Intraoperative management and early post-operative outcomes of patients with coronary artery disease who underwent orthotopic liver transplantation
2020-03-03HiYingKongXinZhoKuiRongWng
Hi-Ying Kong , Xin Zho , Kui-Rong Wng ,*
a Department of Anesthesiology, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310 0 03, China
b Department of Anesthesiology, International Hospital, Zhejiang University, Hangzhou 310 0 0 0, China
Keywords: Orthotopic liver transplantation Coronary artery disease Post-reperfusion syndrome
ABSTRACT Background: Coronary artery disease (CAD) is frequently observed in aging end-stage liver disease (ESLD) patients who require orthotopic liver transplantation (OLT). This situation is challenging for both the pa- tients and the medical staff. Methods: We retrospectively studied the case records of 26 ESLD patients with CAD who underwent OLT with total clamping of the inferior vena cava between 2014 and 2018. We analyzed the details of the pre-operative evaluation, intraoperative anesthetic management and post-operative prognosis of these patients. Results: All patients tolerated the anhepatic stage well. Post-reperfusion syndrome (PRS) was observed in 13 patients (50%) and 2 of them were severe but corrected well. ST-segment depression was frequently observed during the anhepatic stage and reperfusion stage. No mortality due to cardiac-related events occurred among the patients during hospitalization. OLT with the modified piggyback technique could successfully be performed in ESLD patients with mild and moderate CAD. Conclusions: A thorough evaluation and optimization of recipients, strict monitoring and optimized man- agement of circulation, knowledge of the complicated changes during OLT procedures, and strategies to ameliorate post-reperfusion syndrome favorite the outcomes.
Introduction
Orthotopic liver transplantation (OLT) is regarded as a valid treatment for end-stage liver disease (ESLD). Coronary artery disease (CAD) is frequently observed in aging ESLD patients who require OLT [1-3] . The key to the management of the patients with CAD under surgery is maintaining the balance between the oxygen supply and myocardial demands. However, ESLD patients requiring OLT usually exhibit increased cardiac output (CO), low systemic vascular resistance (SVR), and high peripheral blood volume but low central blood volume [4] . These physiologic alterations and altered hemodynamic stresses faced by OLT patients during the dissection phase, anhepatic phase and early reperfusion phase may result in an imbalance between oxygen supply and demand and lead to severe cardiac events [5] . Although anesthetic and surgical techniques have markedly improved, the presence of CAD is considered a relative contraindication to liver transplantation at most transplant centers.
OLT candidates with CAD or other coronary risk factors are prone to post-reperfusion syndrome (PRS) [5 , 6] . PRS is asso- ciated with acute kidney injury (AKI) after OLT [7] . Therefore, the proper intraoperative strategies to decrease the risk of PRS might have the potential to reduce the severe complications and improve recipient survival. However, reports related to intraoper- ative management are scarce, and only two case reports concern perioperative management [8 , 9] . One case report described the perioperative management of living-related liver transplantation (LRLT) in two CAD patients using a surgical technique avoiding the total clamping of the inferior vena cava (IVC) [8] . Another report described the successful management of coronary artery bypass graft (CABG)-OLT in nine severe CAD patients using veno-venous bypass [9] . To the best of our knowledge, the modified piggyback technique is usually used in OLT in most centers to reduce the operative time. Compared to the above two techniques, more significant hemodynamic changes have been observed during the anhepatic stage using the modified piggyback technique in OLT [10] . Therefore, the management of this series of patients undergoing OLT with the modified piggyback technique might be more challenging for anesthesiologists. Here, we reported our experience with managing a special population of patients undergoing OLT and particularly focused on the optimization of anesthesia management and operative skills to reduce the occurrence of PRS and cardiac events during the procedure.
Methods
Study design
This study was approved by the Ethics Committee of the First Affiliated Hospital, Zhejiang University School of Medicine, and written informed consent was obtained from the patients or their relatives. We retrospectively studied the case records of ESLD pa- tients with CAD who underwent OLT with total clamping of the IVC between March 2014 and February 2018 and analyzed the de- tails of the pre-operative evaluation, the intraoperative anesthetic management and the post-operative course of these patients.
The collected data included demographic profiles, indications for transplantation, details of cardiac evaluation and comorbidi- ties, cold ischemia times (CITs), duration of surgery, monitoring, fluid management, transfusion requirements, hemodynamic vari- ables, vasopressor use, PRS, cardiac events, urine output, duration of mechanical ventilation, intensive care unit (ICU) stay and hospi- tal stay, any adverse events noted during the hospital stay and pa- tient and graft survival post-liver transplant. The calculated model for end-stage liver disease (MELD) score and Child classification was used to evaluate the severity of chronic liver disease in the recipients.
