patients older than 60 years old [2] . Our severe complications and CRPF rates also re- semble those reported by National Danish and U.S.A. series [2,26] . The concept of CRPF usually includes grades B and C, accord- ing to ISGPS classification [4] . Conversely, biochemical leak (pre- viously defined as grade A) involves the presence of rich-amylase fluid from drainage without clinical deterioration. In the absence of drainage, biochemical leak cannot be determined. In our work, we have analyzed both overall PF and CRPF, since surgical drainage was not present in 3 patients, as suggested by PANDRA Trial [27] .
As previously mentioned, there are few articles analyzing se- vere complications after PD and related postoperative biomarkers and immune cells. Sasaki et al. [16] observed that CRP was sta- tistically higher in patients with severe morbidity on POD3, POD7 and POD14, though leukocytes did not show any relation to severe complications. Likewise, other studies found that patients suffering Clavien ≥I or ≥II morbidity presented higher CRP value than con- trols [12,21] . Conversely, we demonstrated that only leukocytes on POD2 showed statistical differences (lower count in patients who presented Clavien ≥III complication). Other papers included infec- tious or inflammatory complications without establishing Clavien’s grade [10,11,20] . Thus, their studies are not comparable to ours.

Fig. 5. ( A ) ROC curve obtained for discrimination analysis of the new score based on lymphocytes on POD1 and CRPF on POD2 in relation to CRPF. AUC = 0.912 (95% CI: 0.819-1.0 0 0, P = 0.001); ( B ) ROC curve obtained for discrimination analysis of the new score based on lymphocytes on POD1 and CRPF on POD2 in relation to PF. AUC = 0.857 (95% CI: 0.738-0.975, P < 0.001). ROC: receiver operating char- acteristic; POD: postoperative day; CRP: C-reactive protein; CRPF: clinically relevant pancreatic fistula; AUC: area under curve.
There are few studies analyzing overall PF and postoperative leukocyte counts. They have not confirmed statistical association, which is in line with our data [17,20] . However, we have observed, for the first time, that patients with PF had significantly lower lym- phocyte counts on POD1 and POD2 than controls. Higher lactate value on POD1 and POD2 was also observed in cases of PF, which has been scarcely analyzed in literature. Kinaci et al. [18] detected higher but non-statistical value of this molecule at the end of PD in patients with CRPF. De Schryver et al. [25] also found that pa- tients with PF had significantly higher levels of lactate 6 h after concluding pancreatic resections (82% of their patients underwent PD).
The association between CRPF and preoperative blood param- eters and biomarkers (leukocytes, lymphocytes, hemoglobin, albu- min, amylase and CRP) was evaluated by Hiyoshi et al. [15] and Takeishi et al. [22] . They found no statistical differences, same as we observed in our patients. Postoperative values of leukocytes, platelets and hemoglobin did not obtain statistical significance ei- ther, confirming published data [12,15,18,22,23] . Some studies have shown a relationship between postoperative CRP and CRPF. This molecule is an acute phase reactant synthesized by the liver during acute and chronic systemic inflammation. Therefore, its increase is understandable when postoperative morbidity appears. Curiously, CRP on POD1 reached statistical significance neither in ours nor in those articles [12-15,21,23,24] . On the other hand, postopera- tive CRP showed highest AUC on POD3 or POD4 in most of these articles. We have not registered data beyond POD2 with the aim of evaluating parameters and biomarkers which may behave as very early predictors of morbidity. Once a complication becomes clin- ically evident, there is no role for predictive value of these vari- ables. Finally, Giardino et al. found that postoperative PCT is a spe- cific biomarker for CRPF [12] . Lenschow et al. [20] also found that PCT is higher in patients with PF after PD. However, PCT is not useful in differential diagnosis of PF after PD.
As a novelty, we found that patients presenting complications (severe morbidity, PF or CRPF) had altogether a trend to lower im- mune cells counts (leukocytes, neutrophils and lymphocytes) than controls. Particularly, lymphocytes on POD1 and POD 2 were the most reliable parameter (highest AUC) to predict CRPF. This sup- ports a theory that patients with an inadequate immune response after surgical injury might be at higher risk of suffering a pancre- atic anastomosis failure. Besides, tissue hypoxia and acidosis (evi- denced by higher lactate) might provoke precarious healing in pan- creatic anastomosis after PD, as it has been described for general wound healing [28] . This would constitute a second relevant factor for development of PF. As previously stated, lactate on POD1 and POD2 were higher among our patients with PF.
Finally, only two articles have included the Δ mathematical concept for analytic variables [12,14] . ΔPOD2 leukocytes in pa- tients suffering Clavien ≥III morbidity, ΔPOD2 CRP in patients with PF, ΔPOD2 CRP and ΔPOD1 neutrophils in cases of CRPF reached statistical significance in our study. Nevertheless, their AUCs were very similar or even lower than original variables. We therefore considered that Δ calculation does not add clear advan- tage for early prediction of complications after PD.
Since lymphocytes on POD1 and CRP on POD2 were statisti- cally associated with both PF and CRPF, obtaining high AUC, they were selected for defining a new predictive score. Cut-off values for these two variables were established with acceptable sensitiv- ity and specificity for the aforementioned postoperative complica- tion: low lymphocyte count on POD1 ( < 650 /μL) and high CRP on POD2 ( ≥250 mg/L). Those patients with both criteria were allo- cated to high-risk category, while those who presented only one of them were at medium-risk group. Univariate analysis of this novel score was satisfactory: there was significantly higher rate of PF and CRPF as the risk category increased. High and low-risk categories included 70% of our sample size and validation test showed a good accuracy. Consequently, this constitutes a predictive score for PF and CRPF based on our results. The impaired immunological state (low lymphocyte count on POD1) and increased systemic inflam- matory response (high CRP on POD2) at the very early stage af- ter PD correlated with PF. To our knowledge, we are the first to demonstrate the usefulness of such a score on the prediction of PF. We believe that this score optimized postoperative period. The ap- plication of this score may avoid unnecessary imaging and guide the patients to early oral intake. Consequently, hospital length of stay sanitary may shorten and sanitary costs may decrease.
This study has some limitations, such as the small sample size and its unicentric data collection. In addition, we have registered complications during hospital stay, which underestimated the mor- bidity rate. Despite this, the main interest of our study is to in- crease knowledge on the mechanism and systemic response in pa- tients with pancreatic fistula after PD, as well as the novel score herein described. Our results should be validated by larger sample size studies.
In conclusion, an impaired immunological reaction (particu- larly, remarkable decrease in lymphocytes) in response to surgi- cal aggression at the early postoperative period of PD would favor Clavien ≥III morbidity, PF and CRPF. Acidosis is a risk factor of PF. An elevated CRP on POD2 is an early biomarker of PF and CRPF. PCT, hemoglobin and platelet counts before and after PD were not associated with complications.
CRediT authorship contribution statement
Mario Rodriguez-Lopez:Conceptualization, Data curation, For- mal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing - origi- nal draft, Writing - review & editing.Francisco J Tejero-Pintor:Data curation, Formal analysis, Investigation, Methodology, Soft- ware, Validation, Visualization, Writing - review & editing.Martin Bailon-Cuadrado:Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing - review & editing.Asterio Barrera-Rebollo:Investigation, Methodology, Software, Validation, Visualization, Writing - review & editing.Baltasar Perez-Saborido:Formal analysis, Investigation, Method- ology, Software, Validation, Visualization, Writing - review & edit- ing.David Pacheco-Sanchez:Investigation, Methodology, Software, Validation, Visualization, Writing - review & editing.
Funding
None.
Ethical approval
Clinical data were obtained from our approved database. This is an observational study with no intervention over the patients.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the sub- ject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Impact of EBV infection and immune function assay for lymphoproliferative disorder in pediatric patients after liver transplantation: A single-center experience
- Hepatobiliary&Pancreatic Diseases International
- Intraoperative management and early post-operative outcomes of patients with coronary artery disease who underwent orthotopic liver transplantation
- Acute onset of autoimmune hepatitis in children and adolescents
- Liver stiffness as a predictor of hepatocellular carcinoma behavior in patients with hepatitis C related liver cirrhosis ✩
- Treatment and prognosis of hepatic epithelioid hemangioendothelioma based on SEER data analysis from 1973 to 2014