The American Heart Association classification of CAD severity was introduced to categorize the recipients with CAD based on stenosis in at least one of the three major vessels on angiogram: < 50% (no/mild CAD) and > 50% (moderate/severe CAD) [11] . PRS was defined as a decrease in the mean arterial pressure (MAP) greater than 30% relative to the value at the end of the anhep- atic phase and lasting for at least 1 min within the first 5 min af- ter liver reperfusion [12] . Acute myocardial ischemia (AMI) was de- fined as a troponin-I level greater than 0.04 ng/mL and evidence of myocardial ischemia was indicated by symptoms, ECG changes or imaging evidence. Heart failure was defined by the clinical symp- toms, radiographic evidence, jugular venous distention and ele- vated B-type natriuretic peptide ( > 100 pg/mL). Death due to heart failure, sudden cardiac death, dysrhythmia or acute coronary syn- drome was regarded as cardiac-related mortality.
Anesthesia and monitoring
General anesthesia was induced with weight-related doses of fentanyl, midazolam and rocuronium and maintained with 2% -3% sevoflurane in air/oxygen, 2-3 mg/kg/h propofol and 10-30 μg/kg/h remifentanil. The bispectral index was maintained at 40-60. Two arterial cannulas were placed in the left and right radial arteries as follows: one for continuous blood pressure monitoring and one for blood specimen collection. In addition to routine monitoring, such as five-lead electrocardiogram, blood pressure, pulse oxygen saturation and central venous pressure (CVP), pulse contour cardiac output monitoring (PiCCO) and transesophageal ultrasound (TEE) were also introduced according to the patients’ clinical situation.

Fig. 1. Strategies for preventing post-reperfusion syndrome (PRS) of liver transplan- tation for patients with coronary artery disease.
Measures to prevent PRS
The patients received target-directed fluid therapy, and the MAP was maintained above 60 mm Hg during the procedure. Dur- ing the dissection phase and anhepatic phase, a mild restrictive fluid strategy was used to maintain the CVP below 7 mm Hg or stroke volume variation (SVV) between 13% and 20%, while the target SVV was less than 13% after reperfusion. Ringer’s lactate solution was administered at 1 mL/kg/h. A bolus dose of 5% al- bumin (200 mL) was administered while the SVV was greater than the target SVV, and the cardiac output index (CI) was less than 2.5 L/min/m2. The albumin bolus was repeatedly adminis- tered at frequent intervals until the target SVV and CI levels were achieved. Norepinephrine and/or vasopressin were administered to maintain the systemic vascular resistance index (SVRI) between 10 0 0 and 2500 dyn.s/cm5/m2. The norepinephrine administration was initiated at a dose of 1-2 μg/kg/min and increased slowly to maintain the target SVRI and MAP. Vasopressin infusion was initiated if the MAP was < 60 mm Hg or the heart rate (HR) was > 100 beats/min. Additional dopamine starting from a dose of 2 μg/kg/min or epinephrine starting from a dose of 0.05 mg/kg/min was introduced if the CI was continuously low ( < 2.5 L/min/m2).
In addition, 0.5 g/kg mannitol was routinely administered slowly from the end of the anesthesia induction to the comple- tion of the graft liver implantation. Diltiazem (1 μg/kg/min) was administered during this procedure to dilate the coronary artery and slow the HR. Fluid boluses and inotropes were administered to prepare for the IVC trial.
During anastomosis of the suprahepatic caval vein, the graft was flushed with 500 mL of 5% albumin (0 °C) through the portal vein. Subsequently, the portal vein was unclamped, and 4-6 mL/kg of blood were vented through the portal vein. The absolute vol- ume varied according to the patient’s situation, such as the pa- tient’s MELD score, the weight of the donor liver, and the preload before reperfusion. Then the inferior vena cava was unclamped. Fi- nally, hepatic arterial anastomosis was performed, followed by bile duct reconstruction. No veno-venous bypass was performed during the anhepatic period.
During reperfusion, calcium chloride (0.5 g), sodium bicarbon- ate (50 mL) and phenylephrine and epinephrine boluses were ad- ministered to prevent hypotension.
The intraoperative blood and blood products were transfused according to the measured hemoglobin (Hb) and coagulation pa- rameters. Hb was maintained above 10 g/mL. Fluid warmers and warming blankets were used to maintain normal body tempera- ture.
Strategies for preventing PRS were summarized in Fig. 1 .
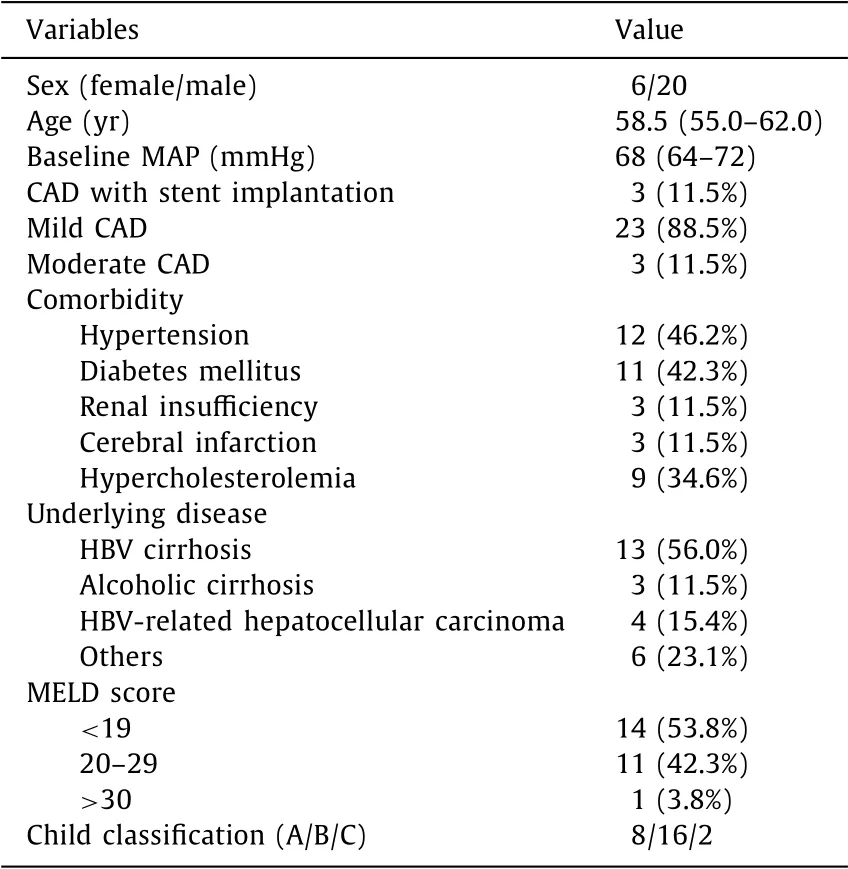
Table 1 Baseline characteristics.
Statistical analysis
The patients’ data were analyzed using SAS release 6.12 (SAS In- stitute, Cary, NC, USA). The values were expressed as either median (interquartile range, IQR) or numbers (percentage).
Results
Patient data
Our study included 26 adult patients. The age, sex, comorbidi- ties, MELD score, Child classification and underling disease of the patients were presented in Table 1 .
Comorbidities included hypertension in 12 patients (46.2%), dia- betes mellitus in 11 (42.3%), hypercholesterolemia in 9 (34.6%), ob- solete cerebral infarction in 3 (11.5%), and mild renal insufficiency in 3 (11.5%). One patient had a temporary pacemaker installed be- fore surgery for bradyarrhythmia.
CAD was recognized in all patients before OLT by a pre- operative cardiac evaluation, including electrocardiogram, echocar- diography (UCG), coronary computed tomographic angiography (CTA), and coronary angiography. All patients had mild to moderate CAD, but only 3 patients (11.5%) with moderate CAD were proved by coronary angiography. Two patients (7.7%) had myocardial in- farction proved by UCG. Four patients (15.4%) had a history of coro- nary angioplasty before OLT. A drug-eluting stent was implanted in the left anterior descending artery in 2 patients and in the right coronary artery in 1 patient about one year prior, and aspirin was continued in all patients. The majority of patients had heart function evaluation by UCG. Twelve patients (46.2%) had varying degrees of left ventricular hypertrophy (LVH); two-dimensional echocardiogram (ECHO) was normal in 5 patients (19.2%), with low ejection fraction (EF) in 3 patients and the lowest EF was 48%. Fourteen patients (53.8%) had moderate diastolic dysfunction.
Intraoperative condition
The details of the intraoperative parameters were presented in Table 2 . PiCCO was used in 23 patients (88.5%). TEE was used in 2 patients (7.7%), and a pulmonary artery catheter and TEE were used in 1 patient (3.8%) due to the severe clinical situation.

Table 2 Intraoperative details.
The duration of surgery ranged from 270 to 414 min with a median of 345.5 min. The duration of the anhepatic stage ranged from 42 to 57 min with a median of 51.5 min. The cold ischemic time ranged from 120 to 458 min with a median of 282.5 min. All patients tolerated the cross clamping the IVC well. ST-segment changes were detected in 12 patients (46.2%) immediately after clamping the IVC, and most patients returned to normal or nearly normal after their blood pressure increased. Two patients had low CI during the anhepatic stage, and CI increased to 2.5 L/min/m2and SVRI decreased after introducing dopamine.
PRS was observed in 13 patients (50%), and 2 (7.7%) of them were severe. Ten patients (38.5%) required epinephrine/ norepinephrine infusion for nearly 30 min, and 5 patients (19.2%) required norepinephrine and dopamine infusion after reperfusion. ST-segment changes were detected in 14 patients (53.8%) imme- diately after reperfusion, and most patients returned to normal within 15 min. Two patients (7.7%) exhibited persistent ST-segment depression (ranging from -1 to -0.5 mm). Two patients (7.7%) re- quired additional nitroglycerin transfusion for the higher CVP.
Intraoperative salvage of blood was employed in 8 patients (30.8%). The blood loss ranged from 600 to 1500 mL with a me- dian of 910 mL. The blood transfusion ranged from 2 to 6 U with a median of 2 U.
Post-operative condition
All patients were admitted to the ICU after the operation. The duration of ventilation ranged from 4 to 12 h with a median of 8 h. The duration of the ICU stay ranged from 2 to 11 days with a median of 4.5 days. The duration of the hospital stay ranged from 8 to 36 days with a median of 13 days.
Six patients (23.1%) had AKI, and 2 patients required dialysis for 2 days. Three patients (11.5%) had AMI (troponin > 0.04 ng/mL), 2 patients experienced heart failure [brain natriuretic peptide (BNP) > 100 pg/mL] but no patients died from a cardiac-related event ( Table 3 ). One patient died 4 months after operation from the se- vere pulmonary infection. The other patients were alive with good cardiac and allograft function at a follow-up (median14 months).
Discussion
The modified piggyback technique is preferred in OLT to re- duce the operative time and the risk of portal vein anastomotic stricture. However, this technique is correlated with cardiovascular instability due to large changes of preload and afterload [10] , which may increase the occurrence of PRS. PRS is a common com- plication after liver reperfusion due to the release of vasoactive mediators from the reperfused liver, which is associated with in- creased complications and mortality [12 , 13] . OLT recipients with CAD or coronary risk factors are prone to an increase of PRS after liver reperfusion [5] . Some reports have suggested that OLT should be performed under veno-venous bypass or partial clamp of the IVC to obtain maximum hemodynamic stability in recipients with CAD [8 , 9] .
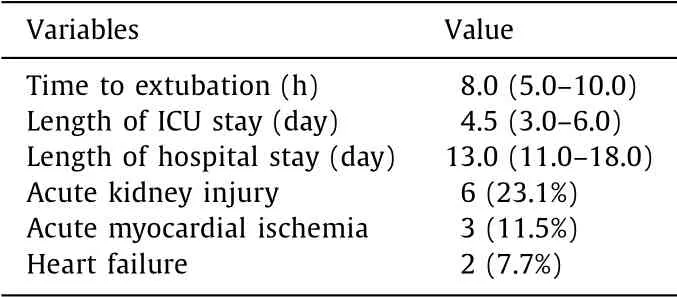
Table 3 Post-operative data.
In 26 ESLD patients with CAD, the patient survival and graft survival were satisfactory. Our data was similar to Skaro’s study in Northwestern Memorial Hospital, Chicago, USA, which found that patients with CAD remained similar survival to patients with- out CAD after liver transplantation [14] . OLT was successfully per- formed with the modified piggyback technique at our center, which might partially contribute to the success of our intraopera- tive management. This protocol was based on our experience with patients undergoing LT or with the reference to the literatures re- lated CAD [8 , 15] . First, the strict management of the hemodynamic parameters through monitoring, fluid transfusion and cardiovascu- lar drug use is required to balance the myocardial oxygen supply and demand. Second, decreasing the occurrence of PRS is key to the management of this special population.
The PiCCO system, which can be used to evaluate cardiovas- cular performance, along with SVV and CI monitoring was in- troduced in the recipients with CAD [10] . Intraoperative TEE al- lows for the real-time detection of myocardial ischemia manifested by regional wall motion abnormalities and is applied in many centers [10] . However, inducing bleeding in esophageal varices is a concern that limits its use at our center.
Perioperative fluid management was aided by CVP and SVV, and the strategy of lowering CVP to decrease bleeding and hepatic congestion, which is related to significant reflex tachycardia [8] , should not be recommended. In our patients, mild strict fluid administration was implemented during the hepatic dissection and anhepatic stages by maintaining the CVP at a relatively high level (6-7 mmHg) or SVV at 13% -20%. It has been reported that the maintenance of a slightly high SVV is effective and safe for reducing blood loss during hepatectomy [16] .
The positive effect of norepinephrine and vasopressin in- fusion on recipient outcomes has been observed during OLT by improving hemodynamic stability and post-operative renal function [7 , 17] . The infusion of vasopressors during the anhepatic phase has been associated with reduced vasoactive drug use to counteract PRS [16] . An adjuvant vasopressor along with controlled fluid therapy can decrease the post-operative tracheal reintubation rate [7] . The proper infusion dose of diltiazem hydrochloride was used to maintain proper coronary blood flow and decrease the risk of AMI. A review indicated that calcium channel blockers repre- sent an important component of triple therapy for patients with stable CAD and are associated with a significant decrease in ma- jor cardiovascular events [18] . In our series, there were no major cardiovascular events during the surgery, but major cardiovascular events that were normalized after treatment were observed in 3 recipients with AMI and 2 recipients with heart failure during the ICU stay.
Recipients with CAD are prone to develop PRS during reperfu- sion. It is very important to attenuate the release of metabolic sub- stances, such as oxygen-derived free radicals, from the reperfused liver into circulation to decrease the occurrence of PRS. There were only two severe cases of PRS (7.7%) occurring after reperfusion in this series, which was lower than the rate reported in previous studies [11 , 19] . Several strategies were introduced to minimize PRS at our center.
First, the portal vein and inferior vena cava were unclamped be- fore starting hepatic artery anastomosis. The anhepatic phase (me- dian 51.5 min) was shorter than that in reported cases [20] . The short anhepatic phase along with rapid hepatectomy can reduce the metabolic substance and significantly improve hemodynamic changes.
Second, the portal vein was flushed to avoid PRS in the patients with CAD. This technique decreases the risk of PRS by reducing the release of inflammatory cytokines from the grafted liver into circu- lation immediately after portal vein decamping [21] . Furthermore, flushing the portal vein can reduce the risk of fluid overload after IVC unclamping as a high filling pressure and severe hypotension are correlated with progressive cardiac ischemic and other severe cardiac events.
Finally, mannitol was slowly infused during the dissection phase and anhepatic phase to attenuate blood loss and PRS. It has been shown that mannitol administration and fluid restriction are effective strategies for reducing blood loss during living donor hepatectomy [16] , and the infusion of mannitol during the anhep- atic phase is effective in attenuating PRS [22] . Mannitol is a free radical scavenger that protects against ischemia-reperfusion injury; furthermore, mannitol is an osmotic diuretic that decreases vascu- lar congestion within the surgical field [22] .
In conclusion, OLT with the modified piggyback technique can successfully be performed in ESLD patients with mild and mod- erate CAD. A thorough evaluation and optimization of recipi- ents, strict monitoring and optimized management of circulation, knowledge of the complicated changes during OLT procedures, and strategies to ameliorate PRS can help achieve a favorable outcome.
CRediT authorship contribution statement
Hai-Ying Kong:Conceptualization, Supervision, Writing - orig- inal draft, Writing - review & editing.Xian Zhao:Data curation, Formal analysis.Kui-Rong Wang:Writing - review & editing.
Funding
None.
Ethical approval
This study was approved by the Ethics Committee of the First Affiliated Hospital, Zhejiang University School of Medicine.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or in directly to the sub- ject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Impact of EBV infection and immune function assay for lymphoproliferative disorder in pediatric patients after liver transplantation: A single-center experience
- Hepatobiliary&Pancreatic Diseases International
- Acute onset of autoimmune hepatitis in children and adolescents
- Liver stiffness as a predictor of hepatocellular carcinoma behavior in patients with hepatitis C related liver cirrhosis ✩
- Treatment and prognosis of hepatic epithelioid hemangioendothelioma based on SEER data analysis from 1973 to 2014
- Cholecystoenteric fistula with and without gallstone ileus: A case series